Assessment of dose-volume histogram statistics using three-dimensional conformal techniques in breast cancer adjuvant radiotherapy treatment
Abstract
Objective
Breast cancer (BC) is first of the top 10 malignancies in Iraq. Dose-volume histograms (DVHs) are most commonly used as a plan evaluation tool. This study aimed to assess DVH statistics using three-dimensional conformal radiotherapies in BC in an adjuvant setting.
Methods
A retrospective study of 70 histologically confirmed women diagnosed with BC was reviewed. The study was conducted between November 2020 and May 2021, planning for treatment with adjuvant three-dimensional conformal radiotherapies. The treatment plan used for each woman was based on an analysis of the volumetric dose, including DVH analysis.
Results
The planning target volume and clinical target volume coverage for tumors at V85% was better than V90% and V95%, with highly significant differences (p < 0.0001). The planning target volume and clinical target volume coverage for lymph nodes at V85% was higher than V90% and V95%, with no significant differences.
Conclusions
This is the only study that has been carried out in Iraq that we are aware of that addresses the evaluation of DVH statistics in BC. V85% produced the best chest wall coverage, and V95% made the worst. With little significance, higher lymph nodes coverage was attained at V85%, whereas the lowest coverage was at V95%.
1 INTRODUCTION
Breast cancer (BC) is the most common cancer among women, representing approximately 24.5% of new cases of female cancers worldwide. GLOBOCAN reported 2,261,419 new cases of BC (rank #1), with 684,996 deaths from BC (rank #4) in 2020.1 In Iraq, there were 3845 cases estimated in 2011.2 This number rose to 4542 in 2014 according to a World Health Organization report.3 In contrast, the new cases of BC in 2020 were 7515.1 It has been demonstrated that adjuvant radiation administered after BC surgery reduces mortality by 5%, and the risk of locoregional recurrence from 30% to 10% after 20 years. Current trials assess the role of radiation therapy (RT), a conventional treatment for ductal carcinoma in situ, in low-risk individuals compared with surgery alone.4-6
The normal tissue dose distributions are calculated using dose-volume histograms (DVHs). DVHs are frequently used to evaluate plans to compare dosages from various plans or structures. Different amounts of damage are caused by the dose heterogeneity in the exposed volume, but the organ's structure and function ultimately determine the pathophysiological outcome.7, 8 The large amount of dosimetric data that must be analyzed when a three-dimensional conformal radiotherapies (3DCRT) plan is evaluated has prompted the development of methods of condensing and presenting the data in more easily understandable formats.9, 10 Two types of DVHs, differential and cumulative, are available in 3DCRT planning. The latter is widely used in plan evaluation for assessing planning target volume (PTV) coverage and dose to organs at risk (OARs).11, 12
The present study aimed to assess DVH statistics using 3DCRT in an adjuvant setting, analyze DVH for all OARs per-patient basis, and evaluate comparative dose distributions for gross target volume (GTV), clinical target volume (CTV), PTV, and OAR on DVH using adjuvant 3DCRT for BC treatment.
2 PATIENTS AND METHODS
2.1 Study design and setting
A total of 70 histologically confirmed female patients with BC were treated in the Baghdad Radiation Oncology Center, located in Baghdad Medical City, Iraq. Between November 2020 and May 2021, the survey was carried out in preparation for adjuvant 3DCRT therapy.
2.2 Data collection
Reviewing medical records allowed for the retrospective collection of data. Age; tumor, node, and metastasis (TNM) staging;, histology; tumor side; patient address; dose; and the number of RT fractions were the variables examined. Imaging tests (conventional radiography, computed tomography, or magnetic resonance imaging) were used to determine the clinical stage of BC, and a tissue sample was used to corroborate the results.
2.3 DVH
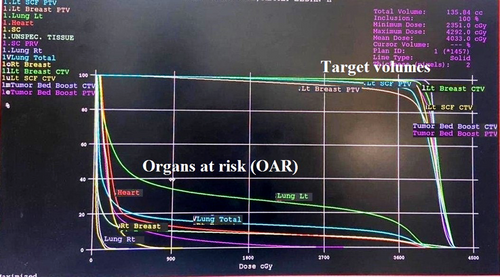
A treatment strategy was developed for each patient based on a volumetric dose study, which included DVH analysis of the PTV and important normal tissues. Beam weights were manually adjusted to maintain a hot spot of 107% while covering the PTV by the iso-dose line at 95%. The protocol was developed with dose-volume restrictions, including dose restrictions to the ipsilateral and contralateral lung, contralateral breast, heart, liver, and spinal cord (Figure 1).
