Clinical Guidelines for the Prevention and Treatment of Radiation-induced Bladder Injury
Abstract
Radiation-induced bladder injury is a common complication after pelvic radiotherapy. Few studies exist on diagnosing and treating radiation-induced bladder injury, with no established guidelines or consensus in China or internationally. Clinical physicians' diagnosis and treatment of radiation-induced bladder injury are primarily based on their own clinical experience, and there is an urgent need for unified guidelines to standardize clinical diagnosis and treatment. Therefore, the Chinese Radiation Therapy Oncology Group, China Anti-Cancer Association Tumor Support Therapy Committee, and China Anti-Cancer Association Tumor Radiation Protection Committee gathered experts to develop Chinese clinical practice guidelines, guiding diagnosing and treating radiation-induced bladder injury. The development of these guidelines adopted the grading system of evidence quality and recommendation strength (GRADE).
Radiotherapy is widely used in pelvic tumors, and the bladder is a critical organ at risk during pelvic radiotherapy. Acute or chronic radiation-induced bladder injury can occur after radiotherapy for pelvic tumors, with the most typical manifestation being bladder bleeding, which significantly affects patients' quality of life. As the cure rate of tumors improves, enhancing the quality of life for cancer patients after treatment has become an essential goal in cancer therapy, making the prevention and treatment of radiotherapy complications a significant research topic. There are few studies on diagnosing and treating radiation-induced bladder injury, and there is a lack of high-level clinical trials.
To our knowledge, there are no guidelines or consensus on preventing and treating radiation-induced bladder injury in China and no widely accepted international guidelines or consensus. In recent years, various new drugs have been used for the prevention and treatment of radiation-induced bladder injury, but their clinical use lacks standardized guidance. Clinical physicians' diagnosis and treatment of radiation-induced bladder injury is mainly based on their clinical experience, lacking unified guidelines to standardize clinical diagnosis and treatment. Therefore, the Chinese Radiation Therapy Oncology Group, China Anti-Cancer Association Tumor Support Therapy Committee, and China Anti-Cancer Association Tumor Radiation Protection Committee gathered experts to develop this guideline, aiming to standardize the clinical practice of radiation-induced bladder injury and benefit radiotherapy patients. The development of this guideline adopted the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system for evidence quality and recommendation strength ,1 as shown in Table 1.
| Rank | Explanation | Examples |
|---|---|---|
| High | The authors have a lot of confidence that the true effect is similar to the estimated effect | Randomized trials without serious limitations; Well-performed observational studies with very large effects(or other qualifying factors) |
| Moderate | The authors believe that the true effect is probably close to the estimated effect | Randomized trials with serious limitations; Well-performed observational studies yielding large effects |
| Low | The true effect might be markedly different from the estimated effect | Randomized trials with very serious limitations; Observational studies without special strengths or important limitations |
| Very Low | The true effect is probably markedly different from the estimated effect | Randomized trials with very serious limitations and inconsistent results; Observational studies with serious limitations; Unsystematic clinical observations (e.g., case series or case reports) |
| Recommendation Strength | Description | / |
| Strong | All or almost all persons would choose that intervention. | / |
| Weak | There is likely to be an important variation in the decision that informed persons are likely to make. | / |
- Abbreviations: GRADE - Grading of Recommendations Assessment, Development, and Evaluation; RCT - Randomized Controlled Trial.
1 DEFINITION
Radiation-induced bladder injury refers to radiation-related bladder injuries caused by pelvic radiotherapy (cervical cancer, endometrial cancer, rectal cancer, prostate cancer, bladder cancer, and anal cancer, et al.), among which radiation cystitis is the most common. With a three-month threshold from the start of radiotherapy, it can be classified into acute radiation-induced bladder injury and late radiation-induced bladder injury. Acute radiation-induced bladder injury is usually a self-limiting disease, gradually alleviating after the end of radiotherapy. Late radiation-induced bladder injury can occur months to years after radiotherapy, with varying durations, and severe cases may present with bladder fistulas.
