Childhood BMI trajectories predict cardiometabolic risk and perceived stress at age 13 years: the STARS cohort
Abstract
Objective
The aim of this study was to examine BMI trajectories from birth throughout childhood, associations with health outcomes at age 13 years, and time frames during which early-life BMI influenced adolescent health.
Methods
Participants (1902, 44% male) reported perceived stress and psychosomatic symptoms and were examined for waist circumference (WC), systolic blood pressure (SBP), pulse wave velocity, and white blood cell counts (WBC). BMI trajectory was analyzed using group-based trajectory modeling of retrospective data of weight/height from birth throughout childhood. The authors performed linear regression to assess associations between BMI trajectories and health outcomes at age 13 years, presented as estimated mean differences with 95% CI among trajectories.
Results
Three BMI trajectories were identified: normal; moderate; and excessive gain. Adjusting for covariates, adolescents with excessive gain had higher WC (19.2 [95% CI: 18.4–20.0] cm), SBP (3.6 [95% CI: 2.4–4.4] mm Hg), WBC (0.7 [95% CI: 0.4–0.9] × 109/L), and stress (1.1 [95% CI: 0.2–1.9]) than adolescents with normal gain. Higher WC (6.4 [95% CI: 5.8–6.9] cm), SBP (1.8 [95% CI: 1.0–2.5] mm Hg), and stress (0.7 [95% CI: 0.1–1.2]) were found in adolescents with moderate versus normal gain. The association of early-life BMI with SBP started around age 6 years with the excessive gain group, which was earlier than in the normal and moderate gain groups, in which it started at age 12 years.
Conclusions
An excessive gain BMI trajectory from birth predicts cardiometabolic risk and stress in 13-year-old individuals.
Study Importance
What is already known?
- Childhood obesity has a significant impact on the development of type 2 diabetes, hypertension, and cardiovascular disease in adulthood.
What does this study add?
- Moderate and excessive BMI gain trajectories from birth were associated with higher waist circumference, systolic blood pressure (SBP), white blood cell counts, and perceived stress in healthy 13-year-old individuals.
- In the excessive gain group, the influence of early-life BMI on SBP started around age 6 years.
How might these results change the direction of research or the focus of clinical practice?
- Our findings stress the importance for researchers and policy makers to look beyond BMI, considering broader health risks from an early age and encompassing both mental and physical well-being.
INTRODUCTION
Children with obesity are approximately five times more likely to experience obesity in adulthood compared with those without obesity [(1)]. The alarming rise in childhood obesity is especially concerning due to its significant impact on the development of type 2 diabetes, hypertension, and cardiovascular disease in adulthood [(2, 3)]. Furthermore, there is increasing evidence supporting the notion that early or rapid childhood weight gain already leads to health problems in adolescence. Early age at body mass index (BMI) rebound has been associated with greater adiposity, insulin resistance, and metabolic risk score in adolescence [(4)]. In children and adolescents, overweight is associated with higher C-reactive protein concentration and higher white blood cell counts (WBC), suggesting a state of low-grade systemic inflammation [(5)].
Instead of using BMI measure at one point in time, recent research has increasingly utilized group-based trajectory modeling approaches, i.e., person-centered techniques, to study childhood BMI trajectories, capture the dynamic changes in BMI over time, and identify diverse patterns [(6)]. Considering blood pressure and pulse wave velocity (PWV) variations in adolescence as predictors of adult cardiovascular disease and mortality [(7)], numerous studies have examined the associations between childhood BMI trajectories and blood pressure [(8-11)] as well as PWV [(9, 10, 12-14)]. However, the findings from these studies have yielded mixed results. Whereas some studies have shown that higher childhood BMI trajectory is associated with higher systolic blood pressure (SBP) [(8, 10, 11)] and PWV [(12-14)], others have found similar levels of SBP [(9)] and PWV [(9, 10)] across different BMI trajectories. Previous studies have shown that adolescents with accelerated BMI trajectory had increased central adiposity [(10)]. No studies, to our knowledge, have assessed whether childhood BMI trajectories are associated with WBC.
