Clinical analysis of immediate breast reconstruction using latissimus dorsi muscular flap in breast cancer
Funding information: Basic Research Program of Jiangsu Province (Natural Science Foundation, Grant/Award Number: BK20191078; Internal Medicine Research Project of Jiangsu Cancer Hospital, Grant/Award Number: ZM202016
Abstract
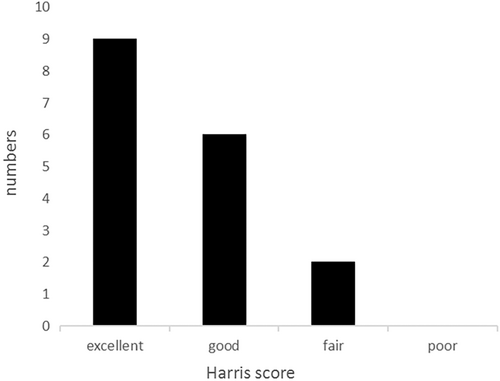
The aim of this study is to explore the clinical efficacy of immediate breast reconstruction (IBR) using the latissimus dorsi muscular flap in Chinese breast cancer patients. The clinical data of 17 breast cancer patients who underwent IBR using the latissimus dorsi muscular flap between August 2013 and September 2021 at Affiliated Cancer Hospital of Nanjing Medical University were analyzed retrospectively. Harris scoring standard was used to evaluate the cosmetic effect. All the 17 cases were successfully treated. The median age was 43 years old (age range: 32–54 years old). In the clinical staging, the patients were mainly early and mid-stage patients, with two cases in stage 0, 12 cases in stage II, and three cases in stage III. Postoperative pathology was predominantly invasive breast cancer (15/17), and two cases were carcinoma in situ. The median operation time was 300 min (range: 180–450 min) and only two patients developed complications. After 2–97 months of follow-up, no patients had recurrence or metastasis. According to the Harris method, 9, 6, 2, and 0 cases were evaluated as “excellent”, “good”, “fair,” and “poor” respectively. The practical application of IBR using the latissimus dorsi muscular flap is a safe and feasible way to improve physical and mental health in breast cancer patients.
1 INTRODUTION
Breast cancer (BC) is one of the most common malignant tumors and its incidence is increasing.1 Surgical therapy remains a mainstay of treatment for breast cancer patients, especially in early-stage cancer. Modified radical mastectomy remained the primary strategy for treating breast cancer, however, changes in body shape and impaired posture result in depression and anxiety in these patients after mastectomy. Breast-conserving surgery seems to be a good choice for breast cancer patients, unfortunately, the limitation of tumor sizes and the risk of tumor recurrence are the major obstacles to breast cancer patients.2 Breast reconstruction, including implant-based reconstruction and autologous breast reconstruction, brings new options for these patients.
In 1977, Schneider opened the prelude to breast reconstruction with autologous tissues, and for the first time reported the use of latissimus dorsi for breast reconstruction.3 Since then, the use of latissimus dorsi for breast reconstruction has been an acceptable and valid choice. However, the concerning complications and high level of technical difficulty were the major obstacles to this new surgical technique. Therefore, we conducted a retrospective research to explore the clinical effect of immediate breast reconstruction (IBR) using the latissimus dorsi muscular flap (LDMF) in the Chinese population.
2 MATERIALS & METHODS
2.1 Specimens collection
A retrospective study was carried out between August 1, 2013 and September 30, 2021 at Affiliated Cancer Hospital of Nanjing Medical University, a total of 17 patients were identified finally from the breast cancer patients who received IBR. Since IBR with autologous tissue was one of the most difficult reconstructions, we had set strict standards for inclusion: (1) Patients with small and medium breasts, who expected that the reconstructed breast is natural, beautiful, and soft were suitable; (2) The latissimus dorsi muscle was intact, the blood supply was good and the skin of breast was not invaded; (3) It was not suitable or not accepted for breast-conserving surgery, implant-based and rectus abdominis myocutaneous flap reconstruction. At the same time we had established strict exclusion criteria: (1) Inflammatory and metastatic breast cancer were the absolute contraindications. (2) Patients who had systemic diseases, such as cardiovascular, respiratory system, immune diseases, and history of deep vein thrombosis and long-term smoking were excluded. (3) Delayed and combined breast reconstruction patients were not selected in this study. The study was authorized by the Ethics Committee of Jiangsu Cancer Hospital and all patients signed the written informed consent.