2.4 Target volumes and OARs data
- a) PTV t volume % covered by 85% dose
- b) PTV t volume % covered by 90% dose
- c) PTV t volume % covered by 95% dose
- d) PTV n volume % covered by 85% dose
- e) PTV n volume % covered by 90% dose
- f) PTV n volume % covered by 95% dose
- g) CTV t volume % covered by 85% dose
- h) CTV t volume % covered by 90% dose
- i) CTV t volume % covered by 95% dose
- j) CTV n volume % covered by85% dose
- k) CTV n volume % covered by 90% dose
- l) CTV n volume % covered by 95% dose
- a) For the lung (each for right and left)
-
Mean dose
-
Volume percentage received 2000 cGy
-
Volume percentage received 1000 cGy
-
Volume percentage received 500 cGy
- b) For the heart
-
Volume percentage received 2500 cGy
-
Mean dose
- c) For the liver
-
Mean dose
-
Volume percentage received 3000 cGy
- d) Spinal cord (mean dose)
- e) Contralateral breast (mean dose)
2.5 Equipment
These included computed tomography pore scanner (85 cm; Philips 16 series), Linear Accelerator (Infinity and Synergy); 2013 (core beam computed tomography), Monaco Elekta HP version 5, and XiO Elekta system version 5.
2.6 Radiotherapy doses
- a) 4005 cGy in 15 fractions over 3 weeks was adopted as standard practice in radiotherapy dosing for women undergo mastectomy.
- b) 4005 cGy/15 fractions/3 weeks performed for patients with BCS plus 1000 cGy/5 fractions/1 week as booster dosing.
2.7 Statistical analysis
All analyses were conducted using SPSS 15.0 (SPSS Inc., Chicago, Illinois, USA). A two-sided p-value of ≤0.05 was considered statistically significant for Fisher's exact, Pearson's χ2-test, Monte Carlo two-sided, and Spearman's correlation. Numbers and percentages of replies in each category made up the descriptive statistics. The one-way ANOVA test for independent measurements was intended to simultaneously compare the means of six separate portal images. The post-hoc Tukey's honestly significant difference (beta) approach made comparing two ANOVA datasets more accessible, and distinguished between the six portal image means.
3 RESULTS
The mean age of studied women was 50.97 ± 11.34 years, with 50 years as the median, and most women were aged 40–49 years (n = 23; 32.90%), followed by 50–59 years (n = 21; 30.00%). In addition, the 30–39 years and 60–69 years age group reported 10 (14.30%) patients. Age more than 70 years was recorded in five women.
Table 1 shows that BC on the left side was documented more than the right side (52.90 vs. 47.10%). The T2 stage was predominant in 45 (64.30%) patients, followed by T1 in 11 (15.71%) patients. The N1 and N2 stages were mostly found in 30 (42.85%) and 25 (35.70%) patients, respectively. Approximately 58 of 70 (82.90%) patients underwent modified radical mastectomy surgery, whereas 12 of 70 (17.10%) patients were surgically treated by BCS. Most patients , 51 of 70 (72.85%), received a RT dose of 40.05 Gy/15fx. Other doses described were 42.56 Gy/16fx and 50 Gy/25fx in 15.7% and 11.4%, respectively. Only six women received a booster dose of 10 Gy/5fx.
| Variables | n | % | |
|---|---|---|---|
| Side | Right | 33 | 47.10 |
| Left | 37 | 52.90 | |
| T staging | T1 | 11 | 15.71 |
| T2 | 45 | 64.30 | |
| T3 | 5 | 7.14 | |
| T4 | 9 | 12.85 | |
| N staging | N0 | 9 | 12.85 |
| N1 | 30 | 42.85 | |
| N2 | 25 | 35.70 | |
| N3 | 6 | 8.60 | |
| Surgery types | MRM | 58 | 82.90 |
| BCS | 12 | 17.10 | |
| RT dose (cGy/fx) | 4005/15fx | 51 | 72.85 |
| 4256/16fx | 11 | 15.71 | |
| 5000/25fx | 8 | 11.43 | |
| Only six patients received booster dose of 1000 cGy/5fx | |||
- Abbreviations: BCS, breast conservative surgery; cGy, centi-gray; fx, fraction; MRM, modified radical mastectomy; N, lymph node; RT, radiotherapy; T, tumor.
