Postoperative pulmonary complications in severe acute respiratory syndrome coronavirus 2 infected patients who underwent emergency surgery
Abstract
Background
Recent studies suggest that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection increases the incidence of postoperative pulmonary complications (PPCs) and mortality. Consequently, patients with SARS-CoV-2 infection undergoing emergency surgery are more vulnerable to PPCs, yet few studies have evaluated PPCs in these patients.
Methods
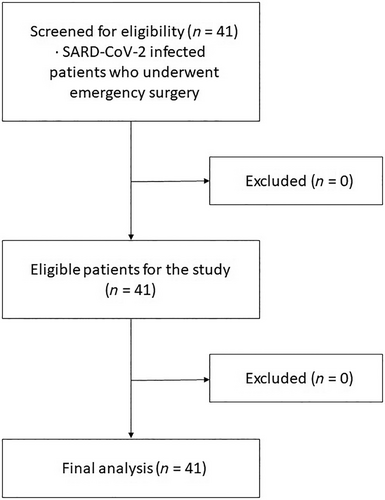
A retrospective analysis was conducted between January 2022 and February 2023 on the medical records of patients infected with SARS-CoV-2 who underwent emergency surgery. The study evaluated the incidence of PPCs and 30-day postoperative mortality in all enrolled patients.
Results
A total of 41 patients were enrolled, among whom PPCs occurred in seven patients (17%). The incidence of PPCs was statistically significant in patients with underlying diabetes compared to those without (p = 0.01) and in patients with an American Society of Anesthesiologists (ASA) class 3 or higher compared to those with less than 3 (p = 0.005) (ASA classification uses a grading system of I (one) through V (five)). The 30-day mortality rate was 4.9%.
Conclusions
Our study demonstrates that the incidence of PPCs and 30-day mortality rates after emergency surgery in patients infected with SARS-CoV-2 are higher compared to prepandemic baseline rates. Given the significant interest and concern worldwide regarding severe infectious respiratory diseases, such as coronavirus disease 2019 (COVID-19), clinicians should focus on conducting research to identify ways to reduce the incidence of PPCs and mortality in patients with severe acute respiratory infections.
INTRODUCTION
Postoperative pulmonary complications (PPCs) are a frequent perioperative adverse event associated with increased morbidity, mortality, delayed recovery, longer hospital stays, and higher cost of care, with reported frequencies ranging from 2% to 70%, due to differing definitions of PPCs used in various studies.1-3
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has affected all aspects of society, and hospitals have reallocated resources and postponed/canceled elective surgeries in infected patients to protect healthcare workers and reduce transmission risk.4, 5 Recent studies suggest that SARS-CoV-2 infection increases the incidence of PPCs and mortality.6, 7 Consequently, patients with SARS-CoV-2 infection undergoing emergency surgery are more vulnerable to PPCs, yet few studies have evaluated PPCs in these patients. Therefore, the major goal of this study was to investigate the incidence of PPCs and 30-day mortality in SARS-CoV-2 infected patients who underwent emergency surgery.
METHODS
This study was a retrospective analysis of medical records of patients with SARS-CoV-2 infection who underwent emergency surgery under general or regional anesthesia between January 2022 and February 2023, approved by the Institutional Review Board and the written informed consent was waived due to the nature of the study. This study was performed in accordance with the tenets of the Declaration of Helsinki-2013.
The diagnosis of SARS-CoV-2 infection was confirmed by real-time reverse transcription polymerase chain reaction (RT-PCR) testing of material from nasal and pharyngeal swabs, taken within 7 days before surgery. Clinical symptoms at emergency admissions were as follows: cough, dyspnea, abdominal pain, fever ≥38°C, sore throat, nausea or vomiting, sputum, fatigue, diarrhea, and myalgia. The PPCs were as follows: pneumonia, atelectasis, bronchospasm, respiratory failure, and/or unexpected postoperative ventilation.8 Only the first PPCs occurring in any one patient were analyzed. Thirty-day mortality was defined as death occurring within 30 days after surgery. The PPCs and 30-day mortality were assessed.