2.2 Surgical techniques
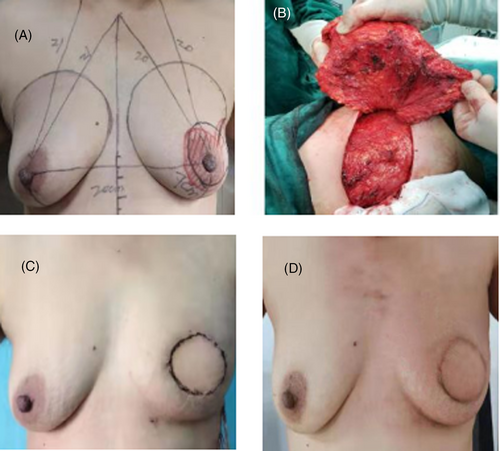
The operation method was briefly described. Before the operation, we assessed fully the condition of the breast and back by ultrasound and magnetic resonance to guide the preoperative design. Subsequently, we marked the separation range of the breast and the cut range of the latissimus dorsi myocutaneous flap (Figure 1A). After successful general anesthesia, we first separated the breast on the surface of the pectoralis major muscle, and performed sentinel lymph node biopsy or axillary lymph node dissection according to the patient's condition. We estimated the required muscle volume and dissected the muscle fat flap according to the shape and size of the reconstructed breast (Figure 1B). After cutting off the latissimus dorsi muscle bundle above the entry point of the thoracodorsal artery, through the subcutaneous tunnel, the latissimus dorsi musculocutaneous flap was transferred to the chest. Next, we adjusted the shape and size of the reconstructed breast by cutting the flaps and fixed the breast. Finally, we stopped the bleeding on the wound thoroughly, placed negative pressure drainage tube and sutured the skin. The color of the flap was monitored every day until the patient was discharged (Figure 1C). The postoperative patients underwent outpatient followed-up (Figure 1D).
2.3 Follow-up
After breast reconstruction, patients received chemotherapy, endocrine therapy and targeted therapy according to the corresponding breast cancer types. All patients were followed-up. Harris scoring standard, which has four grades: excellent, good, fair, and poor was used to evaluate the cosmetic effect.4
3 RESULTS
The baseline characteristics of these 17 patients were shown in Table 1. All the collected 17 patients with immediate latissimus dorsi breast reconstruction were women. The median age was 43 years old (age range: 32–54 years old), and the majority of them were younger than 50 years old (14/17). Most of the patients went to the doctor because of breast lumps, 13 of them were on the left breast, and four were on the right breast. In the clinical stage, the patients were mainly early and mid-stage patients, with two cases in stage 0, 12 cases in stage II, and three cases in stage III. Postoperative pathology was predominantly invasive breast cancer (15/17), two cases were carcinoma in situ, and half of the patients had lymph node metastasis (9/17). In the molecular classification, there were three cases of luminal A type, seven cases of luminal B type, and five cases of Her-2 positive.
| Clinical parameters | Number of patients |
|---|---|
| Age | |
| ≤50 years old | 14 |
| >50 years old | 3 |
| Tumor site | |
| Left | 13 |
| Right | 4 |
| Clinical staging | |
| 0 | 2 |
| II | 12 |
| III | 3 |
| Histology WHO | |
| Invasive carcinoma | 15 |
| Carcinoma in situ | 2 |
| Lymph node metastasis | |
| Yes | 9 |
| No | 8 |
| Breast cancer types | |
| Luminal A | 3 |
| Luminal B | 7 |
| HER-2 positive | 5 |
| Operation time | |
| <300 min | 8 |
| ≥300 min | 9 |
| Complication | |
| Delayed healing | 1 |
| Seroma | 1 |
| None | 15 |
The median operation time was 300 min (range: 180–450 min), and half of the operation time was longer than 300 min (9/17). No patients experienced flap ischemia, infection or necrosis, and no patients experienced dysfunction of the affected limbs after the operation. There were only two patients who developed complications. One was seroma in the back incision, which healed after repeated puncture and pressure bandaging; the other was wound delayed healing, which healed nearly 1 month after multiple dressing changes.
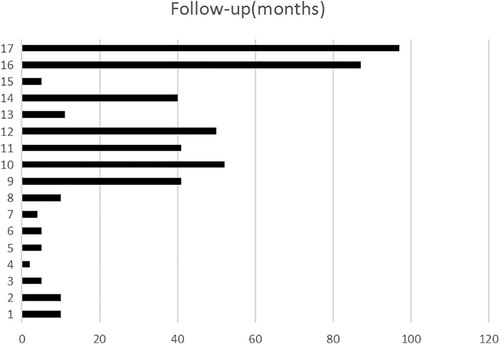
After 2–97 months of follow-up, no patients had recurrence or metastasis (Figure 2). According to the Harris method, 9, 6, 2, and 0 cases were evaluated as “excellent,” “good,” “fair,” and “poor,” respectively (Figure 3). The survey on breast surgery satisfaction showed that most breast reconstruction patients were satisfied with breast reconstruction.