2 EPIDEMIOLOGY
Radiation-induced bladder injury is a common adverse reaction following pelvic radiotherapy. The incidence of ≥G2 acute radiation-induced bladder or urogenital system injury after pelvic radiotherapy ranges from 20% to 60%,2-5 and the incidence of ≥G3 acute injury is ≤4%.5-7 The incidence of ≥G2 late radiation-induced bladder or urogenital system injury after radiotherapy is 10% to 30%,1, 3, 6 while the incidence of ≥G3 late injury is 1% to 7%.3, 7, 8
3 PATHOGENESIS
The bladder wall can be divided into the mucosal layer, muscular layer, and outer membrane(Figure 1). The mucosal layer can be divided into the bladder epithelium, basement membrane, and lamina propria. The bladder epithelium is a transitional epithelium with umbrella cells on its surface. Extensive tight junctions and bridge granules exist between umbrella cells, preventing urine leakage. The surface of umbrella cells is covered by plaques (asymmetric unit membranes) containing transmembrane proteins uroplakins (UP), including UPIa, UPIb, UPII, and UPIII. Among them, UPIII plays a vital role in the bladder epithelium structure. The bladder epithelium also contains a glycosaminoglycan (GAG) layer covering the umbrella cells. The tight connections between umbrella cells, bladder epithelial plaques, and the GAG layer form the bladder epithelial barrier, preventing hypertonic solutes and urine pathogens from invading bladder tissues and entering the bloodstream.9
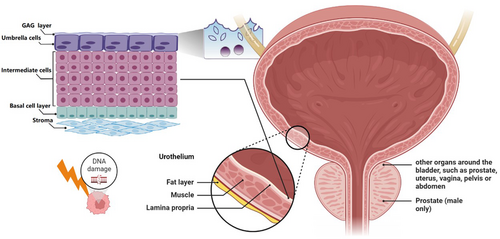
Acute radiation-induced bladder injury is mainly caused by damage to the bladder epithelium and microvessels. After radiation exposure to the bladder, the bladder epithelial barrier is affected, resulting in a reduction of umbrella cells, loss of the surface UPIII layer, and destruction of the GAG layer.10 Since the renewal rate of bladder epithelial cells is slow (42∼350 d), acute radiation-induced bladder injury does not cause severe destruction of bladder tissue structure.9 After the bladder epithelial barrier is damaged, hypertonic urine can penetrate the bladder wall and induce an inflammatory response. Subsequently, mast cells are activated, releasing histamine through degranulation, causing vasodilation and tissue swelling, leading to more severe bladder injury. Electrolytes, histamine, and other inflammatory substances in urine stimulate nerve endings in the bladder wall. The destruction of the bladder epithelial barrier also makes the bladder susceptible to secondary infections, further aggravating bladder injury.
Endothelial cells are essential target cells for bladder irradiation. Damage to microvascular endothelial cells results in acute inflammation, leading to edema in the bladder mucosa, submucosa, and muscular layer. Bladder smooth muscle fibers are replaced by fibroblasts due to microvascular ischemia, edema, and cell damage, resulting in increased collagen deposition. After radiation exposure, the bladder experiences smooth muscle edema, fibroblast substitution, collagen deposition, and vascular ischemia.11, 12
Cell adhesion molecules and prostaglandin synthesis increase at the molecular response mechanism level after radiation exposure to the bladder. This leads to increased inflammatory response and edema in the muscular layer, decreasing bladder capacity and causing bladder irritation symptoms.13, 14
4 CLINICAL MANIFESTATIONS
Acute radiation-induced bladder injury occurs during or after a period of radiotherapy. Common symptoms include urinary frequency, urgency, difficulty in urination, hematuria, and pain, which affect patients' quality of life and prolong hospitalization time. Most patients experience mild, self-limiting symptoms that gradually alleviate after radiotherapy cessation. A few patients may experience symptoms lasting up to 3 months after radiotherapy.
