Risk factors of dermatitis during radiation for vulvar carcinoma
Xue Teng and Xian Zhang contributed equally to this work and should be considered as co-first authors.
Funding information: National Natural Science Foundation of China, Grant/Award Number: 71804073
Abstract
Radiodermatitis, inflammatory lesions of skin and mucosa caused by radiation, is a common adverse effect during the radiation therapy of vulvar carcinoma. The incidence of radiodermatitis is affected by various factors, and the purpose of this study was to investigate the risk factors of radiodermatitis in patients with vulvar carcinoma. Patients with vulvar tumors who received radiotherapy from January 2015 to December 2020 were included in this retrospective study. Radiodermatitis was graded according to the grading criteria of the American Center for Radiological Oncology, and then univariate analysis and logistic multivariate regression analysis were used to determine the risk factors of radiodermatitis. A total of 60 eligible patients were enrolled, including 3 (5%), 25 (41.7%), 28 (46.7%), and 4 (6.6%) patients with grade 0, 1, 2, and 3 radiodermatitis, respectively. Univariate analysis showed that the incidence of radiodermatitis was significantly correlated with age, therapeutic strategy, pathological stage and radiotherapy dose (p < .05). Multivariate regression analysis indicated that age, therapeutic strategy and radiotherapy dose were independent risk factors for radiodermatitis (p < .05). In the current study, we identified the independent risk factors for radiodermatitis in patients with vulvar carcinoma were age, therapeutic strategy and radiotherapy dose, which might be conducive to identify high-risk patients, so as to adjust their treatment plan in time and reduce the risk of radiation-induced skin toxicity.
1 INTRODUCTION
Radiation dermatitis, a common and predominant sequela in patients undergoing radiotherapy, which might occur as acute or late side effect, and up to 95% of those patients would develop moderate to severe cutaneous reaction, including moist desquamation, ulceration and even necrosis and bleeding.1 Once acute radiodermatitis occurs, and the patients do not receive timely and effective symptomatic treatments, it is highly likely to lead to the interruption of radiotherapy, and thus play negative impacts on the tumor control and patients' prognosis.2 Therefore, it is necessary to predict the risk of radiodermatitis efficiently and accurately. The occurrence of radiodermatitis depends on multiple factors which may be intrinsic (i.e., patient-related) or extrinsic (i.e., treatment-related). It has been reported that skin often develops erythema when exposed to the radiation of 20–40 Gy, while blisters, wet desquamation and even infection may occur when the dose reaches to 40 Gy or more.3 Vulva cancer patients are more likely to have skin reaction or radiodermatitis because of its intertriginous location and the skin of vulva has an apparently poor tolerance to irradiation.4 At present, the worldwide studies on radiodermatitis are mainly focused on its assessment and management,5 and numerous studies intended to prevent acute radiodermatitis through creams, passive-scattering proton therapy or semipermeable dressing, but their efficacy have not been consistently proven.2, 6, 7 Furthermore, few studies analyzed the risk factors of radiodermatitis, and the sample size of existing studies was limited.
Based on this, this retrospective study aims to explore the risk factors of radiodermatitis in vulvar cancer patients, so as to provide theoretical basis for early identification of high-risk patients with radiodermatitis and the adoption of specific intervention measures.
2 MATERIALS AND METHODS
2.1 Enrollment of patients
This study included patients with vulvar carcinoma who received radiation therapy in the Jiangsu Cancer Hospital and Affiliated Hospital of Xuzhou Medical University from January 2015 to December 2020. The enrolled patients did not receive surgical treatment before radiation therapy and the diagnosis of radiation lesions was based on the grading criteria of the American Center for Radiological Oncology. This retrospective study was approved by the local Medical Ethics Committee, and it met the ethical standards.
2.2 Grading criteria for radiodermatitis
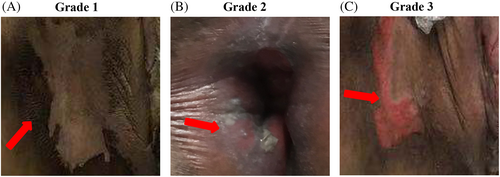
The grading of radiodermatitis was evaluated according to the grading standard of Radiation Therapy Oncology Group (RTOG): grade 0: no change; grade 1: dark red spots with follicular appearance/dry desquamation/hair loss/reduced sweating; grade 2: tender or bright red spots, flaky erosion/moderate edema; grade 3: erosions and pitting edema in areas other than skin wrinkles; grade 4: ulcer, bleeding, and necrosis.
In our study, we divided the patients into two groups, grade 0–1 and grade 2–4 based on whether radiodermatitis required treatment, because grade 1 radiodermatitis, which is characterized by pigmentation of the skin, is a common skin change that occurs with increased radiation dose and does not require treatment. However, when grade 2 radiodermatitis occurs, the skin can develop from mild erythema to moist desquamation, which affect patients' quality of life and may cause the cessation of radiotherapy.