4 DISCUSSION
The breast is an important second sex organ for women and the source of women's self-confidence. The breast defect has a serious impact on the patient's physical and mental health and social relations.5With the development of plastic surgery technology, the in-depth understanding of breast cancer disease, and the significant improvement in patients' awareness of seeking beauty, the purpose of breast cancer treatment has also shifted from simply improving the survival rate to improving the quality of life. Therefore, the ideal model of breast cancer treatment should maintain the shape of the breast while eradicating the tumor. Although breast-conserving surgery can be our first choice, breast reconstruction has become an important alternative for breast cancer patients with tumors larger than 5 cm, multi-center lesions, and multiple positive margins that cannot be breast-conserved.6
The overall rate of breast reconstruction is 10.7% in surgical treatment for breast cancer in China, with 20.1% for autologous tissue reconstruction.2 The long period of personnel training in reconstruction surgery and the difficulty in acquiring flap and other materials are the important limitations when the new surgical techniques are adopted. Although the rate of breast reconstruction is low, the latissimus dorsi flap is still the most commonly used flap in autologous reconstruction performed at our hospital. It has the following advantages: it has constant vascular anatomy, rich blood supply, and flexible flap removal. It is relatively easy to operate and does not need to cooperate with microsurgical techniques such as vascular anastomosis. Whether it is delayed breast reconstruction or IBR, it can be performed with latissimus dorsi myocutaneous flap. It can be used alone or combined with silicone breast implant in breast reconstruction at the same time.7
The seroma of the back donor site is the most common complication after IBR with latissimus dorsi musculocutaneous flap, whose rate is as high as 12% ~ 50%.8 In our study, only one patient developed a seroma due to a small sample size. In order to reduce the occurrence of seroma, separation between the shallow and deep fat gaps, careful hemostasis, the placement and the maintenance of negative pressure drainage tube at the lowest point are the key to prevent during the operation. Restricting the movement of the affected upper limbs, and the fixation of the back flaps can effectively reduce the incidence of seroma after the operation, also.9
Latissimus dorsi can reshape the shape of the breast, and patient satisfaction is high. In our research, we found that the most patients were satisfied with breast reconstruction, which had greatly improved the quality of life in patients. Metastasis and recurrence of breast cancer are related to tumor size, stage, lymph node status and degree of differentiation.10 Recent studies have shown that IBR is a safe and effective treatment, which will not increase tumor local recurrence and distant metastasis.11 From our current small-scale study, it is found that the application of latissimus dorsi myocutaneous flap for breast reconstruction is safe, and no patients with local recurrence and distant metastasis have been found.
In the present day, the economy and reconstructive learning curve were the primary factors limiting the increased application of LDMF. Although breast reconstruction using LDMF has been recorded in several articles, limited information could be adopted in IBR using LDMF without implants in the Chinese population. Undoubtedly, the absolute number of IBR using LDMF without implants was still quite low, so this research was designed to review a series of 17 breast cancer patients who underwent IBR using LDMF without implants in the nearly 8 years. Moreover, there were only a few investigations about the possible risks, complications and satisfaction in IBR using LDMF without implants. Thus, the clinical application feasibility and the cosmetic effect in breast reconstructive patients were retrospectively collected and evaluated in our study.
We should consider the potential limitations on our study. First, this retrospective research is a single-center study and the number of samples enrolled is small, which can result in an inherent bias. Second, this study is a single-arm trial and lacks a control group, which may lead to a possibility of selection bias. Therefore, a large-scale randomized controlled study should be considered in further studies.
5 CONCLUSIONS
In conclusion, the use of IBR with LDMF is a safe and effective way to improve physical and mental health in breast cancer patients. The long period of personnel training is the key to improve the rate of breast reconstruction. A large-scale randomized controlled study should be conducted in further studies.
ACKNOWLEDGMENTS
This work was supported by the Internal Medicine Research Project of Jiangsu Cancer Hospital (ZM202016) and Basic Research Program of Jiangsu Province (Natural Science Foundation, No. BK20191078).
CONFLICT OF INTEREST
The authors declare there is no potential conflicts of interest.