Late radiation-induced bladder injury mainly occurs between 6 months and 20 years after radiotherapy, with an average latency period of about 3 years.15 The most common symptom is bleeding; mild cases may present as microscopic hematuria or mild gross hematuria, while severe cases may require repeated blood transfusions due to anemia caused by bleeding, even posing life-threatening risks. Blood clots resulting from hematuria can cause urinary retention and urinary tract obstruction. Hematuria may be accompanied by pain, urinary frequency, urgency, incontinence, and decreased bladder capacity. Severe radiation-induced bladder injury can lead to bladder fistulas, such as vesicovaginal and vesicorectal fistulas.
5 GRADING CRITERIA
Grading of radiation-induced bladder injury can be done using the Radiation Therapy Oncology Group/European Organization for Research and Treatment of Cancer (RTOG/EORTC) acute and late radiation injury grading criteria16 or the Common Terminology Criteria for Adverse Events (CTCAE) by the National Cancer Institute. The RTOG/EORTC acute injury grading criteria apply to radiation injuries occurring within 1–90 days from the start of radiotherapy, while injuries occurring after 90 days use the late injury grading criteria (Table 2). The CTCAE is currently updated to version 5.0, and commonly used adverse event assessments for radiation-induced bladder injury include hematuria, non-infectious cystitis, urinary frequency, urgency, difficulty in urination, incontinence, urinary retention, bladder spasms, bladder perforation, and urinary fistulas.
| Grading Criteria | Grade 0 | Grade 1 | Grade 2 | Grade 3 | Grade 4 |
|---|---|---|---|---|---|
| RTOG/EORTC Acute (Genitourinary) | No change | Frequency of urination or nocturia twice pretreatment habit/dysuria, urgency not requiring medication |
Frequency of urination or nocturia that is less frequent than every hour. Dysuria, urgency, bladder spasm requiring local anesthetic (e.g.,Pyridium) |
Frequency with urgency and nocturia hourly or more frequently/dysuria, pelvis pain or bladder spasm requiring regular, frequent narcotic/gross hematuria with/without clot passage | Transfusion-requiring hematuria; bladder obstruction |
| RTOG/EORTC Late (Bladder) | None | Slight epithelial atrophy; minor telangiectasia (microscopic hematuria) | Moderate frequency; generalized telangiectasia; intermittent macroscopic hematuria | Severe frequency and dysuria; Severe generalized telangiectasia (often with petechiae); Frequent hematuria; Reduction in bladder capacity (<150 cc) | Necrosis/Contracted bladder(capacity < 100 cc); Severe hemorrhagic cystitis |
- Abbreviation: RTOG/EORTC - Radiation Therapy Oncology Group/European Organization for Research and Treatment of Cancer.
6 RISK FACTORS
The risk of radiation-induced bladder injury is related to the total radiotherapy dose, fractionated dose, and bladder irradiation dose volume.17 The higher the total dose of radiotherapy, the higher the risk of localized bladder injury, hematuria, and ulceration.18, 19 Diabetes, hypertension, smoking history, high body mass index, and a history of abdominal surgery are risk factors.20, 21 Surgery, postoperative complications, and chemotherapy can exacerbate late radiation-induced bladder injury. Concurrent treatments and individual radiosensitivity are also risk factors for radiation-induced bladder injury.
7 DIAGNOSIS
The diagnosis of radiation-induced bladder injury lacks a gold standard and mainly relies on a comprehensive judgment based on medical history, clinical presentation, physical examination, laboratory tests, cystoscopy, and imaging studies.
The clinical manifestations of radiation-induced bladder injury are mentioned earlier. A history of pelvic radiotherapy is a necessary condition for diagnosing radiation-induced bladder injury, and it is essential to collect information on the patient's radiotherapy timing, dose partitioning, radiotherapy techniques, and the dose received by the bladder. A thorough general physical examination and detailed pelvic examination are recommended for the patient.
Urinalysis and urine culture should be conducted to rule out urinary tract infections, and if infections are present, anti-infective treatment should be administered first. Other laboratory tests include complete blood count, kidney function, and, if necessary, tumor markers to differentiate from tumor progression.
