Heterogeneous tumor-immune microenvironments between primary and metastatic carcinoid tumors differentially respond to anti-PD-L1 antibody therapy
Abstract
A pulmonary carcinoid tumor is a rare tumor that lacks a validated therapeutic approach for unresectable disease. Understanding the intersite tumor-immune heterogeneity is essential to harness the immune system for cancer therapy. However, little is known about the tumor-immune microenvironment (TIME). Here, we describe a patient who had heterogeneous TIME between primary and metastatic carcinoid tumors which differentially responded to chemoimmunotherapy. A 72-year-old man was diagnosed with an advanced pulmonary carcinoid tumor. CT-guided biopsies of lung and scapular tumors confirmed typical carcinoid (PD-L1, 1%–24%) and atypical carcinoid tumors (PD-L1, negative), respectively. Although the primary lung carcinoid tumor showed a partial response, the scapular tumor was significantly enlarged after two cycles of anti-PD-L1 antibody therapy in combination with carboplatin plus etoposide. We performed quantitative pathology imaging analysis with fluorescent multiplex immunohistochemistry. CD8+ T cell infiltration was detected in the PD-L1-positive primary lung tumor nest; however, it was mostly restrained in the stroma in a PD-L1-negative metastatic scapular tumor. Treg infiltrations into both tumor nests and stroma were detected in the lung tumor, which were not detected in the metastatic scapular tumor. This study provides the first evidence of coexistence of heterogeneous TIME within a single individual with a pulmonary carcinoid tumor. This study may provide new insights into the mechanism of primary resistance to chemoimmunotherapy in pulmonary carcinoid tumors.
Introduction
Typical and atypical carcinoids are classified as highly differentiated malignant neuroendocrine tumors (NET).1 Due to their rarity, pulmonary carcinoids lack a validated therapeutic approach for unresectable disease.2, 3 Therefore, development of new therapeutic options is urgently needed.
Although immune checkpoint inhibitors (ICIs) have revolutionized the treatment of non-small cell lung cancer (NSCLC), their impact on small cell lung cancer, which is in the same spectrum with typical and atypical carcinoids, is limited.4, 5 Drug development of immunotherapy targeting pulmonary NET including carcinoids is ongoing.1, 3, 6 However, there is only very limited evidence for immunotherapy in patients with pulmonary carcinoids, with early trials suggesting a low-level activity in patients treated with single agent therapy,3, 6 highlighting the importance of investigating the heterogeneity of tumor-immune microenvironments (TIME) in carcinoids.
TIME have an influence on tumor initiation and response to therapy.7-9 Thus, understanding the intersite tumor-immune heterogeneity is essential to harness the immune system for cancer therapy. However, little is known about TIME in carcinoid tumors.10 Here, we describe a patient who had heterogeneous TIME between primary and metastatic carcinoid tumors which differentially responded to chemoimmunotherapy. This study may provide new insights into the mechanism of primary and acquired resistance to immunotherapy in carcinoid tumors.
Case report
A 72-year-old man was diagnosed with advanced pulmonary carcinoid with multiple bone metastases (Fig 1). CT-guided biopsies of lung and scapular tumors confirmed the diagnoses of typical carcinoid (PD-L1, 1%–24%; Oncomine Dx target test, negative; microsatellite instability [MSI], negative) and atypical carcinoid (PD-L1, negative; Oncomine Dx, negative; MSI, negative), respectively.
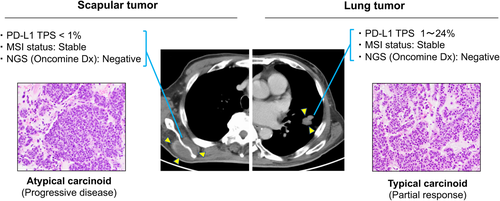
The patient received atezolizumab in combination with carboplatin plus etoposide as first-line therapy. Although a CT scan showed a partial response in the primary lung lesion, the scapular tumor was significantly enlarged after two cycles of chemoimmunotherapy. There was no antitumor effect on other bone metastases similar to the scapula tumor. Thus, a progressive disease was evaluated according to RECIST version 1.1.
Understanding the intersite tumor-immune heterogeneity is essential to harness the immune system for cancer therapy. However, little is known about TIME in pulmonary carcinoid tumors. To further explore this case, we investigated the immune contexture of pretreatment primary and metastatic tumors by fluorescent multiplex immunohistochemistry (Supplementary Text S1), which can capture multidimensional data related to tissue architecture, spatial distribution of multiple cell phenotypes, and co-expression of signaling.11, 12 Synaptophysin and PD-L1 were simultaneously stained and the tissue localizations of tumor-infiltrating lymphocytes (TIL) were evaluated. CD8+ T cells and immunosuppressive CD3+FOXP3+ regulatory T cells (Tregs) in the tumor nest and surrounding stroma were profiled and quantified by quantitative pathology imaging system. CD8+ T cell infiltrations were detected in the tumor nest of PD-L1-positive primary lung carcinoid; however, they were mostly restrained in the stroma of the PD-L1-negative metastatic scapular tumor. Treg infiltrations into both tumor nests and stroma were detected in the primary lung carcinoid tumor, however, which were not detected in the metastatic scapular tumor (Fig 2).