Anesthesia included general anesthesia and regional (spinal) anesthesia. General anesthesia was achieved with propofol (1–2 mg/kg) and rocuronium (0.5–1.2 mg/kg) followed by tracheal intubation. Anesthesia was maintained with inhaled sevoflurane (1%–2%) or desflurane (3%–7%). Mechanical ventilation was kept to maintain the end-tidal carbon dioxide at 30–40 mmHg throughout the surgery. Spinal anesthesia was established via the L4–5 or L3–4 interspace. After free flow of cerebrospinal fluid was confirmed, 0.5% hyperbaric bupivacaine was injected into the intrathecal space. If sedation was required during surgery, midazolam, propofol, or dexmedetomidine were administered intravenously. American Society of Anesthesiologists physical status (ASA-PS) classification at the time of surgery was analyzed as grades 1–2 versus grades 3–5. The ASA-PS score, which represents patients requiring emergency surgery, also consists of an ASA-PS grade plus an “E”.9 Emergency surgery was defined as procedures classified by the National Confidential Enquiry into Patient Outcome and Deaths as immediate, urgent, or expedited.10 The exclusion criteria included insufficient medical records and being under 18 years of age.
Statistical analysis
Statistical analysis was conducted using Stata 14.1 (Stata Corporation). The results are expressed as the mean (range) or number of patients (percentage). Mann–Whitney U test was used for continuous variables, while Pearson's chi-square test or Fisher's exact test was used for categorical variables. A p-value <0.05 was considered statistically significant.
RESULTS
A total of 41 patients were included in the study, consisting of 19 males (46.3%) and 22 females (53.7%) with a mean age of 62 years (range 50–72 years). Of these, 35 patients (85.4%) had no clinical symptoms on admission, while six patients (14.6%) had symptoms. The types of clinical symptoms in six patients were cough in one patient, fever in two patients, fever and sore throat in two patients, and myalgia in one patient. General anesthesia was performed on 34 patients and regional anesthesia on seven patients. The average duration of anesthesia was 115 min, with mean anesthesia time of 128 min for patients who experienced PPCs and 112 min for patients who did not develop PPCs. Surgical diagnoses included benign disease in 19 patients (46.3%), cancer in four patients (9.8%), and trauma in 18 patients (43.9%). The types of emergency surgeries included 18 severe trauma cases, three cardiac emergencies, two neurological diseases, 15 abdominal diseases (2 perforated ulcers, 5 appendicitis, 4 acute cholecystitis, 2 intestinal obstruction, 2 intestinal perforation), and three cesarean sections. Out of the patients, 39 patients had received the COVID-9 vaccine, while two patients had not received the vaccine. The patients who did not receive the vaccine were pregnant women who underwent emergency cesarean section. Within 30 days, seven patients (17%) developed PPCs, including two patients with pneumonia, one patient with atelectasis, one patient with bronchospasm, and three patients with respiratory failure.
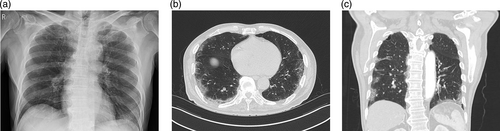
The incidence of PPCs was significantly higher in patients with diabetes as underlying disease (p = 0.01) and ASA CLASS 3E or more (p = 0.005). The 30-day mortality rate was 4.9% (2 of 41), both of whom were male patients aged 70 and 78 years with preoperative clinical symptoms, suspected COVID pneumonia on preoperative chest CT, and PPCs following exploratory laparotomy for acute abdominal pain. The causes of death were respiratory failure and multiple organ failure, and the patients died on day 7 and day 15, respectively. Details are presented in Table 1, and Figures 1 and 2.