For patients with gross hematuria, a cystoscopy can be performed. Under endoscopy, radiation-induced bladder injury can manifest as diffuse congestion and edema of the bladder mucosa; dilation and disorder of blood vessels in the lesion area, tortuous courses, and appearance engorged or clustered; submucosal bleeding can also be seen. In some patients, scattered or diffuse bleeding spots, ulcers, or necrotic lesions can be observed on the bladder mucosa. Inflammatory granulation tissue may be visible in some patients, primarily in the bladder's posterior wall and trigone area. Based on the cystoscopic findings, radiation-induced bladder injury can be divided into three categories: (1) inflammation-dominant type, characterized by edema, mucosal pallor, and ulceration; (2) bleeding-dominant type, characterized by capillary dilation and submucosal bleeding; (3) mixed type, with both inflammation and bleeding-dominant presentations22.
Imaging examinations such as CT or MRI can help differentiate upper urinary tract bleeding or pelvic tumor recurrence and progression.
- (1)
Urinary tract infection: Urinary tract infections can manifest with indications such as frequent urination, a sense of urgency, discomfort, and the presence of blood in the urine, commonly accompanied by a fever, raised levels of white blood cells in the bloodstream, and an elevated proportion of neutrophils. Urinary leukocytes may also be elevated, and antimicrobial therapy can be effective. A clean urine culture detecting the pathogen can confirm the diagnosis. It is important to note that radiation-induced bladder injury often coexists with urinary tract infections, exacerbating the symptoms of radiation-induced bladder injury.
- (2)
Tumor recurrence or progression: This may compress or invade the bladder, causing urinary frequency, pain, hematuria, and bladder fistulas. The condition can be differentiated based on patient history and imaging examinations and, if necessary, through biopsy and pathological examination.
- (3)
Drug-induced bladder injury: This is mainly caused by chemotherapy drugs, including common systemic chemotherapy drugs such as dimethyl sulfoxide, cyclophosphamide, ifosfamide, doxorubicin, paclitaxel, carboplatin, and bladder instillation chemotherapy agents such as mitomycin C, epirubicin, and thiotepa.23 Drug-induced bladder injury typically presents with hematuria, which may be accompanied by urinary frequency, urgency, and pelvic pain. The use of relevant drug history and cystoscopic findings can differentiate the condition.
8 PREVENTION
The most important method for preventing radiation-induced bladder injury is to reduce the dose and volume of radiation exposure. Cutting-edge radiotherapy methods, such as intensity-modulated radiotherapy (IMRT), image-guided radiotherapy (IGRT), and adaptive radiotherapy, can lower the bladder dose and better protect the bladder.19, 24, 25 During positioning and treatment, partial bladder displacement from high-dose areas can be achieved by moderately filling the bladder. Pay attention to limiting the bladder dose when creating a radiotherapy plan. Dose limitations for prostate cancer patients are as follows: 50% of the bladder <50-60 Gy, 30% of the bladder <70 Gy.26 Dose limitations for rectal cancer patients are as follows: 40% of the bladder ≤40 Gy, 15% of the bladder ≤45 Gy, maximum bladder dose ≤50 Gy; maximum allowable dose: 55% of the bladder ≤40 Gy, 30% of the bladder ≤45 Gy, 5% of the bladder ≤50 Gy.27 For patients with cervical cancer undergoing radical radiotherapy with image-guided three-dimensional brachytherapy, the total dose for 2cc of the bladder should be ≤90 Gy28; for two-dimensional brachytherapy, the bladder dose should be limited to 60%-70% of the prescription dose, not exceeding 80%.29
9 TREATMENT
9.1 Acute Radiation-induced Bladder Injury
Acute radiation-induced bladder injury is primarily inflammatory and is usually self-limiting. Symptoms may resolve on their own after radiotherapy is completed or paused. Mild cases can be observed and followed up, while symptomatic treatment can be provided for more severe cases. Anticholinergic medications such as oxybutynin and tolterodine can be used for patients with urinary frequency, urgency, incontinence, and increased nocturia. Frequently encountered adverse effects of these medications encompass symptoms such as oral dryness, gastrointestinal discomfort, residual urine after bladder voiding, and, in rare cases, urinary retention. For patients with difficulty urinating or incomplete dissolution, alpha-1 receptor blockers such as tamsulosin can be used. The most common side effect of these medications is orthostatic hypotension. Symptomatic pain relief can be provided for patients with painful urination, with nonsteroidal anti-inflammatory drugs (NSAIDs) being effective for most patients.22, 30 For acute radiation-induced bladder injury of grade ≥3, radiotherapy may be temporarily paused or stopped if necessary. Urinary tract infections often accompany acute radiation-induced bladder injury; antibiotics can be used for symptomatic treatment for patients with concurrent infections.
