Radiation-induced pseudomembranous tracheobronchitis: A report of two cases
Abstract
Radiation therapy can cause radiation pneumonitis, organizing pneumonia, and lung fibrosis. Radiation-induced pseudomembranous bronchitis is a rare condition. Here, we describe a rare case each of pseudomembranous tracheobronchitis and pseudomembrane with total bronchial obstruction which developed after thoracic radiotherapy. A 50-year-old man presented paroxysmal severe cough 1 month after concurrent chemoradiotherapy for small-cell lung cancer. Bronchoscopy revealed a whitish membrane in the trachea and bronchus, which were the fields of radiation. Another 60-year-old man complained of dyspnea 7 months after radiation therapy for metastatic lymph node adenocarcinoma. Bronchoscopy demonstrated a membrane with total obstruction of right lower lobar bronchus, which was the area of radiation. The pathological findings of histological examination in both cases demonstrated radiation-induced pseudomembranous tracheobronchitis. Patients in both cases responded well to steroids and the pseudomembrane disappeared. If patients who have received thoracic radiation therapy complain of persistent cough, bronchoscopy may be helpful.
INTRODUCTION
Radiation therapy is one of the treatment modalities for lung cancer. However, the effects of radiation are not specific to cancer cells but also affect normal cells. Thoracic radiotherapy may induce lung injuries, mainly radiation-induced pneumonitis, radiation-induced lung fibrosis, radiation-induced bronchiolitis obliterans organizing pneumonia,1, 2 and radiation-induced bronchitis.3, 4 We report two rare cases of radiation-induced pseudomembranous tracheobronchitis with or without bronchial obstruction in lung cancer patients.
CASE REPORT
Case 1
A 50-year-old man presented with worsening cough in August 2019. He had a history of pulmonary tuberculosis 30 years ago. He had a smoking history of 45 pack years and had quit smoking 3 years ago. He also had chronic obstructive pulmonary disease (COPD), which was treated with long-acting inhaled bronchodilators. He was diagnosed with small-cell lung cancer of limited stage of the right upper lobe (RUL) and right hilar and mediastinal lymph nodes (LNs) in May 2019. He had been treated with chemotherapy of etoposide and cisplatin every 3 weeks for four cycles. He had also been treated with concurrent radiation therapy of a daily 220-cGy dose, with a total 66-Gy dose from June 5, 2019, to July 17, 2019.
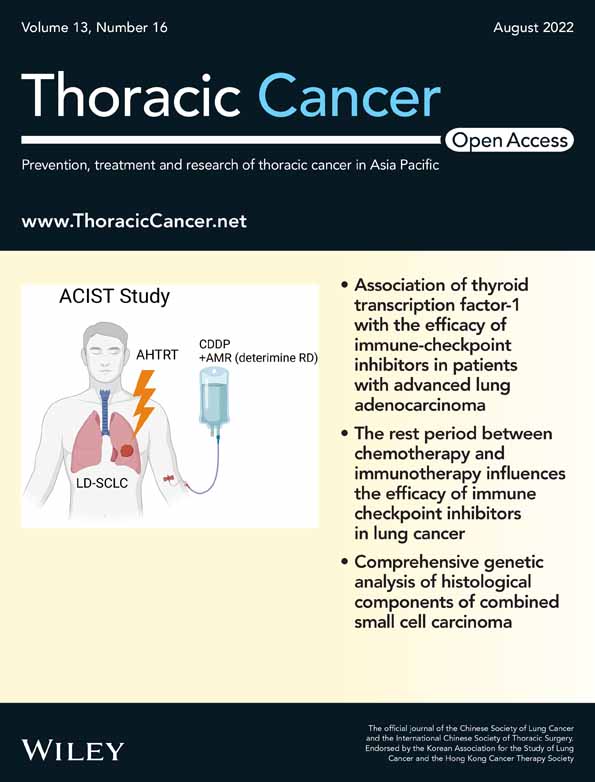
During radiation therapy, his dry cough began and got worse. The cough did not improve even with codeine, sedatives, or narcotic pain relievers. One month after completion of radiation therapy, chest X-ray showed new consolidation on the right upper lung field. We performed a chest computed tomography (CT) scan, and it revealed radiation pneumonitis and a thickened airway wall (Figure 1a). The bronchoscopy showed mucosal edema and diffuse whitish plaques with membrane