Divergent trends of hospitalizations for upper and lower gastrointestinal bleeding based on population prescriptions of aspirin, proton pump inhibitors and Helicobacter pylori eradication therapy
Trends of upper and lower gastrointestinal bleeding
Abstract
Background
With the increasing use of medications that alter the risk of gastrointestinal bleeding (GIB), comprising aspirin, proton pump inhibitors (PPIs), and Helicobacter pylori eradication therapies, the trends of GIB are evolving.
Objective
The aim of this study is to determine and predict the trends of GIB and to evaluate the effects of population prescriptions of these medications on GIB incidences.
Methods
We retrieved patients hospitalized for GIB in all public hospitals in Hong Kong between 2009 and 2019. Monthly age- and sex-standardized GIB data were fitted and predicted, based on population prescriptions of aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs), anticoagulants, other antiplatelet drugs, PPIs, and H. pylori therapies, using autoregressive integrated moving average model for time series analysis.
Results
The incidence of upper GIB (UGIB) showed a clear declining trend while lower GIB (LGIB) decreased slightly. Older population (>80 years) had the greatest decline in UGIB but was associated with an increase in LGIB. Prescriptions of PPIs and aspirin increased significantly with time. PPIs prescriptions were negatively associated with UGIB incidence (coefficient log(PPIs) −4.58; 95% confidence interval [CI]: −5.69, −3.47). H. pylori eradication in the previous month showed a nonsignificant trend on UGIB (coefficient −0.14; 95% CI: −0.30, 0.02). In contrast, aspirin increased the incidences of UGIB (coefficient 0.06; 95% CI: 0.04, 0.07) and LGIB (coefficient 0.04; 95% CI: 0.03, 0.05). NSAIDs, anticoagulants, and other antiplatelet drugs were not significantly associated with the trend of either UGIB or LGIB. UGIB is predicted to decline continuously but LGIB is projected to rise, particularly with increasing use of aspirin.
Conclusions
UGIB incidences were decreasing and had been surpassed by LGIB. Based on population prescriptions of aspirin and PPIs, divergent trends of upper and lower GIB are expected, especially in elderly.
Key summary
Summarize the established knowledge on this subject
-
With increasing use of proton pump inhibitors (PPIs) and Helicobacter pylori eradication therapy, the incidences of upper gastrointestinal bleeding (UGIB) are declining.
-
The increasing use of antiplatelets and anticoagulants, however, increases the risk of both UGIB and lower gastrointestinal bleeding (LGIB).
-
The dynamic contribution of these factors on the incidences of UGIB and LGIB at population level remains uncertain.
What are the significant and/or new findings of this study?
-
The incidences of UGIB showed a clear declining trend while LGIB decreased slightly over the past decade in Hong Kong.
-
LGIB had actually surpassed UGIB as the leading source of GIB, especially among older population.
-
The increasing PPIs prescription was associated with the falling incidences of UGIB, whereas the rising use of aspirin was associated with both an increase in UGIB and LGIB.
-
With the increasing use of aspirin and the lack of effective prevention preventive strategies, LGIB would become a major health challenge.
1 INTRODUCTION
Gastrointestinal bleeding (GIB) is one of the major causes of emergency hospital admission. In the United States, GIB accounted for more than 500,000 hospitalizations and consumed nearly US$5 billion in 2014.1 With the increasing use of proton pump inhibitors (PPIs) and Helicobacter pylori eradication therapy, the incidence of upper GIB (UGIB) is declining.2-8 On the other hand, epidemiological data on lower GIB (LGIB) are limited. Lanas et al.2 reported a significant increase in the incidences of LGIB in Spain, which may be caused by the increasing use of nonsteroidal anti-inflammatory drugs (NSAIDs), especially aspirin, and the lack of effective preventive strategies of LGIB.9
Thus far, the effects of various medications on the trends of GIB have not been properly investigated, particularly in population setting. Miyamoto et al.4 reported that the annual incidence of UGIB was negatively associated with PPIs use. Some studies also investigated the relationship between the prescriptions of aspirin, NSAIDs or other drugs and the incidences of UGIB.6, 10 However, the issues of autocorrelation (data are not independent, particularly for those in the near time) in time series data were not formally addressed in these studies, which may lead to spurious correlation.11
Aging is another challenge faced by many countries and regions including Hong Kong. While both GIB incidences and medication usages including aspirin, PPIs, NSAIDs, anticoagulants, and other antiplatelet drugs, are more common in the older population, the impacts of these medications on the trend of GIB remains uncertain.