2.3 Data collection
The following clinical information of enrolled patients were collected from the electronic medical records system, including: (1) basic clinical characteristics (sex, age, height, weight, marital status, reproductive history); (2) diseases (pathological stage, past medical history); (3) treatment (therapeutic strategy, radiotherapy dose); (4) long-term follow-up data of patients with radiodermatitis (treatment plan, treatment frequency and curative effect).
2.4 Statistical analysis
SPSS 20.0 was used for all data analyses. The univariate analysis was used to analyze the relationship between baseline clinical features and radiodermatitis, and the multivariate logistic regression analysis was used to determine independent risk factors for radiodermatitis. p < .05 was considered significant.
3 RESULTS
3.1 Baseline clinical information
A total of 60 patients were included in this study, and their clinical information were shown in Table 1. All patients were married, and their median age was 65.5 years old (range 30 ~ 91 years old). Among these patients, 21 (35%) were pathological stage I, 19 (31.7%) were pathological stage II, and 20 (33.3%) were pathological stage III. The 26 patients were treated with radiotherapy alone, while 34 patients were treated with concurrent chemoradiotherapy. There were 3, 25, 28, and 4 patients suffered from grade 0, 1, 2, and 3 radiodermatitis, respectively, and no patients developed grade 4 radiodermatitis. As shown in Figure 1, grade 1 radiodermatitis showed dark red spots and dry desquamation, grade 2 radiodermatitis presented with tenderness, bright red spots, flaky erosion or moderate edema, grade 3 radiodermatitis showed erosions and pitting edema in areas other than skin wrinkles.
| Characteristic | Value |
|---|---|
| Age, years | |
| Median (range) | 65.5 (30–91) |
| BMI | |
| <18.5 | 6 (10%) |
| 18.5–23.9 | 22 (36.7%) |
| ≥23.9 | 32 (53.3) |
| Education | |
| Illiterate | 31 (51.7%) |
| Junior high school and below | 24 (40%) |
| Senior secondary school and above | 5 (8.3%) |
| Number of children | |
| ≤1 | 16 (26.7%) |
| 2 | 12 (20%) |
| ≥3 | 32 (53.3%) |
| Pathological stage | |
| I | 21 (35%) |
| II | 19 (31.7%) |
| III | 20 (33.3%) |
| Treatment plan | |
| Radiotherapy alone | 26 (43.3%) |
| Concurrent chemoradiation | 34 (56.7%) |
| Radiotherapy dose | |
| ≤45 Gy | 30 (50%) |
| >45 Gy | 30 (50%) |
| Combined chronic disease | |
| Yes | 15 (25%) |
| No | 45 (75%) |
| Grading of radiation dermatitis | |
| 0 | 3 (5%) |
| 1 | 25 (41.7%) |
| 2 | 28 (46.7%) |
| 3 | 4 (6.6%) |
3.2 Analysis of risk factors for radiodermatitis
3.2.1 Single factor correlation analysis
The results of univariate analysis (Table 2) indicated that there were statistically significant differences in age (p = .044), pathological stage (p = .039), therapeutic strategy (p = .001), and radiotherapy dose (p = .031) between grade 0–1 and grade 2–4 groups.
| Variable | No. | Grade 0–1/case (%) | Grade 2–4/case (%) | p |
|---|---|---|---|---|
| Age | .044a | |||
| ≤60 years | 21 | 14 (66.7) | 7 (33.3) | |
| >60 years | 39 | 14 (35.9) | 25 (64.1) | |
| BMI | .432 | |||
| <18.5 | 6 | 1 (16.7) | 5 (83.3) | |
| 18.5–23.9 | 22 | 14 (63.6) | 8 (36.4) | |
| ≥23.9 | 32 | 13 (40.6) | 19 (59.4) | |
| Education | .379 | |||
| Illiterate | 31 | 10 (32.3) | 21 (67.7) | |
| Junior high school and below | 24 | 15 (62.5) | 9 (37.5) | |
| Senior secondary school and above | 5 | 3 (60.0) | 2 (40.0) | |
| Number of children | .622 | |||
| ≤1 | 16 | 8 (50.0) | 8 (50.0) | |
| 2 | 12 | 6 (50.0) | 6 (50.0) | |
| ≥3 | 32 | 14 (43.8) | 18 (56.2) | |
| Pathological stage | .039a | |||
| I | 21 | 14 (66.7) | 7 (33.3) | |
| II | 19 | 9 (47.4) | 10 (52.6) | |
| III | 20 | 5 (25.0) | 15 (75.0) | |
| Treatment plan | .001a | |||
| Radiotherapy alone | 26 | 18 (69.2) | 8 (30.8) | |
| Concurrent chemoradiation | 34 | 10 (29.4) | 24 (70.6) | |
| Radiotherapy dose | .031a | |||
| ≤45 Gy | 30 | 18 (60.0) | 12 (40.0) | |
| >45 Gy | 30 | 10 (33.3) | 20 (66.7) | |
| Combined chronic disease | .671 | |||
| Y | 15 | 5 (33.3) | 10 (66.7) | |
| N | 45 | 23 (51.1) | 22 (48.9) |
- Note: Only risk factors in Table 2 with p value less than .05 were considered for inclusion in a multivariable analysis.
- a Statistically significant, p < .05.