formation in the trachea and main bronchus (Figure 1b). To exclude a microbiologic cause, we tried to do a biopsy of the membrane of trachea using forceps. Two days later, follow-up bronchoscopy showed a more aggravated whitish patch with membrane formation to the anterior wall of the trachea (Figure 1c). Pathologic findings of membrane showed necrotic fibrin and inflammatory cells (Figure 1d). According to these findings, we diagnosed pseudomembranous tracheitis and bronchitis. We started prednisolone 50 mg/day. After 3 days of steroid administration, the whitish patch had improved on the follow-up bronchoscopy (Figure 1e). After 40 days of steroid administration, the whitish patch disappeared (Figure 1f) and the steroid was tapered after 3 months of use. After 7 months, there was no pseudomembrane in the bronchoscopy findings (Figure 1g).
Case 2
A 60-year-old man presented with worsening cough in February 2022. He had a smoking history of 15 pack years and had quit smoking 6 years ago. He had COPD treated with inhaled long-acting bronchodilators. He was diagnosed with adenocarcinoma of the RUL of stage IB and had undergone RUL posterior segmentectomy on February 2019. In April 2021, metastatic left interlobar LN developed, and a fractional stereotactic radiosurgery of 17 Gy daily, three times with a total dose of 51 Gy for metastatic left interlobar LN was performed. Chemotherapy was done 4 cycles, every 3 weeks of pemetrexed and cisplatin chemotherapy were administered, and then a monotherapy of pemetrexed was maintained every 3 weeks. Radiation pneumonitis developed in September 2021 and was treated with oral prednisolone 30 mg/day from September 2021, which was tapered in January 2022.
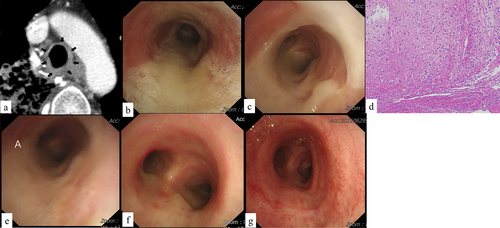
After stopping prednisolone, a dry cough developed. We performed chest CT scan for surveillance of lung cancer. The chest CT scan and chest X-ray (Figure 2a) revealed fibrotic changes of previously treated radiation pneumonitis on the right middle lobe and right lower lobe (RLL) without new lesions. Despite the administration of antitussive drugs, the cough worsened. Three days later, dyspnea developed and the follow-up chest X-ray (Figure 2b) showed new atelectasis in the right lower lung field compared to previous chest X-ray (Figure 2a). We performed bronchoscopy and it showed whitish membrane (Figure 2c) with total obstruction of the RLL lobar bronchus (Figure 2d). We removed the whitish membrane of the RLL bronchus and the obstructed RLL bronchus reopened (Figure 2e). Pathologic findings of the whitish membrane revealed fibrin clot and inflammatory exudate without evidence of malignancy or infection (Figure 2f). On the basis of all these findings, we finally made a diagnosis of pseudomembranous bronchitis with bronchial obstruction after radiation therapy. We restarted prednisolone therapy 30 mg/day for pseudomembranous bronchitis. The pseudomembrane disappeared and the bronchial obstruction also improved on follow-up bronchoscopy.