The aim of this study was to determine and to forecast the time trends of nonvariceal UGIB and LGIB in Hong Kong, as well as to evaluate the effects of population prescriptions of aspirin, NSAIDs, anticoagulants, other antiplatelet drugs, PPIs, and H. pylori eradication therapies on the GIB trends.
2 METHODS
2.1 Data source
All GIB hospitalization and drug prescription records were retrieved from the Clinical Data Analysis and Reporting System (CDARS), an electronic healthcare database of the Hong Kong Hospital Authority, which is the only public healthcare provider for the 7 million population. Patient's key information, including demographics, hospitalization, visits to outpatient clinics and emergency departments, diagnoses, and drug prescription in all public hospitals and clinics are recorded. This database has been previously used in a number of high-quality studies.12-15 The International Classification of Diseases, 9th Revision (ICD-9) is the coding system used in CDARS, which has been verified in our previous study on GIB.16 All nonvariceal UGIB, LGIB and other unspecified GIB hospitalizations between 2009 and 2019 were retrieved from the CDARS using ICD-9 codes (Table S1 and Supporting Information Methods). The monthly crude incidence rates of GIB were expressed in 100,000 person-months.
Prescriptions of aspirin, PPIs (omeprazole, lansoprazole, esomeprazole, pantoprazole, and rabeprazole), NSAIDs (ibuprofen, naproxen, diclofenac, indomethacin, mefenamic, piroxicam, celecoxib, etoricoxib), anticoagulants (warfarin, dabigatran, apixaban, edoxaban, rivaroxaban), and other antiplatelet drugs (clopidogrel, dipyridamole, cilostazol, ticagrelor, ticlopidine) given between January 2009 and December 2018 in all hospitals and clinics of the Hospital Authority, were retrieved by months from the CDARS. We included only outpatient oral medications in this analysis. We determined the cumulative durations of prescription given in a month, in terms of prescription days per 100,000 person-months. Since it was not possible to estimate the proportion of H. pylori-infected population, we identified the number of patients (count per 100,000 person-months) who had received their first course of clarithromycin-containing triple therapy for H. pylori eradication,12, 14 which was the first-line therapy in Hong Kong during the study period.17
Population demographics of Hong Kong over the study period were obtained from Hong Kong Annual Digest of Statistics.18 The mid-year population by age and sex groups were extracted.
2.2 Outcomes and statistical analysis
The GIB incidence and covariates were standardized by age and sex based on the Hong Kong population in 2018. To better present the time trend, the trend component of the GIB data were generated after decomposing using additive model. In addition, the time trend was also tested using linear regression. To model UGIB and LGIB trend, the autoregressive integrated moving average model (ARIMA) was used (Supporting Information Methods), which addressed the autocorrelation of the data. The parameters (coefficient and 95% confidence interval [CI]) were estimated using maximum likelihood estimation.11, 19 Non-UGIB, which included LGIB plus unspecified GIB, was also analyzed.
The cumulative prescriptions and number of patients who had received H. pylori eradication were included as covariates. Based on the characteristic of the data, transformation, such as logarithm, was performed when necessary. The data, GIB incidence and covariates, were split into training set (January 2009 to December 2015) and test set (January 2016 to December 2018), and the training data were firstly used to fit the model. The mean absolute error (MAE) were calculated to test the accuracy of forecast.19 The whole dataset were also used to fit the model, with which forecasts of UGIB and LGIB in the following 3 years, 2019–2021, were performed based on predicted covariates or artificially assumed level (Supporting Information Methods). To further validate the prediction, standardized GIB incidences observed in 2019 were retrieved.
The incidences of UGIB and LGIB were stratified by sex and age (0–14, 15–44, 45–59, 60–79, and ≥80 years) to compare the time trends. Incidences of GIB in different groups were compared using Student's t-test paired by age and month. A p < 0.05 was considered statistically significant. All statistical analyses were performed using the R 3.5.1.