Similar to obesity, mental health problems are increasingly prevalent and disabling among children and adolescents [(15)]. In Sweden, the proportion of 13- and 15-year-old students reporting multiple psychosomatic symptoms continue to increase, reaching the highest levels in the survey year 2021 to 2022 since the mid-1980s [(16)]. These subjective health complaints have been shown to reflect stress among adolescents [(17)]. There is evidence supporting the association between chronic stress and overweight/obesity in adolescents [(18)]. Meanwhile, cross-sectional studies often report that children with excess weight are more likely to be stigmatized and experience the burden of psychiatric and psychological disorders in childhood and adolescence [(19)]. There are scarce data regarding the influence of childhood BMI trajectories on mental health problems. Having high BMI growth trajectory during childhood has been shown to be linked to worse scores for emotional symptoms, peer problems, happiness, body satisfaction, and self-esteem at age 11 years [(20, 21)]. No studies, to our knowledge, have examined whether early-life BMI trajectory may be linked to perceived stress and psychosomatic symptoms in adolescents.
Most studies using group-based trajectory modeling approaches have focused mainly on childhood and adolescence, missing birth and infancy [(6)]. It is well known that the first 2 years of a child's life are a sensitive window for the development of obesity and cardiometabolic disease in adulthood [(22)]. Moreover, studies employing group-based trajectory modeling often face limitations in terms of the number of measurement occasions, which can negatively impact the precision and accuracy of the identified trajectories [(23)].
Furthermore, there is limited knowledge regarding whether distinct growth trajectories may have varying time frames in which early-life BMI influences adolescent health outcomes. This has potential significance because it raises the possibility that BMI at certain ages and/or specific patterns over time may be particularly influential in determining cardiometabolic risks and mental well-being during adolescence.
The STudy of Adolescence Resilience and Stress (STARS) provides an excellent opportunity to examine when and how childhood growth trajectories may impact adolescent health. The data set from STARS provided 11 measurements of weight and length/height data collected from birth to age 13 years. It offered a comprehensive examination of various aspects of physical health, including vascular functions (blood pressure, PWV), central obesity (waist circumference [WC]), and inflammation markers (WBC) at age 13 years. Additionally, mental health indicators such as perceived stress and psychosomatic symptoms were also assessed at age 13 years, at the same time as the physical examination.
The aims of this study were three-fold: 1) to identify overall BMI trajectories from birth to age 13 years; 2) to determine whether BMI trajectories predict adverse health outcomes (health risk) at age 13 years, and, if so; 3) to study whether differences exist among trajectories regarding time frames during which early-life BMI influenced health outcomes.
METHODS
Study participants
Seventh-grade pupils were recruited for STARS, an ongoing longitudinal cohort with baseline examinations and three follow-ups (2-year, 5-year ongoing, and 10-year). The recruitment of participants took place in 54 schools across 16 municipalities in Western Sweden, as previously described [(17)]. Schools were purposefully selected from different areas with various socioeconomic contexts. For this study, we utilized baseline data and retrospectively collected data from other data bases.
Both pupils and their parents or guardians provided written informed consent for participation and use of data in the research. The study received approval from the Swedish Ethical Review Authority (Dnr 578–15).
Childhood growth measurements
We retrospectively collected weight and length/height data from birth to age 12 years. Data from birth and around age 6, 12, and 18 months and age 2, 4, and 5 years were retrospectively collected from the child health care data base. Data around ages 8 (grade 2), 10 (grade 4), and 12 years (grade 6) were retrospectively collected from the school health care data base. Weight and height at age 13 years (grade 7) were measured during the baseline examination in STARS.
In order to be included in the analysis, individuals needed to have attended the baseline examination at age 13 years and have a minimum of five weight and length/height measurements: one at birth; at least one measurement between ages 6 and 18 months (maximum 3 measures); at least two measurements between ages 2 and 8 years (maximum 4 measures); and at least one measurement between ages 10 and 13 years (maximum three measures). This allowed for the coverage of birth, infancy, the typical period of adiposity rebound, and late childhood to early adolescence. A total of 1902 participants (829 male) were included in the BMI trajectory analysis.
Health outcomes at age 13 years
Weight, height, and WC were measured using standard anthropometric equipment. Participants were measured while wearing light clothing and without shoes. Age- and sex-specific BMI z scores were then calculated [(24)].
Resting blood pressure and heart rate were measured after a minimum of 5 min of rest and repeated at least three times using GE Dinamap Carescape version 100 device (Sweden). Additional measurements were taken if there was a variation exceeding 5%. Carotid-femoral PWV was measured at least three times using the oscillometer Vicorder (SMT medical GmbH & Co, Düsseldorf, Germany). Additional measures were taken if the readings differed by more than 0.5 m/s. The mean of the three measurements was used for the analyses. Non-fasting blood samples were collected, and WBC were analyzed using HemoCue WBC DIFF system (HemoCue AB, Ängelholm, Sweden).