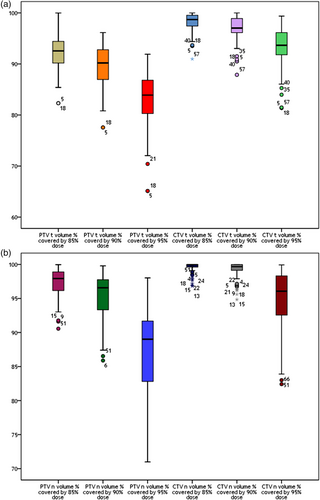
The dosimetry of this study is shown in Table 2 and Figure 2. The PTV coverage for tumor at V85% (92.08 ± 3.55, p < 0.0001) was better than V90% (89.60 ± 4.12, p < 0.0001) and V95% (82.83 ± 5.90, p = 0.006), with a high significant difference regarding the post-hoc Tukey's test (16.56, 12.15, and 4.41), respectively, and ANOVA analysis (73.55, p < 0.0001). The PTV coverage for lymph nodes at V85% (97.20 ± 2.25, p = 0.97) was higher than that at V90% (95.40 ± 3.23, p = 0.98) and V95% (87.14 ± 6.70, p = 0.10), with no significant differences (p = 0.968). CTV coverage for tumor at V85% (98.10 ± 1.90, p < 0.0001) was higher than that at V90% (96.93 ± 2.55, p < 0.0001) and V95% (93.14 ± 4.16, p = 0.058), with high significant differences regarding the post-hoc Tukey's test (13.73, 10.48, 3.25), respectively, and ANOVA analysis (51.50, p < 0.0001). The CTV coverage for lymph nodes at V85% (99.54 ± 0.82, p = 0.99) was more than that at V90% (99.10 ± 1.33, p = 0.99) and V95% (94.60 ± 4.57, p = 0.99), with no significant association (p = 0.99).
| Parameters | V% | Coverage (%) | Maximum coverage (%) | Minimum coverage (%) | Post-hoc Tukey HSD (p-value) | ANOVA (p-value) |
|---|---|---|---|---|---|---|
| PTVt volume % covered | 85% | 92.08 ± 3.55 | 99.98 | 82.31 | 16.56 (<0.0001) | 73.55 (<0.0001) |
| 90% | 89.60 ± 4.12 | 96.15 | 77.55 | 12.15 (<0.0001) | ||
| 95% | 82.83 ± 5.90 | 91.90 | 65.12 | 4.41 (0.006) | ||
| PTVn volume % covered | 85% | 97.20 ± 2.25 | 99.97 | 90.56 | 0.33 (0.97) | 0.03 (0.968) |
| 90% | 95.40 ± 3.23 | 99.79 | 85.88 | 0.27 (0.98) | ||
| 95% | 87.14 ± 6.70 | 98.02 | 70.99 | 0.06 (0.1) | ||
| CTVt volume % covered | 85% | 98.10 ± 1.90 | 100 | 90.97 | 13.73 (<0.0001) | 51.50 (<0.0001) |
| 90% | 96.93 ± 2.55 | 100 | 87.87 | 10.48 (<0.0001) | ||
| 95% | 93.14 ± 4.16 | 99.38 | 81.37 | 3.25 (0.058) | ||
| CTVn volume % covered | 85% | 99.54 ± 0.82 | 100 | 96.83 | 0.17 (0.99) | 0.008 (0.99) |
| 90% | 99.10 ± 1.33 | 100 | 94.84 | 0.15 (0.99) | ||
| 95% | 94.60 ± 4.57 | 99.93 | 82.41 | 0.02 (0.99) |
- Abbreviations: CTV, clinical target volume; n, lymph node; PTV, planning target volume; SD, standard deviation; t, tumor; V, volume.