2.3 Ethics approval
This study was approved by Institutional Review Board of the University of Hong Kong and the Hospital Authority Hong Kong West Cluster on 12 September 2019 (Reference Number: UW19-543). Our study did not require a written informed consent because it was based on electronic database of anonymous patient's data. The study protocol conforms to the ethical guidelines of the Declaration of Helsinki.
3 RESULTS
3.1 Time trends of medication prescriptions
During the study period, the prescriptions of PPIs and aspirin all showed rising trends (p for trend <0.001, Figure 1). In particular, the prescription of PPIs increased by 4.4-fold (from 24,190 days per 100,000 person-months in January 2009 to 105,320 in December 2018) and aspirin increased by about 1.2-fold (from 109,070 to 134,980 days per 100,000 person-months). Based on the historical values of aspirin or PPIs prescriptions, prescriptions of both aspirin and PPIs were predicted to continue to increase in the following 3 years (Figure 1). Similarly, the use of NSAIDs, anticoagulants and other antiplatelet drugs also experienced slight rising trends, but the level was much lower than that of PPIs and aspirin. The trend of NSAIDs prescription also remained relatively static after 2016. In contrast, a decrease in the number of patients who had received H. pylori eradication therapy was observed, which dropped from the highest of 10.57 per 100,000 person-months in February 2009 to 7.27 in December 2018 (p for trend <0.001), and the number was predicted to remain stable (Figure S1).
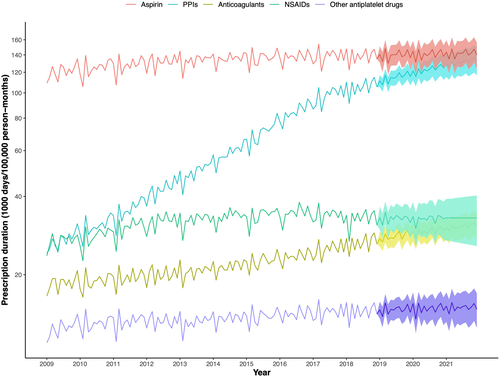
Trends of medications prescribed over the study period (2009–2018) and their predicted values (2019–2021)
3.2 Time trend and forecast of UGIB
A total of 169,699 GIB events were identified from 2009 to 2019, including 56,884 (33.5%) nonvariceal UGIB and 74,230 (43.7%) LGIB. The monthly incidence of UGIB showed a clear decreasing trend from 10.42 per 100,000 person-months in January 2009 to 3.26 in December 2019 (coefficient for trend −0.05; p < 0.001; Figure 2), which was more obvious after decomposing, especially after 2010 (Figure S2).
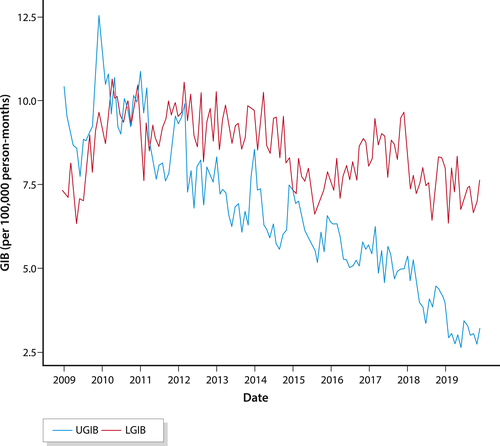
Time trends of age- and sex-standardized GIB incidence from 2009 to 2019. GIB, gastrointestinal bleeding
The incidence of UGIB increased with age and the highest incidence rate was noted in the ≥80 years group (Figure 3). After stratified by sex, men had more UGIB than women (p < 0.001). Notably, the decreasing trend of UGIB was also more obvious in the older age groups, especially in 60–79 and ≥80 age groups, in both male and female (Figure 3).