9.2 Late Radiation-induced Bladder Injury
Symptomatic treatment can be provided for late radiation-induced bladder injury with inflammation as the primary type, similar to acute radiation-induced bladder injury. Late radiation-induced bladder injury is often characterized by bleeding, with clinical manifestations ranging from microscopic hematuria to life-threatening bleeding. The following treatments can be considered:
9.2.1 General treatment
Symptomatic hemostatic treatment, such as tranexamic acid, can be given. For patients with a large amount of hematuria in a short period, it is essential to closely monitor vital signs, administer oral or intravenous fluid therapy if necessary, and be vigilant for shock due to insufficient blood volume. For patients with severe anemia, red blood cell transfusion may be required.30 It is advisable to instruct patients to maintain proper hydration by consuming ample water to ensure adequate urine output and perform bladder irrigation to prevent the formation of large blood clots. For patients with blood clots in the bladder, a catheter can be inserted for intermittent or continuous bladder irrigation.30 Active anti-infection treatment should be administered for patients with confirmed concurrent urinary tract infections.
Recommendation: It is recommended to use symptomatic hemostatic treatment, fluid replacement, blood transfusion (when necessary), and bladder irrigation as the initial treatment methods for patients with late radiation-induced bladder injury and bleeding. Recommendation strength: Strong; Evidence quality: Low.
9.2.2 Bladder Instillation
9.2.2.1 Aluminum salts
Agents like alum can cause protein precipitation on cell surfaces and within tissue gaps, preventing capillary bleeding in patients with less severe bleeding. The efficacy of aluminum salt bladder instillation for severe bleeding is 50% to 66%.31, 32 In cases of significant bleeding, the residues can quickly thicken, leading to clot retention, expansion, and aggravated bleeding. Local side effects include suprapubic pain and urinary urgency, which can be controlled with antispasmodics and analgesics. There have been reports of encephalopathy in patients with renal failure after aluminum salt bladder instillation, so kidney function should be assessed before treatment.33, 34 Alum salt (e.g., potassium alum) can be dissolved in a saline solution with a concentration of 1% (50 g in 5000 mL) and then instilled into the bladder at a rate of 250 to 300 mL/h.35
Recommendation: For patients with poor initial treatment outcomes, it is recommended to use bladder instillation of alum salt to treat late radiation-induced bladder injury. Recommendation strength: Strong; Evidence quality: Moderate.
9.2.2.2 Formalin
Formalin bladder instillation can cause protein precipitation in bladder mucosal cells and has a coagulating and fixing effect on dilated capillaries, thereby alleviating bladder bleeding in late radiation-induced bladder injury. After formalin bladder instillation, bleeding resolves in 70% to 90% of patients.35, 36 Formalin can also cause the fixation of bladder muscle tissue, leading to bladder contractions and reduced capacity; fixation of the ureteral tissue may result in ureteral obstruction, potentially causing hydronephrosis and renal failure. Reflux of formalin into the ureters may cause bilateral pyelonephritis and severe sepsis.
With the advancement of endoscopic techniques, the importance of formalin bladder instillation is decreasing. Therefore, formalin bladder instillation is recommended only for patients whose bladder has lost function due to urinary diversion.30 or for refractory severe radiation-induced bladder injury patients who have failed other conservative treatments to be used as a last resort before surgical intervention.