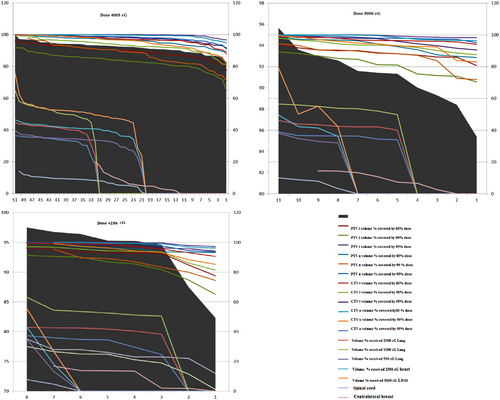
The dosimetry of OAR in this investigation is shown in Table 3. The right (ipsilateral) lung received an overall mean (median) dose of 750 (125) cGy. In addition, the lung received 2000 cGy in 15.80% of patients, 1000 cGy in 19.29%, and 500 cGy in 24.68% of patients. The left (ipsilateral) lung received an overall mean (median) dose of 786.9 (905) cGy. In addition, in 17.22% of patients, the lung received 2000 cGy; in 20.90%, it received 1000 cGy; in 26.8%, it took 500 cGy. The overall mean (median) dose received by the heart was 338.1 (324) cGy, with a maximum dose reaching 889 cGy, whereas in 12.43% of patients, the heart received 2500 cGy during the course. The overall mean dose received by the liver was 398.31 cGy, with the maximum dose reaching 1021 cGy, whereas 5.80% received 3000 cGy during the course. Accordingly, the overall mean dose received by the spinal cord was 1590 cGy, and the overall maximum dose reached 3534 cGy. Finally, the overall mean dose received by the contralateral breast during RT was 31.14 cGy, and the overall maximum dose received 181 cGy. The results presented here suggested that the RT dose of 4005 cGy had been better for covering target volumes (PTV and CTV) and the lowest doses received by different OARs than doses of 5000 cGy and 4256 cGy, respectively, as shown in Figure 3, which is acceptable for efficacy and safety.
| OARs | Parameters | Volume %/mean dose (cGy) (median) | Maximum dose received | Minimum dose received |
|---|---|---|---|---|
|
Rt lung (ipsilateral) (V30% ≤17%) |
Mean dose (cGy) | 750 (125) | 1861 | 27 |
| 2000 cGy | 15.80% | 38.90% | 0 | |
| 1000 cGy | 19.29% | 46.14% | 0 | |
| 500 cGy | 24.68% | 64.80% | 0 | |
|
Lt lung (ipsilateral) (V30% ≤17%) |
Mean dose (cGy) | 786.90 (905) | 1851 | 0 |
| 2000 cGy | 17.22% | 39.77% | 0 | |
| 1000 cGy | 20.90% | 49.50% | 0 | |
| 500 cGy | 26.80% | 79.03% | 0 | |
|
Heart (V25% ≤5%) (V5% ≤30%) |
Mean dose | 338.10 (324) | 889 | 0 |
| 2500 cGy | 12.43% | 13.99% | 0 | |
|
Liver (V70% < 20G) |
Mean dose | 398.31 (343) | 1021 | 0 |
| 3000 cGy | 5.80% | 19.80% | 0 | |
|
Spinal cord (Dmax <45 G) |
Mean dose (cGy) | 1590 (1496.5) | 3534 | 58 |
| Contralateral breast | Mean dose (cGy) | 31.14 (23.5) | 181 | 9 |
- Abbreviations: cGy, centi-gray; Dmax, maximum dose; Lt, left; OARs, organs at risk; Rt, right; V, volume.