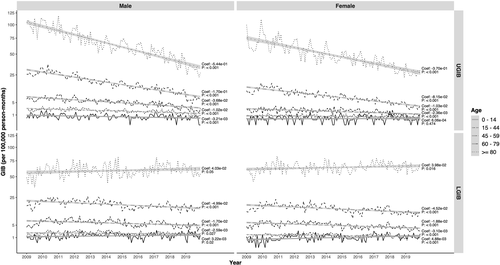
GIB incidences stratified by age and sex. GIB, gastrointestinal bleeding
Using the ARIMA model, the MAE was 0.38 and 0.61 for the training set and test set, respectively (Figure S3A). Increasing consumption of aspirin was associated with an increase in the UGIB incidence by 0.06 (95% CI: 0.04, 0.07) per 100,000 person-months, for every 1000 days per 100,000 person-months increase in aspirin prescription (Table 1). In contrast, increasing PPIs consumption was associated with a decrease in the incidence of UGIB with the coefficient of −4.58 (95% CI: −5.69, −3.47) for PPIs after logarithm. H. pylori eradication in the previous month (lag 1 month) showed a nonsignificant negative trend on UGIB (coefficient −0.14; 95% CI: −0.30, 0.02). No significant association was however detected between prescriptions of NSAIDs (coefficient 0.01; 95% CI: −0.05, 0.08), anticoagulants (coefficient 0; 95% CI: −0.20, 0.21), or other antiplatelet drugs (coefficient −0.04; 95% CI: −0.44, 0.35) and UGIB, which were therefore not included in the final model. Though the number of patients who had received H. pylori eradication was not significantly associated with the trend of UGIB, it was also adjusted in the ARIMA model considering its clinical impact on UGIB and the relatively large absolute value of the coefficient.
| Coefficients (95% CI) | p Value | |
|---|---|---|
| UGIB | ||
| Aspirin | 0.06 (0.04, 0.07) | <0.001 |
| PPIsa | −4.58 (−5.69, −3.47) | <0.001 |
| H. pylori eradicationb | −0.14 (−0.30, 0.02) | 0.09 |
| LGIB | ||
| Aspirin | 0.04 (0.03, −0.05) | <0.001 |
| Non-UGIB | ||
| Aspirin | 0.07 (0.05, 0.09) | 0.02 |
| PPIsa | −1.94 (−3.62, −0.25) | <0.001 |
- Abbreviations: ARIMA, autoregressive integrated moving average model; CI, confidence interval; LGIB, lower gastrointestinal bleeding; PPIs, proton pump inhibitors; UGIB, upper gastrointestinal bleeding.
- a Logarithm was used for the prescription of PPIs.
- b Data lagged 1 month for number of patients who received H. pylori eradication was used.
Based on the ARIMA model (Table S2), the incidence of UGIB is predicted to continue to decline in the following 3 years (Figure 4a). An additional 20% increase in PPIs prescription was associated with a further decrease in the incidence of UGIB, whereas 20% increase in aspirin prescription would increase the incidence. To verify our prediction, the actual UGIB incidences observed in 2019 were found to be at the lower borderline of the predicted region.
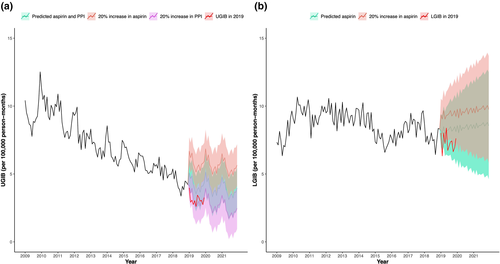
Forecast of UGIB and LGIB incidences based on different levels of PPIs or aspirin prescription for 2019–2021, and the actual observed incidences in 2019. STROBE Statement—Checklist of items that should be included in reports of observational studies. LGIB, lower gastrointestinal bleeding; PPIs, proton pump inhibitors; UGIB, upper gastrointestinal bleeding
3.3 Time trends and forecast of LGIB
While UGIB was more prevalent than LGIB in 2009, LGIB dominated from 2011 onwards (Figure 2). The ratio of UGIB to LGIB dropped from 1.43 in January 2009 to 0.43 in December 2019. The incidence of LGIB fluctuated around 8.51 per 100,000 person-months during the study period with a gradual declining trend (coefficient for trend −0.01; p < 0.001), but the trend was less marked as UGIB (Figures 2 and S2). After stratifying by age, increasing trend of LGIB was observed in the oldest age group (≥80 years) in both male and female (Figure 3). Unlike UGIB, there was no significant difference in the incidence of LGIB between male and female (p = 0.487).