Before formalin bladder instillation, bladder imaging should be performed to rule out bladder-ureteral reflux to prevent severe adverse reactions from formalin reflux into the ureters and kidneys.36 For patients with bladder-ureteral reflux, instillation can be considered after placing an occlusive balloon in the ureter.15 Due to the significant pain sensation, it is recommended that formalin bladder instillation be performed under anesthesia, either general or regional.36 Dilute formalin to a concentration of 1% to 10% and instill it into the bladder through a catheter. It is recommended to retain the solution for about 15 minutes before draining through the catheter, followed by bladder irrigation with saline.
Recommendation: Formalin bladder instillation effectively treats bleeding in radiation-induced bladder injury but carries significant complications. It is only recommended for patients whose bladder has lost function due to urinary diversion or for refractory severe radiation-induced bladder injury patients who have failed other conservative treatments to be used as a last resort before surgical intervention. Recommendation strength: Weak; Evidence quality: Low.
9.2.2.3 Recombinant human granulocyte-macrophage colony-stimulating factor
-
Recombinant human granulocyte-macrophage colony-stimulating factor (GM-CSF) has a multilineage cell-promoting effect. In addition to promoting neutrophil development, it also stimulates the release of wound healing-related factors, promotes the migration and proliferation of mucosal epithelial cells, induces keratinocytes to enter a regenerative state, and activates fibroblasts to promote granulation tissue formation and mucosal healing.37 Studies have shown that GM-CSF effectively treats refractory grade III-IV hemorrhagic cystitis.38-40 Generally, 400 μg of GM-CSF is dissolved in 5–10 mL of saline and injected into the bladder, followed by flushing the catheter with 5–10 mL of saline. The solution is retained for 30–120 minutes (depending on patient tolerance) before being drained, and then continuous saline bladder irrigation is performed for at least 5 days or until symptoms improve.
- Recommendation: Recombinant human granulocyte-macrophage colony-stimulating factor can relieve grade III-IV hemorrhagic cystitis bleeding and is suggested for refractory radiation-induced cystitis when conventional treatments fail. Recommendation strength: Weak; Evidence quality: Very low.
9.2.2.4 Traditional Chinese Medicine
Traditional Chinese Medicine (TCM) has accumulated some clinical evidence in treating radiation-induced bladder injury.41-43 According to TCM theory, radiation is considered a “hot and toxic” pathogen that depletes qi and injures yin, leading to a loss of body fluids and gastrointestinal heat accumulation.41 Clinical reports have shown effective treatment of chronic radiation-induced cystitis with methods that nourish yin, clear heat, and cool blood.43 Further clinical trials are needed to verify these medications' role in treating radiation-induced bladder injury.
Recommendation: It is suggested to use TCM based on syndrome differentiation for radiation-induced bladder injury. Recommendation strength: Weak; Evidence quality: Very low.
9.2.3 Electrocoagulation/ablation under cystoscopy
For hemorrhagic bladder injuries unresponsive to conservative measures, electrocoagulation or ablation of bleeding points under cystoscopy is an effective treatment method. Common techniques include electrocoagulation, argon gas, and laser therapy. Potential complications include bladder perforation and fistula formation, but the treatment is often less effective in patients with more severe hemorrhagic cystitis.44
Recommendation: Electrocoagulation/ablation under cystoscopy is recommended for radiation-induced bladder injury with bleeding unresponsive to conservative treatment. Recommendation strength: Strong; Evidence quality: Very low.