DISCUSSION
Risk factors for radiation lung injuries are age older than 65, female, nonsmoker, poor performance status, higher radiation dose, sequential chemoradiation therapy, and COPD.5 Case 1 and 2 patients both had COPD but were younger than 65 years. Radiation-induced lung injuries mainly include radiation pneumonitis, lung fibrosis, and organizing pneumonia.6, 7 Radiation bronchitis with stenosis or granulation was reported in lung cancer patients, but they had received brachytherapy3, 4 or combined external-beam and high dose-rate iridium brachytherapy.8 Radiation bronchitis was reported in esophageal cancer patients who had a total 68.4 Gy dose.9
Pseudomembranous tracheobronchitis is a rare condition that shows a pseudomembrane in the airway. The exact pathogenesis and pathology of the pseudomembrane formation in the airway has not been clarified. Presumed mechanisms are radiation-induced injury of epithelial and endothelial cells, and exudation.7 Pseudomembranous tracheobronchitis due to unknown cause with severe bronchial obstruction,10 Aspergillus,11-14 or Mycoplasma pneumoniae15 have been reported. However, there are no reports about radiation-induced pseudomembranous tracheobronchitis or pseudomembrane with bronchial obstruction in lung cancer patients. The case 1 patient developed radiation pneumonitis and pseudomembranous tracheobronchitis 1 month after radiation therapy. The pseudomembrane was observed in the trachea and the bronchus exposed to radiation and became thicker. Although the optimal corticosteroid types, dosage, and duration have not been evaluated prospectively,5 radiation lung injuries usually improve and recover quickly with corticosteroid treatment.5 We started prednisolone 1 mg/kg because the pseudomembrane was severe and the patient could not sleep due to severe frequent paroxysmal cough. The case 2 patient was initially diagnosed with radiation pneumonitis after stereotactic radiotherapy and was treated with prednisolone 0.5 mg/kg for 3 months. One month after stopping prednisolone, the patient developed sudden bronchial obstruction due to pseudomembrane. To the best of our knowledge, this is the first report of airway obstruction caused by pseudomembranous bronchitis after radiation therapy in a lung cancer patient. In this report, the patients were former smokers and had COPD. On the contrary, Pezzuto et al. reported that smoking cessation notably improved pulmonary functional parameters.16 Condoluci et al. reported that nonsmokers showed better outcomes of radiation therapy compared to smokers.17 Cihanbeylerden et al. reported no relationship between pulmonary function and survival in patients with operable lung cancer.18 The risk factors for pseudomembranous tracheobronchitis after radiation therapy are not yet known. We suggest that smoking or COPD might be related to the development of pseudomembrane in the airway after radiation therapy. Usually, lung injury by stereotactic radiotherapy is lower than for conventional radiation therapy. In the case 2 patient, what might have caused the pseudomembrane in the targeted area with obstruction? It might be the host factor such as smoking history or immune mechanism. However, there is no clarified evidence. Targeted stereotactic radiotherapy can also form a pseudomembrane, especially if the target was close to the bronchus. We need to consider pseudomembrane formation when a patient complains of respiratory symptoms. Just as we did to find the exact cause and mechanism, we did not know how to prevent it. Further studies will be needed.
Pseudomembranous tracheobronchitis usually does not manifest on chest X-ray, except in cases with obstruction or pneumonitis. When a patient presents with cough after radiation therapy, a first chest X-ray will be needed to exclude radiation pneumonitis. In such cases, we tried to use antitussive drugs because the chest X-ray did not show new lesions. If cough persists after radiation therapy in lung cancer patients or the chest CT scan does not reveal progression of lung cancer or radiation pneumonitis, we should perform bronchoscopy though chest X-ray.
In conclusion, we reported two rare cases of radiation-induced pseudomembranous tracheobronchitis and bronchial obstruction due to pseudomembrane in lung cancer patients, and they responded well to steroids. If thoracic radiation-treated patients have persistent cough, bronchoscopy may be helpful.
AUTHOR CONTRIBUTIONS
Hye Sook Choi: conceptualization, data curation, investigation, supervision, visualization, writing-original draft preparation, and writing – review and editing.
ACKNOWLEDGMENTS
The author has no funding.
CONFLICT OF INTEREST
The authors declare that they do not have any conflict of interest.