| Variables | Population | No PPC (n = 34) | PPC (n = 7) | p-value |
|---|---|---|---|---|
| Age (yr), mean (ranges) | 62 (50–72) | 61 (46–72) | 64 (60–78) | 0.488 |
| Sex | >0.999 | |||
| M | 19 (46.3) | 16 (47.1) | 3 (42.9) | |
| F | 22 (53.7) | 18 (52.9) | 4 (57.1) | |
| Anesthesia | 0.243 | |||
| General | 34 (82.9) | 28 (82.4) | 6 (85.7) | |
| Regional | 7 (17.1) | 6 (17.7) | 1 (14.3) | |
| Vaccination | – | |||
| No | 2 (4.9) | 2 (5.9) | 0 (0.0) | |
| Yes | 39 (95.1) | 32 (94.1) | 7 (100.0) | |
| Hb (g/dL) | 12.8 | 12.9 | 12.4 | 0.51 |
| CRP (mg/L) | 7.75 | 5.4 | 46.8 | 0.72 |
| PLT (103/uL) | 228 | 228 | 231 | 0.268 |
| Symptoms at admission | 0.268 | |||
| No | 35 (85.4) | 30 (88.2) | 5 (71.4) | |
| Yes | 6 (14.6) | 4 (11.8) | 2 (28.6) | |
| Underlying diseases | 0.39 | |||
| No | 26 (63.4) | 23 (67.7) | 3 (42.9) | |
| Yes | 15 (36.6) | 11 (32.4) | 4 (57.1) | |
| Pulmonary disease | 3 (7.3) | 2 (5.9) | 1 (14.3) | 0.439 |
| CVD | 4 (9.8) | 2 (5.9) | 2 (28.6) | 0.128 |
| Hypertension | 12 (29.3) | 9 (26.5) | 3 (42.9) | 0.398 |
| DM | 7 (17.1) | 3 (8.8) | 4 (57.1) | 0.01 |
| ASA PS | 0.005 | |||
| ≤2 | 20 (48.8) | 20 (58.8) | 0 (0.00) | |
| ≥3 | 21 (51.2) | 14 (41.2) | 7 (100.0) |
- Note: Values are presented as mean (ranges) or number of patients (%).
- Abbreviations: ASA PS, American Society of Anesthesiologists physical status; CVD, cardiovascular disease; DM, diabetes; PPC, postoperative pulmonary complication.
DISCUSSION
In the present study, we assessed the occurrence of PPCs and postoperative mortality in patients infected with SARS-CoV-2 who underwent emergency surgery, and we found that the PPCs rate was 17% and the 30-day mortality rate was 4.9%. It should be noted that patients undergoing emergency surgery have an increased risk of developing PPCs,1, 2 particularly if they have had a recent acute respiratory infection, and most anesthesiologists recommend waiting 3–4 weeks before performing surgery on patients with upper respiratory infections.1-3, 8
The incidence rate of PPCs in COVID-19 patients compared to those with other infectious respiratory diseases is difficult to determine due to limited research, but severe acute respiratory diseases like COVID-19 increase the risk of developing PPCs. Previous studies have shown that SARS-CoV-2 positive patients have a greater number and severity of postoperative complications, with PPCs being more prevalent in these patients.6, 7, 11 While an international and multicenter study11 reported a 51.3% PPCs rate after emergency surgery in SARS-CoV-2 infected patients, our study found a lower rate of 17%, which may be attributed to the small sample size and the accumulated experience of the medical system in responding to the pandemic. Chandler et al.12 reported an incidence rate of PPCs ranging from 2% to 5.6% in the general surgical population and from 20% to 70% in upper abdomen and thoracic surgery. Anesthesiologists have recommended waiting 3–4 weeks before performing surgery in patients with upper respiratory infection, which has been listed as a predictor of PPCs.