9.2.4 Hyperbaric Oxygen Therapy
Hyperbaric oxygen therapy (HBOT) is a treatment method that involves inhaling 100% oxygen at pressures greater than 1 atmosphere. Hyperbaric chambers provide conditions for complete hemoglobin saturation, with oxygen dissolving at very high concentrations in plasma. HBOT can promote angiogenesis and fibroblast activity in damaged tissues, facilitate tissue repair, and correct ischemic injuries secondary to radiation.45 Compared to other therapies, such as formalin and silver nitrate bladder instillation, HBOT does not cause structural or functional damage to the bladder and can be considered a viable treatment choice for individuals suffering from radiation-induced bladder injuries unresponsive to conventional treatments. A randomized controlled study showed that HBOT could improve symptoms of radiation-induced cystitis compared to standard therapy.46 The overall effectiveness rate of HBOT for radiation-induced cystitis is 87.3%, with a complete remission rate of 65.3%44; the complication rate is 9.6%, with common complications including ear pain and visual disturbances. The incidence of permanent or severe complications is very low.45
There is no consensus on the HBOT protocol for treating radiation-induced bladder injury. Literature-based protocols often involve pressures of 1.8 to 2.5 atmospheres for 60 to 120 minutes once per day, with a total of 20 to 40 treatments.45 Some literature recommends pressures ≥2.4 atmospheres, ≥90 minutes of 100% oxygen inhalation, and a total of ≥40 treatments.47
Recommendation: HBOT is recommended for treating late radiation-induced bladder injury and can be combined with other treatment methods. Recommendation strength: Strong; Evidence quality: High.
9.2.5 Surgery
Surgery can be considered a treatment option for severe radiation-induced bladder injuries that do not respond to conventional treatments.48, 49 Surgical options include (1) selective embolization or ligation of the internal iliac artery; (2) percutaneous nephrostomy; (3) percutaneous ureterostomy or intestinal conduit; (4) cystectomy.
Selective embolization or ligation of the iliac artery can effectively alleviate bladder bleeding in patients and further clarify the bleeding vessels through interventional angiography, allowing for selective embolization.50
Urinary diversion may be considered for intractable severe radiation-induced bladder injuries, including methods such as percutaneous nephrostomy, ureterostomy, and transverse colonic conduit.48 Among these, intestinal conduits are the preferred method, using a transverse colon or non-irradiated ileum and ureters for urinary diversion. In patients undergoing urinary diversion, more than 50% experience complications related to a functionally deficient bladder, including sepsis, bleeding, and pain. Most patients still require cystectomy after urinary diversion, and concurrent cystectomy may be considered during urinary diversion.51
Recommendation: Surgery is recommended for patients with severe radiation-induced bladder injuries and bladder fistulas when non-surgical treatments are ineffective. Recommendation strength: Strong; Evidence quality: Low.
9.2.6 Treatment selection process
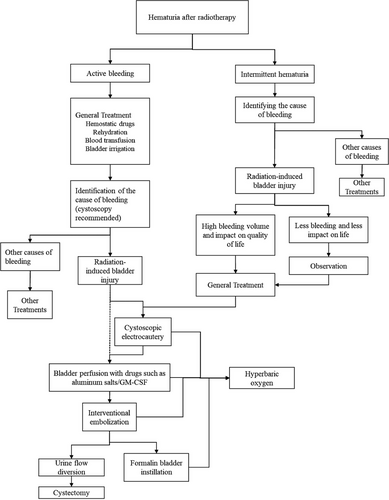
General treatments can be administered initially for patients with bleeding as the primary symptom, including hemostatic drugs, oral or intravenous rehydration, blood transfusion (if necessary), and bladder irrigation. After stabilizing the patient's general condition, it is necessary to investigate the cause of bleeding, excluding upper urinary tract bleeding and bladder tumors, and a cystoscopy examination is suggested. After confirming the diagnosis of radiation-induced bladder injury bleeding, electrocoagulation under cystoscopy can be performed to control bleeding. If electrocoagulation/ablation is not feasible or ineffective, bladder instillation of aluminum salts can be conducted. If these treatments fail, embolization can be performed. Urinary diversion surgery can be considered if severe bleeding persists after the above treatments. If possible, hyperbaric oxygen therapy is recommended to be combined with the treatments.22, 30, 35 The recommended treatment work flow were show in Figure 2.