3.2.2 Multivariate logistic regression analysis
Then the variables significantly related to radiodermatitis were introduced into logistic regression equation for multivariate logistic regression analysis. The results showed that age (odds ratio [OR], 3.270; 95% confidence interval [CI], 1.024–10.446; p = .046), therapeutic strategy (OR, 4.894; 95% CI, 1.775–13.492; p = .002) and radiotherapy dose (OR, 3.273; 95% CI, 1.163–9.012; p = 0.025) were independent risk factors for the occurrence of grade 2–4 radiodermatitis (Table 3).
| Items | Odds ratio | 95% confidence interval | p |
|---|---|---|---|
| Age | 3.270 | 1.024–10.446 | .046a |
| Pathological stage | 0.607 | 1.187–2.667 | .607 |
| Treatment plan | 4.894 | 1.775–13.492 | .002a |
| Radiotherapy dose | 3.273 | 1.163–9.012 | .025a |
- a Statistically significant, p < .05.
4 DISCUSSION
Radiodermatitis, an inflammatory skin disease, is one of the most common complications of radiotherapy in patients with breast cancer, head and neck cancer, as well as vulvar carcinoma.8, 9 Vulvar carcinoma is a malignant tumor of the female perineum, accounting for about 3% ~ 5% of female malignant tumors. It mainly occurs in postmenopausal women and tends to increase with age. The incidence of vulvar carcinoma has been reported to be increasing in recent decades, while the relative 2-year and 5-year survival rates have been decreasing.10 In the past, surgical resection was the main treatment for vulvar carcinoma. However, as most vulvar cancer patients are older and have a poor overall condition, their tolerance to radical resection is low and there are many postoperative complications. Besides, as patients with advanced vulvar cancer have a large tumor burden and a wide range of invasion, radical surgery requires the removal of pelvic organs, which inevitably result in the poor postoperative quality of life. Therefore, radiotherapy for vulvar carcinoma has gradually received more and more attention, and has become an important treatment strategy for vulvar cancers.10, 11
Radiation damage to the skin and mucous membranes occur within a few weeks after the initiation of radiotherapy.3, 12 Previous studies have shown that more than 90% patients developed erythema after standard radiotherapy, and about 10% patients developed erythema of grade 3 or 4.13 A number of previous studies have suggested that the risk of radiodermatitis is highly variable, and the probability and degree of injury mainly depend on the target of radiation, exposure dose, therapeutic factors and individual differences, among which high-dose irradiation is one of the most important predictors of the severity of acute radiodermatitis.14, 15 In this study, we found that the incidence rate of radiodermatitis was higher in the population receiving concurrent chemoradiotherapy, and the radiodermatitis was radiation dose-dependent, with the increase of radiation dose and the extension of radiation duration, the incidence of radiodermatitis increased, which was consistent with many other studies.14-17 However, the mechanism by which these factors cause radiodermatitis remains unclear, and we speculate that this might be related to the radio sensitization effect of concurrent chemotherapy, in other words, chemotherapy not only improves the antitumor effect of radiotherapy, but also increases the incidence of radiation-related adverse events.
In our study, age and pathological stage were also important predictors of the occurrence of radiodermatitis, while BMI, level of education, whether combined other chronic diseases or not and childbearing history had no significant correlation with the appearance of radiodermatitis. However, J. R. Kouvaris et al. found that BMI was a risk factor for radiodermatitis,4 which was not consistent with our findings, and this may be due to different radiotherapy techniques, small sample size and racial differences.
From this, we suggest clinicians to identify high-risk patients early and take timely intervention measures according to the high-risk factors associated with radiodermatitis identified in this study, so as to effectively prevent the occurrence and inhibit the progression of radiodermatitis. For instance, for elderly patients, the dose of single radiotherapy can be appropriately reduced; if the effect of radiotherapy alone is better, concurrent chemoradiotherapy should be avoided as far as possible; for patients with high-risk factors of radiodermatitis, preventive measures should be taken ahead of time, although there are no universally recommended measures to prevent radiodermatitis, it is necessary to use dressings or creams on the surface of the skin for high-risk patients.
Moreover, this study has some limitations. First, the sample size of patients included in this study is relatively small, although we enrolled patients in two hospitals. Second, because it's a retrospective study, the nursing intervention methods may vary in the two hospitals. Therefore, we will continue to collect vulvar carcinoma patients to expand the sample size, and we will develop standard care measures to reduce deviations when conducting the study in collaboration with different hospitals.
In conclusion, the results of this retrospective study suggested that age, therapeutic strategy, pathological stage and radiotherapy dose were closely related to radiodermatitis in patients with vulvar tumor.
ACKNOWLEDGMENT
We would like to thank all the caregivers in the radiotherapy department for their assistance in collecting the data for this study.
FUNDING INFORMATION
This study was supported by Grants 71804073 from the National Natural Science Foundation of China.
CONFLICT OF INTEREST
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
ETHICS STATEMENT
The investigation was approved by the local Ethics Committee of Nanjing Medical University and the project No is (2018)550. All participants in the study patients have provided written informed consent.