In the model for LGIB, the MAE was 0.49 and 0.82 for the training set and test set, respectively (Figure S3B). Aspirin prescriptions were positively associated with the incidence of LGIB (coefficient 0.04; 95% CI: 0.03, 0.05; Table 1). However, PPIs (coefficient −1.01; 95% CI: −2.26, 0.24), NSAIDs (coefficient 0.02; 95% CI: −0.03, 0.07), anticoagulants (coefficient 0.04; 95% CI: −0.19, 0.28), or other antiplatelet drugs (coefficient 0.10; 95% CI: −0.37, 0.56) were not significantly associated with LGIB and were not included in the prediction model. The incidence of LGIB was predicted to increase in the following 3 years, and further increase in aspirin prescription would increase the incidence of LGIB (Figure 4b). The actual LGIB incidence observed in 2019 was also within the predicted range.
3.4 Sensitivity analysis
Sensitivity analysis on non-UGIB (Supporting Information Results), which comprises of LGIB and all unspecified GIB, showed that aspirin was again positively associated with incidence of non-UGIB with the coefficient of 0.07 (95% CI: 0.05, 0.09; Table 1), but PPIs were also negatively associated with the incidence of non-UGIB (coefficient for PPIs after logarithm −1.94; 95% CI: −3.62, −0.25).
4 DISCUSSION
The trends of GIB incidence are evolving rapidly in most countries due to multiple reasons including aging population with comorbidities, changing patterns of prescription that would modify the risk of GIB as well as the declining prevalence of H. pylori infection. In this study that was based on the population prescription volume and GIB hospitalization records of Hong Kong, we reported the dynamic trends of all GIB incidences over a 10-year period. We showed that hospitalizations for nonvariceal UGIB had a progressively declining trend over the past decade. Although LGIB also showed a slight decreasing trend, a rising trend was observed in the oldest age group (≥80 years). Notably, the incidence of LGIB has surpassed UGIB from 2011 and became the leading source of GIB in Hong Kong. Accordingly, the UGIB to LGIB ratio has decreased from 1.43 in January 2009 to 0.43 in December 2019.
The numbers of prescriptions of aspirin, PPIs, and anticoagulants all showed increasing trends during this period. The increasing use of PPIs was associated with a decline in the incidence of UGIB, but not LGIB. While there was a gradual reduction in the number of H. pylori eradication therapies prescribed over the study period, there was only a nonsignificant trend on UGIB with a lag time of 1 month. In contrast, the number of aspirin prescriptions were associated with both increase in the incidence of UGIB and LGIB. We also found that prescriptions of NSAIDs, anticoagulants, and other antiplatelet drugs were not significantly associated with the incidences UGIB or LGIB. We speculated this may be related to the use of population-level data to evaluate their effect on the overall GIB trend instead of determining individual's bleeding risk. While the population-level prescriptions of these drugs were much lower than PPIs and aspirin, their contributions may be less obvious in the overall GIB trend.
Based on the trends of prescription of aspirin, PPIs and H. pylori eradication, UGIB is forecast to continue to decline in the subsequent 3 years but the trend of LGIB is forecast to increase slightly. Although time trends of gastrointestinal events have been reported in previous studies, most studies focused on upper gastrointestinal events, especially peptic ulcer and its complications.2-8, 20-27 While most studies reported decreasing trends of UGIB or peptic ulcer bleeding, several studies found either no decline or even a rising trend of UGIB.20, 22, 24, 27
We showed that the declining trends of UGIB were more obvious among older patients, especially in 60–79 and ≥80 age group, which was consistent with the study by Lanas et al.2 However, Kang et al.28 reported that admission rates for peptic ulcer bleeding was actually increased for older people. Similar observation was made by Bakkevold et al.24 In another study from Spain, the decline in the incidence of peptic ulcer complication was particularly evident in the younger (<65 years), but there was no clear decline among older patients.29 Loperfido et al.30 also reported a decreasing trend in patients <70 years. We speculated that these differences may be related to different background prevalence of H. pylori infection, and more importantly, the failure to account for concurrent medications used, particularly for PPIs and aspirin which are commonly prescribed in elderly patients.
