Solitary extramedullary plasmacytoma of the left main bronchus: A case report and literature review
Funding information: National Natural Science Foundation of China, Grant/Award Numbers: 81900197, 82273019; Tianjin Natural Science Foundation, Grant/Award Number: 18JCYBJC92100; Key Project of Cancer Foundation of China, Grant/Award Number: CFC2020kyxm003; Tianjin Key Medical Discipline (Specialty) Construction Project, Grant/Award Number: TJYXZDXK-061B; General Project of Tianjin Lung Cancer Institute, Grant/Award Number: TJLCMS2021-03; Science and Technology Program of Sichuan Province, Grant/Award Number: 2020YJ0104; Chongqing NSF project, Grant/Award Number: cstc2021jcyi-msxm4159
Abstract
Tracheal tumors are rare, accounting for 0.1% of all malignancies. Squamous cell carcinoma and adenoid cystic carcinoma are the two most prevalent tracheal cancers. Less than 20 cases of extramedullary plasmacytoma in the trachea and main bronchus have ever been documented in the literature, making it extremely uncommon. Although the origin of these lesions is unclear, viral pathogenesis and persistent inflammation are thought to be the main causes. Clinically, these individuals exhibit vague symptoms such as stridor, a persistent cough, dyspnea, or wheezing, making a correct diagnosis difficult.
INTRODUCTION
Plasma cell neoplasms are characterized by the uncontrolled proliferation of a single clone of plasma cells that produce monoclonal immunoglobulins. They may manifest as either a single tumor (plasmacytoma) or several tumors (multiple myeloma). Plasmacytomas of bone are typically isolated tumors that originate in the bone. The term extramedullary plasmacytoma is used to describe lesions that originate outside of the bone. More than 80% of extramedullary plasmacytoma cases occur in the head and neck, with the nasal cavity, and oronasopharynx being the most common sites.1 Extramedullary plasmacytomas of the larynx, thyroid, parotid gland, and middle ear are uncommon. Bronchus and lung parenchyma are quite uncommon.2
CASE REPORT
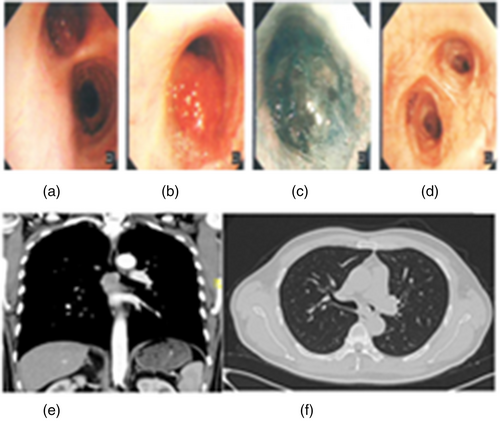
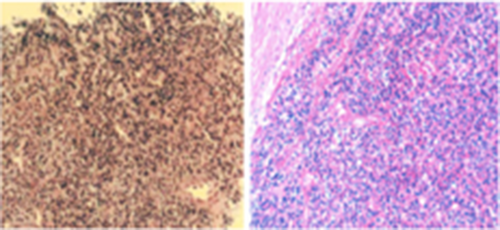
A 50-year-old male patient with no smoking history visited a doctor at our hospital with a history of intermittent dyspnea and cough. Fiberoptic bronchoscopy indicated the presence of a new papillary organism on the inner surface of the left main bronchus. The upper edge of the new organism was 5 mm below the carina, the surface was congested and swollen, and the lower edge was 20 mm from the upper and lower lobe bronchial openings of the left lung (Figure 1a–d). On a chest computed tomography (CT) scan, a soft tissue density shadow was observed in the left main branch air duct cavity. After enhancement, it had visibly and consistently increased to a size of approximately 2.1 × 1.7 cm (Figure 1e,f). Pathological and immunohistochemical findings of fiberoptic bronchoscopic biopsy were as follows: medium-sized plasma cell-like infiltration with consistent morphology; CD138 (+), CD38 (+), CD79a (+), kappa (+), lamda (−), MUM-1 (+), Ki67 (3%)+, CD 20 (+); and CD 56 (−), CD 3 (−) (Figure 2). The pathology report suggested a tumor composed of plasma cells. After negative results for lactic dehydrogenase, microspherin, serum protein electrophoresis, and bone marrow biopsy, the patient was diagnosed with extramedullary plasmacytoma.