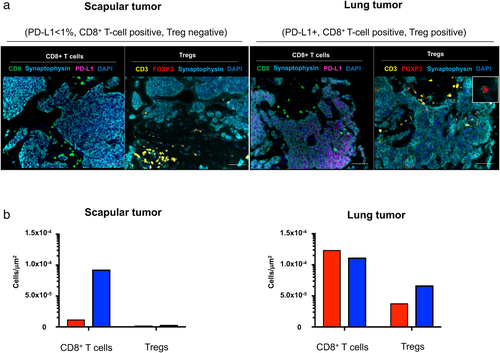
 ) Tumor nest, (
) Tumor nest, ( ) Tumor stroma
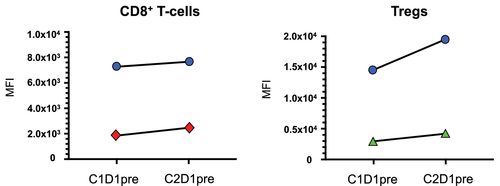
) Tumor stromaWe evaluated a systemic immune response in the peripheral blood. Multiparameter flow cytometric analysis was performed on the peripheral blood mononuclear cells (PBMCs) as previously described (Supplementary Text S1).13-15 PD-1 and Ki67 in CD8+ T cells increased after one-cycle of chemoimmunotherapy, suggesting systemic immune activation was induced by blocking PD-1/PD-L1 pathway (Fig 3). However, CTLA-4 and Ki67 expressions in Tregs simultaneously increased, indicating Treg activation was induced by blocking the PD-1/PD-L1 pathway.
 ) Ki67, (
) Ki67, ( ) PD-1, (
) PD-1, ( ) Ki67, (
) Ki67, ( ) CTLA-4
) CTLA-4Discussion
Jiménez-Sánchez et al. reported that multiple distinct TIME co-exist within a single individual and heterogeneous TIME was associated with the heterogeneous fates of metastatic lesions,8 which were consistent with our findings. In the current study, a significant CD8+ T cell infiltration was seen in the tumor nest of the PD-L1-positive lung carcinoid, which was associated with a significant response to chemoimmunotherapy, despite Treg infiltration in both the tumor nest and stroma. However, CD8+ T cell infiltration was restrained in the surrounding stroma in the PD-L1-negative metastatic scapular tumor and which was associated with primary resistance to chemoimmunotherapy, suggesting that the infiltrating CD8+ T cells in the tumor nest may play a key role in response to ICIs in advanced carcinoid tumors.
Tregs have immunosuppressive activity and have been reported to play a critical role in negatively regulating antitumor immune responses.16 Activation of systemic Tregs with an increase of CTLA-4 expression was confirmed after treatment with ICI followed by disease progression, suggesting that the CTLA-4 signaling pathway could be one of the key mechanisms of acquired resistance to PD-1/PD-L1 blockade therapy in carcinoid.
Lung carcinoid tumors are categorized as typical (<2 mitoses per 2 mm2 and no necrosis) and atypical (2–10 mitoses per 2 mm2 and/or necrosis), corresponding to low-grade (grade 1) and intermediate-grade (grade 2), respectively.17 These categories were developed for resected primary tumors. A biopsied specimen represents only part of a whole tumor. Tumor heterogeneity within neuroendocrine tumors has been previously reported.17 Thus, the tumor heterogeneity of tissue specimens obtained by CT-guided biopsies may have affected the difference of diagnosis in the current study.
Everolimus is an oral mammalian target of rapamycin inhibitor approved for NETs based on a clinical trial (RADIANT-4).18 In this study, efficacy of everolimus compared to placebo in previously-treated patients was reported. The current patient showed rapid progression of tumors at diagnosis. Therefore, we chose atezolizumab in combination with chemotherapy, which is currently used for poorly differentiated NET, small cell lung cancer as the first-line therapy.
In our study, the PD-L1-positive primary tumor responded to therapy; however, the predictive value of PD-L1 has not yet been validated in NET immunotherapy. Therefore, our findings should be interpreted with caution. Only one patient was involved in this study, thus further studies are needed to determine whether the principles discovered here apply to other patients with carcinoid tumors. Despite such limitations, the present study provides the first evidence of the coexistence of heterogeneous TIME within a single individual with a pulmonary carcinoid tumor. The present study may therefore contribute to our understanding of the TIME of carcinoids and provide new insights into the complex TIME of NETs.
Acknowledgments
We thank Misako Takahashi (Department of Respiratory Medicine, Kumamoto University) for technical assistance in vitro analysis. We are very grateful to our patient for participation in this study. This work was supported by JSPS KAKENHI Grant Number JP18K15928 and Takeda Science Foundation.
Disclosure
No potential conflicts of interest were disclosed.