4 DISCUSSION
By administering various adjuvant RT doses to 70 Iraqi patients with BC, the present study demonstrates our continuous clinical expertise in 3DCRT therapy of BC in Iraq. Although there are no apparent uncertainties in the OAR dose determination during RT, this is acceptable. These findings also assist the ongoing research on 3DCRT delivery in our region. The findings confirm several other studies conducted in Iraq.13-17 Age is an essential factor in the occurrence and management of BC.18 In the research comparing women from Iraq and Britain, the mean age was higher by over 15 years than what the present results showed. BC was also more prevalent than we had previously estimated among USA women in their sixth decade of life. According to our study, women aged under 50 years were more likely to be diagnosed with BC in most Arabian nations than women aged over 50 in the USA.18
The tumor characteristics in the present study revealed that left BC was documented more than the right. The T2 stage was predominant, and N1 and N2 stages were mostly found. Most patients underwent modified radical mastectomy surgery, whereas the rest were surgically treated with BCS. Similarly, data mentioned by Al-Naqqash et al.,13 Al-Alwan et al.,15 and Al-Rawaq,16 differ from the results recorded by Goldhirsch et al.19 and Al-Khafaji.20 These are crucial in BC, as the existence and quantity of affected axillary lymph nodes highly correlate with the likelihood of distant metastasis, disease-free survival, and overall survival, all of which are strongly predicted by the tumor size. It serves as a separate prognostic factor. The strongest indicator of systemic micrometastases and the most significant prognostic factor, the lymph node status, is directly associated with survival.21-24
In the present study, the protocols utilized to treat those women apply according to international guidelines and trials.4-7, 25-29 Most patients received a RT dose of 40.05 Gy/15fx. Other doses described were 42.56 Gy/16fx and 50 Gy/25fx. Only six women (8.6%) received a booster dose of 10 Gy/5fx. Long-term follow-up shows that early BC patients can receive hypofractionated radiation safely and effectively dosed.28 When 2236 women were enrolled in START-A in 2013, it was discovered that moderate or marked breast induration, telangiectasia, and breast edema were significantly less common in the 39 Gy group than in the 50 Gy group. The median follow-up was 9.3 years (IQR 8.0–10.0), during which 139 local or regional relapses occurred.29 In 2013, the START-B found that breast shrinkage, telangiectasia, and breast edema were significantly less common normal tissue effects in the 40 Gy group than in the 50 Gy group. All these were obtained from 2215 enrolled women with a median follow-up of 9.9 years (IQR 7.5–10.1), after which 95 local-regional relapses had occurred.29 Also, there is increasing interest in adjuvant breast RT with fewer and larger fractions.26, 27 The FAST trial randomized 915 women (age >50 years) with node-negative BC to either 50 Gy in 25 fractions or 28.5 Gy or 30 Gy in five once-weekly fractions of 5.7 Gy or 6.0 Gy. At 3 years of follow-up, the 28.5 Gy arm was comparable with 50 Gy in 25 fractions, but the 30 Gy fractionation was adversely affected. The FAST-Forward trial has completed the recruitment of 4000 women. This randomized trial of women compared a scheme of 40 Gy in 15 fractions with two other schedules, 27 Gy in five fractions over 1 week or 26 Gy in five fractions over 1 week.29 The proportional gain from RT will be more significant for women irradiated today, because radiotherapy planning has changed, and women with BC today receive better coverage of target areas.26, 27, 29 Furthermore, doses to normal tissues are lower today, so the risks of radiotherapy are also likely to be lower. The techniques have been improved over the past few decades, so radiotherapy's proportional benefits are likely to be larger.30
The dosimetry of the present study revealed that the PTV coverage for the breast tumor bed at V85% was better than that at V90% and V95%. The CTV coverage for the tumor bed at V85% was higher than that at V90% and V95%, whereas CTV coverage for lymph nodes at V85% was more than that at V90% and V95%, with no significant association according to ANOVA analysis. Due to the lack of such studies in Iraq, the comparison with several studies from other countries is unenviable.