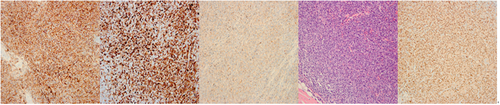
The patient had a left main bronchus tumor resection and carina repair after accomplishment of all essential examinations. During the operation, the tumor in the left main bronchus measured approximately 2.0 cm in diameter, its proximal end was approximately 0.5 cm from the carina, its distal end was approximately 2.0 cm from the opening of the upper and lower lobe bronchus of the left lung, and the lymph node under the carina measured approximately 2 cm in diameter. The operation was successful. The findings of postoperative pathology indicated a bronchial segment measuring 3.0 cm in length and 2.3 cm in diameter. On the bronchial mucosa, a tumor measuring approximately 1.8 × 1.5 × 1.4 cm and involving the whole layer of the tube wall was detected. Microscopically, there was evidence of extensive plasma cell proliferation and infiltration, with different degrees of differentiation. The majority of cells were of uniform sizes. The nucleus was frequently biased. Karyokinesis was uncommon and the chromatin in the nucleus was spoke-shaped. Immunohistochemistry determined CD79a (+), CD138 (+), CD38 (+), PCK (−), CD 20 (−), PAX5 (−), CD 3 (−), CD 56 (−), CD 30 (−), lamda (+), mum-1 (+), Ki67 (3%+), CD 5 (−), CD10 (−), WT-1 (−), S-100 (−), SynA (−), and cyclin D1 (−) (Figure 3). There was no evidence of cancer in lymph node groups 3–10. IgH and IgK clonal amplification peaks were found by in situ hybridization as part of an EBER1/2 (−) gene rearrangement investigation. During a mutation analysis, it was determined that exon 5 of the MYD88 gene was not mutated. The tumor was identified as an extramedullary plasmacytoma using a combination of clinical and further diagnostics. The patient recovered well from surgery without radiotherapy and was monitored regularly. No recurrence or metastasis has been identified since 20 months ago.
DISCUSSION
Solitary extramedullary plasmacytoma of the bronchus is extremely uncommon. According to the literature, this tumor has been found to occur between the ages of 15 and 69, as well as in individuals older than 40.3 Additionally, as a result of its origin and location, it is typically associated with airway obstruction or irritation, such as cough, shortness of breath, or dyspnea. However, some individuals exhibit no symptoms and may therefore be mistakenly diagnosed with bronchial asthma due to the existence of symptoms that are similar to those of bronchial asthma.
Radiotherapy and/or surgery are the most frequent treatments. We believe surgery is an effective treatment for extramedullary plasmacytoma of the trachea or bronchi. However, radical resection can be difficult if the tumor has spread to a large area or to neighboring essential organs. Due to the rarity of tracheobronchial extramedullary plasmacytoma, however, there is little evidence to evaluate if the combination of radiotherapy and surgery can boost the survival rate of patients. The size of the original tumor and lymph node metastases are two independent poor prognostic factors that affect patient survival.4 In our case, the patient's tumor was located in the left main bronchus, with its upper edge just 5 mm from the carina and its lower edge 20 mm from the opening of the left lung's upper and lower lobe bronchus. The patient recovered well after surgery. He avoided microbial and fungal diseases and did not receive radiation treatment. During the 20-month follow-up period, no recurrence or metastasis was seen.
Plasmacytoma must often be differentiated pathologically from poorly differentiated bronchial squamous cell carcinoma. The latter is polyclonal and has cancer cells with obvious pleomorphism and atypia, a nest-like distribution, and no plasma cell differentiation. Additionally, it is frequently necessary to pathologically differentiate plasmacytoma from plasma cell granuloma. In plasmacytomas, monoclonal expression is typically seen.
In conclusion, the predominant symptom of plasmacytoma is obstruction of the respiratory tract. Early identification is difficult, and it is easy to be misdiagnosed and missed. A surgical operation can remove the tumor entirely and relieve symptoms while also providing a precise pathology diagnosis that can aid treatment. In addition, long-term follow-up is recommended.
AUTHOR CONTRIBUTIONS
Limin Gao analyzed data and wrote the paper; Xinyun Wang revised the manuscript; Wang Shen and Huifang Li revised the pathology analysis; Cheng Ai and Xuebing Li collected literatures.
ACKNOWLEDGMENTS
This study was supported by grants from the National Natural Science Foundation of China (no. 82273019, to Xuebing Li), Tianjin Natural Science Foundation (no. 18JCYBJC92100, to Xuebing Li), the Key Project of Cancer Foundation of China (no. CFC2020kyxm003, to Xuebing Li), the Tianjin Key Medical Discipline (Specialty) Construction Project (no. TJYXZDXK-061B)-General Project of Tianjin Lung Cancer Institute (no. TJLCMS2021-03, to Xuebing Li); the National Natural Science Foundation of China (81900197) and Science and Technology Program of Sichuan Province (2020YJ0104); Chongqing NSF project (cstc2021jcyi-msxm4159).
CONFLICT OF INTEREST
No authors report any conflict of interest in this work.