Recommendation: A step-by-step management approach is suggested to treat non-life-threatening radiation-induced bladder injuries. Based on the efficacy, side effects, accessibility, and patient acceptance of different treatment methods, individualized treatment should be adopted. Recommendation strength: Weak; Evidence quality: Very low.
10 CONCLUSION
The diagnosis and treatment of radiation-induced bladder injury require multidisciplinary involvement. This guideline summarizes current research and clinical experience, aiming to guide the prevention, diagnosis, and treatment of radiation-induced bladder injury. Current research on radiation-induced bladder injury is limited, and most treatment methods lack high-level evidence. The treatment principles proposed in this guideline aim to provide support and reference for clinical decision-making, and their clinical use should be combined with the actual situation of patients and the clinical experience of different institutions.
ACKNOWLEDGMENTS
Guiding experts: Jinming Yu (Shandong Cancer Hospital).
Writing experts: Weiping Wang, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College; Fuquan Zhang, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College
Editorial Board Members: (Alphabetize by Last Name)
Weiqing Chen, Chongqing University Cancer Hospital
Xiaozhong Chen, Zhejiang Cancer Hospital
Yan Cheng, First Affiliated Hospital of Zhengzhou University
Mei Feng, Sichuan Third People's Hospital
LiYing Gao, Gansu Provincial Cancer Hospital
Xianshu Gao, Peking University First Hospital
Yuanhong Gao, Sun Yat-sen University Cancer Center
Xia He, Jiangsu Cancer Hospital
Man Hu, Shandong Cancer Hospital
Xiaobo Huang, Sun Yat-Sen Memorial Hospital
Baosheng Li, Shandong Cancer Hospital
Guiling Li, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology
Jie Li, Shanxi Provincial Cancer Hospital
Jingao Li, Jiangxi Provincial Cancer Hospital
Qin Lin, The First Affiliated Hospital of Xiamen University
Fang Liu, The People's Liberation Army General Hospital
Qing Liu, The Third Affiliated Hospital of Air Force Medical University
Zi Liu, The First Affiliated Hospital of Xi'an Jiaotong University
Tenghui Ma, The Sixth Affiliated Hospital of Sun Yat-sen University
Shuhuai Niu, The Fourth Hospital of Hebei Medical University
Qiao Qiao, The First Affiliated Hospital of China Medical University
Jianguang Qiu, The Sixth Affiliated Hospital of Sun Yat-sen University
Mei Shi, Xijing Hospital of Air Force Military Medical University
Hui Wang, Hunan Cancer Hospital
Jun Wang, The Fourth Hospital of Hebei Medical University
Qifeng Wang, Sichuan Cancer Hospital
Rensheng Wang, The First Affiliated Hospital of Guangxi Medical University
Ruozheng Wang, Cancer Hospital Affiliated to Xinjiang Medical University
Weiping Wang, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College
Sangang Wu, The First Affiliated Hospital of Xiamen University
Qin Xu, Fujian Provincial Cancer Hospital
Junlin Yi, The Cancer Hospital of Chinese Academy of Medical Sciences
Shuanghu Yuan, Shandong Cancer Hospital
Xianglin Yuan, Tongji Hospital of Tongji Medical College, Huazhong University of Science and Technology
Daxin Zhang, the First Affiliated Hospital of Harbin Medical University
Fuquan Zhang, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College
Liyuan Zhang, The Second Affiliated Hospital of Soochow University
Yunyan Zhang, Harbin Medical University Cancer Hospital
Zhen Zhang, Fudan University Shanghai Cancer Center
Anping Zheng, Anyang Tumor Hospital
Li Zhu, Tianjin Medical University Cancer Institute and Hospital
Hongqing Zhuang, Peking University Third Hospital
Dongling Zou, Chongqing University Cancer Hospital
CONFLICTS OF INTEREST STATEMENT
Jinming Yu is the Editor-in-Chief of the journal and co-author of this article. He was excluded from the peer-review process and all editorial decisions related to the acceptance and publication of this article. Peer review was handled independently by the other editor to minimize bias.
ETHICS STATEMENT
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part are appropriately investigated and resolved.