On the other hand, studies on LGIB trends were limited and the results were even more conflicting.2, 3, 7, 21, 31 In our study, an overall slight decreasing trend of LGIB was found, but the oldest (>80 years) age group had a rising trend. Cavallaro et al.7 reported a nonsignificant increasing trend of LGIB, whereas Laine et al.21 reported a decreasing trend of LGIB and Lanas et al.2 found an increasing trend of lower GI complications, particularly in patients >60 years. This was similar with the increasing trend of LGIB in age group ≥80 in our study. The rise in LGIB incidences in older patients are not unexpected. First, diverticulitis and ischemic colitis, which are also the common causes of LGIB, are more prevalent in older patients.32, 33 Second, the high consumption of aspirin or NSAIDs in the old population may also drive the increasing trend of LGIB. With the projected increase in aspirin prescription, the incidence of LGIB was however predicted to increase slightly in the next 3 years. Lanas et al.2 also reported the rates for upper and lower GI complications converged with time and the ratio of upper versus lower GI events dropped from 4.3 in 1996 to 1.4 in 2005. In our study, although LGIB has surpassed UGIB after 2011, it was mainly caused by the decline in UGIB rather than actual increase in LGIB.
Though there is increasing concern that the potent acid suppression by PPIs could increase the risk of LGIB by altering intestinal microbiota,9, 34 the numbers of PPIs prescriptions was not found to be associated with the incidence of LGIB in our study. Indeed, PPIs prescriptions were found to be negatively associated with the incidence of non-UGIB (i.e., combining LGIB and unspecified GIB) which also included small bowel bleeding. Hence, at least from population perspectives, the increased prescription of PPIs was not associated with a parallel increase in LGIB and possibly small bowel bleeding.
One of the strengths of this study is the use of population prescription to associate with the major clinical outcome of GIB hospitalizations by using a comprehensive public healthcare database from Hong Kong. Also, since prescription and dispensing are all conducted in the same setting in public hospital and clinics in Hong Kong at a very low cost (US$2 per item for 16 weeks), the prescription record generally matches the dispensing record. Although a number of studies have investigated the effect of drug use on GIB risk in patient-based studies, the association between drug consumption and time trends of GIB incidence were not well investigated, particularly for LGIB. Moreover, the statistical methods employed in previous analyses were not robust enough with only descriptive analysis or traditional regression analysis performed.4, 6, 10, 27-29, 35, 36 In our study, we studied the association between GIB trend and medication consumptions or H. pylori eradication after addressing the autocorrelation using ARIMA models, which was one of the most commonly used methods for time series analysis.
Our study has limitations. First, despite multiple measures to ascertain the source of bleeding in the electronic database by retrieving all other possible relevant information, the proportion of unspecified GIB was high (22.8%). We have, however, performed a sensitivity analysis combing unspecified GIB and LGIB as non-UGIB, which yielded consistent results. The validation of the GIB codes during the same period has been conducted in a previous study that the positive predictive value and negative predictive value of GIB codes was 100% and 98%, respectively.16 Second, we only evaluated the prescription durations without considering individual dosage in our analysis. However, prescription duration could better reflect the time effects of these medications on GIB. In addition, at population level, the primary dosage is usually stable for a particular drug, especially for commonly used medications such as aspirin and PPIs.
5 CONCLUSION
The incidence of hospitalization for nonvariceal UGIB showed a progressively decreasing trend over the past decade in Hong Kong, which has been surpassed by LGIB. Older patients, in particular, had the largest drop in UGIB but were associated with a rising incidence of LGIB. The increasing PPIs prescription was associated with the falling incidence of UGIB, whereas the rising trend of aspirin prescription was associated with both an increase in upper and lower GIB. Based on the predicted population prescription of aspirin and PPIs, UGIB is forecasted to continue to decline but LGIB is forecasted to rise, particularly with the increasing use of aspirins.
ACKNOWLEDGMENTS
The authors thank the Hospital Authority of Hong Kong for the use the Clinical Data Analysis and Reporting System and all staff members for their work on the system maintenance. Authors are also in debt to Lijia Chen for her work on initial data clearance.
CONFLICT OF INTERESTS
W. K. L. has received speaker fee from Eisai, Ipsen and honorarium for attending advisory board for Janssen and Pfizer, which are not related with this study. Other authors have no conflict of interest to declare.
Open Research
DATA AVAILABILITY STATEMENT
Raw data were retrieved from the Clinical Data Analysis and Reporting System of the Hong Kong Hospital Authority, an local electronic healthcare database, which are not publicly available. Derived data supporting the findings of this study are available within the article and the supplementary materials.