Diabetes is known to be linked with immune dysfunction, which increases susceptibility to infections.13 MoriKane et al.14 reported that diabetes is a predisposing factor for developing pulmonary complications after surgery. Similarly, our study found that the incidence of PPCs was significantly higher in patients with underlying diabetes compared to those without diabetes (p = 0.01).
The ASA-PS classification system has undergone revisions since its introduction in 1941 and is widely used by anesthesiologists to assess a patient's overall health.9 Recently, it has been considered an independent predictor of postoperative complications and mortality.15 Foley et al.16 reported that medical complication or mortality occurred with a much higher frequency in higher ASA PSE class patients than in lower ASA PSE class patients, and the COVIDSurg Collaborative reported that the only independent predictor factor of 30-day pulmonary complications was ASA grades 3–5 in patients infected with SARS-CoV-2 who underwent surgery in 24 countries.6 In our study, the incidence of PPCs was found to be statistically significantly higher in ASAs 3-5E than in ASAs 1-2E (p = 0.005), similar to the previous report.6
In cases where emergency surgery is required for patients with pre-existing respiratory infections or risk factors for PPCs, it is important to implement perioperative strategies to minimize the risk of PPCs, such as preoperative optimization of lung function, careful fluid management, use of regional anesthesia techniques, early mobilization after surgery, and early initiation of pulmonary rehabilitation, as well as close monitoring and prompt management of any respiratory complications that may arise.13, 17 For COVID-19 patients, regional anesthesia is strongly advocated to prevent aerosolization and transmission of the virus while preserving respiratory function. In this study, out of seven patients who underwent emergency surgery under regional anesthesia, only one patient (a 67-year-old woman with diabetes, hypertension, and malignancy who underwent femur fixation) developed PPCs.
In a previous study, it was observed that patients who had been infected with SARS-CoV-2 before surgery had a significantly higher risk of 30-day mortality after surgery compared to those who were not infected with the virus.11 This increased risk of death may be attributed to the adverse respiratory and cardiovascular effects of the SARS-CoV-2 virus, which is thought to cause lung damage due to an overactive immune response of the host along with microvascular pulmonary thrombosis.18-20 Surgery may further contribute to proinflammatory conditions and facilitate these pathways.21-23
A systematic review and meta-analysis conducted by Brown et al.24 evaluated the mortality of patients with COVID-19 who underwent elective or emergency surgery, with a mortality rate of 7.9% in emergency surgical patients. In comparison, our study found a lower mortality rate of 4.9%. This difference in mortality rates may be attributed to differences in the timing of patient recruitment, as the previous study included patients from the early stage of the COVID-19 pandemic, while our study included patients who underwent vaccination after the outbreak of the pandemic. Moreover, differences in disease severity may have also contributed to this variation. In our study, two out of 41 patients died after surgery due to respiratory failure and multiple organ failure, which were presumed to be caused by adverse effects of the SARS-CoV-2 virus.
The present study had several limitations that need to be acknowledged. First, it was a retrospective study with a relatively small sample size. Given that, during the early days of the COVID-19 pandemic, treatment of infected patients in Korea was centralized to designated hospitals, and our study was limited to patients treated at a single center. Therefore, a larger-scale multicenter study is required to confirm our findings. Second, some patients who were asymptomatic were diagnosed through testing at the time of admission, and this may have resulted in delayed diagnosis for some patients.
In conclusion, our study demonstrates that SARS-CoV-2 infected patients undergoing emergency surgery are at higher risk for PPCs and 30-day mortality compared to prepandemic rates. Notably, the presence of diabetes as an underlying disease and an ASA CLASS 3-5E are significant risk factors for PPCs. Given the global concern and interest in infectious respiratory diseases due to COVID-19, it is imperative for clinicians to focus on research aimed at reducing the incidence of PPCs and mortality rates in patients with severe acute respiratory infections.
AUTHOR CONTRIBUTIONS
MO designed the research study. MO and SB performed the research. MO and SB analyzed the data. MO and SB wrote the manuscript. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST STATEMENT
The authors declare no competing interests.