Ohashi et al.31 documented breast and axillary dosimetric parameters. They found no significant differences in the variability of the V90% and V95% values. The mean volumes of V90% and V95% rose significantly with 3DCRT, which disagreed with our findings. When RT is intended to treat the BC bed and axillary areas, an appropriate technique is applied to reduce locoregional recurrence rates.32, 33 Their findings concluded that PTV and normal tissue are unaffected by the number of beams. To lessen the scattered radiation, medical physicists must therefore carry out the optimal strategy without using more beams than necessary.34
In a study conducted in Egypt, researchers discovered that the target was better covered, and the mean of V95% was more significant, although not considerably, after adding more beams (p = 0.9152). Additionally, even though the intensity-modulated RT was more advanced, they only used two tangential fields in the 3DCRT approach compared with five to seven fields in the intensity-modulated RT technique, making the V95% difference inconsequential (p = 1.000).35
The availability of DVH allows radiophysicists and radiation oncologists to virtually explore different tentative plans, and perform successive modifications of a starting plan for each RT. However, the choice of treatment plans is mainly made by side-to-side comparison of DVHs and isodose curves for each tentative schedule. As differences between them are minor, any selection made by inspection, as is generally the case, may not be easy to justify on clinical terms.36
DVH data are generally analyzed within a treatment planning system (TPS) per-patient basis, with an evaluation of single-plan or comparative dose distributions. Meticulous structure-by-structure review is performed on this data during initial and iterative plan evaluation and quality assessment (per physician prescription and treatment goals), applying structure-specific dose constraints. However, the correlation of dosimetric data with clinical information outside of the TPS (e.g., treatment response or follow-up toxicity) remains a significant hurdle for many clinical and research-related inquiries. Moreover, TPS software is generally unable to perform comparative dosimetry simultaneously among a cohort of patients.37
The overall mean dose received by the right lung was 750 cGy, whereas 15.80%, 19.29%, and 24.68% received 2000, 1000, and 500 cGy, respectively. In the left lung, the mean dose was 786.9 cGy, and 17.22% received 2000 cGy, 20.90% received 1000 cGy, and 26.80% received 500 cGy. Generally speaking, 12.43% of the heart received 2500 cGy during the RT course, and 5.80% of the liver received 3000 cGy. Accordingly, the overall mean dose received by the spinal cord was 1590 cGy. Finally, the overall mean dose received by the contralateral breast during RT was 31.14 cGy, which is seemly slightly above the findings of Benson et al.,37 who recorded that the ipsilateral lung V30% should be kept at ≤17%, and V25% of the heart kept at ≤5% and V5% of the heart kept at ≤30%.
Ohashi et al.31 investigated the dosimetric parameters for the heart, lungs, and other organs. Whole OARs showed dropped doses with the 3DCRT plan. Heart dose minimizing is a concern for BC on the left side. If the heart receives <30 Gy, the cardiac complications are likely to be lower,37, 38 which supports the present study's results.
Pneumonitis rates in BC treated with standard tangential fields are low and are thus clinically acceptable.39 Radiation to the axillary area increases the lung volume irradiated,32 which may increase the probability of pneumonitis.40 Marks et al.41 showed that V20% and DVHs of the lung for all patients were acceptable.
The statistical analyses of the heart and lung doses were carried out for only 11 left-sided patients in a study in Egypt. The complication of normal tissue in group b of the heart was lower than in group a, meaning there was no significant association.34 The main issue with average tissue dose raise of this magnitude is an elevated late secondary malignancy risk.31, 41, 42
Also, Hall and Gao et al.42, 43 discussed this subject again and found to be as it was the most significant issue with a low risk for systemic relapse. There was a report that adjuvant RT may increase the chances of lung cancer and angiosarcoma.42, 44, 45 The study of Chitapanarux et al. agrees with the present findings regarding the mean value of the lung (16.4 ± 2.8), which is close to the current research (18.11 ± 1.722) and slightly beyond the value of more fields.46
5 CONCLUSIONS
To our knowledge, this is the first study carried out in Iraq that discusses the examination of DVH statistics when 3DCRT adjuvant is used to treat BC. It also evaluated comparative dose distributions and carried out a per-patient analysis of DVH for all OARs. Planning BC RT can be made more accessible, effective, informative, and accurate by using DVH. The RT dose of 40.05 Gy/15fx gave more outstanding coverage of the target volumes (PTV and CTV) compared with 50 Gy/25fx and 42.56 Gy/16fx, and the lowest doses received by diverse normal tissues. V85% provides the best chest wall coverage, whereas V95% provides the least. With no significance, better coverage of lymph nodes is obtained at V85%, and the lowest coverage at V95%. Significant RT doses result in high tumor bed and lymphatic coverage, but they may also be more hazardous to normal tissues.
6 LIMITATION
A limitation of the present study are the small number of patients, and the study not clarify the details of the treatment plans, this could be helpful for carrying out a future study on this topic in Iraq.
CONFLICT OF INTEREST
The authors declare that they have read the article and there are no competing interests.
ETHICS STATEMENT
The Medical Ethical Committee of College of Medicine/Baghdad University approved this study (code; 935 in 01/12/2020).