We assessed perceived stress using the 10-item Perceived Stress Scale, which measures the extent to which respondents perceive their lives as unpredictable, uncontrollable, and overwhelming [(25)]. The Psychosomatic Problem Scale was used to measures the frequency of perceived psychosomatic symptoms such as difficulties in concentrating and sleeping [(26)]. More details can be found in online Supporting Information.
Covariates
To assess potential covariates, we included sex at birth, age at health examinations, migrant background, and family socioeconomic status (SES). Family SES was measured using parental earned income from the year preceding the health examinations at age 13 years. The income information was collected from the Income and Taxation Register at Statistics Sweden. In our analyses, we categorized parental earned income into quintiles.
Statistical analyses
First, we performed a nonresponse analysis by comparing characteristics of adolescents who were included and excluded in the current study. This analysis involved the use of Student t tests and χ2 tests to assess any significant differences between the two groups.
Second, we applied group-based trajectory modeling (PROC TRAJ, SAS version 9.4, Cary, North Carolina) to identify BMI trajectories. The longitudinal BMI data were fitted using a polynomial function of age with the maximum likelihood method. In line with the recommendations of Cole et al. [(27)], we employed BMI instead of BMI z scores. More details can be found in online Supporting Information and Table S1.
After selecting the best-fitting model, individuals were assigned to one of the trajectory classes based on their highest estimated group membership probabilities. Posterior probability of each trajectory is presented in Table S2.
In an exploratory analysis, we examined the trajectories separately for male and female individuals to assess whether they followed similar patterns. We identified three trajectories in both sexes that exhibited similar developmental patterns (data not shown). As a result, the BMI trajectories of the entire analysis sample were utilized in the subsequent steps.
Third, we used linear regression analysis to investigate the impact of BMI trajectories (trajectory membership as predictor) on health outcomes and reported point estimates of unstandardized linear slope coefficients (b) and 95% confidence intervals (CI). Furthermore, we constructed a combined health risk load using all six health outcomes, namely blood pressure, WC, WBC, PWV, stress, and psychosomatic symptoms at age 13 years, calculated as the sum of the number of high-risk health outcomes (range 0–6). High blood pressure was defined as elevated blood pressure and hypertension according to the 2017 guideline [(28)]. For other health outcomes, high-risk level was defined as ≥90th percentile of the STARS cohort data (details in online Supporting Information). The association between the BMI trajectories and the cumulative health risk load (classified as 0, 1, or ≥2) was analyzed using ordinal logistic regression. The predicted probability was derived from the proportional odd ratios estimated for the sex-, age-, migrant background-, and parental income-adjusted ordinal logistic model. Differences in the predicted probability among the BMI trajectory groups were tested by ANOVA, and a Bonferroni-corrected p ≤ 0.05 was considered statistically significant.
Finally, we examined whether differences exist among trajectories regarding time frames during which early-life BMI influences health outcomes at age 13 years. We analyzed associations of BMI measured at different time points with sex- and age-adjusted health outcomes.
All analyses, except identifying BMI trajectories, were carried out using SPSS Statistics version 27 (IBM Corp., Armonk, New York). A two-sided p ≤ 0.05 was considered statistically significant.
RESULTS
Nonresponse analysis showed that, compared with included participants, the excluded participants were more likely to have a migrant background, mostly due to the lack of growth data during infancy. More details about nonrespondents, as well as detailed information about the number of BMI measurements, can be found in online Supporting Information and Tables S3–S7.
Childhood BMI trajectories
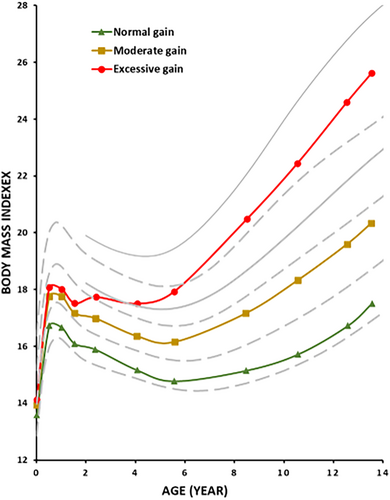
Three distinct BMI trajectories were identified, and they were plotted on gender-weighted averages of Swedish BMI reference (median, +1 SD, and +2 SD) [(29)] and International Obesity Task Force cutoffs for overweight and obesity ((1, 24)].
Two trajectories closely followed the Swedish growth reference chart: one slightly under the median line (44.5% of the sample, named normal gain); and another above the median line (42.8%, named moderate gain). Participants in the moderate gain group had statistically significant, although modestly, higher birth weight (3.56 ± 0.51 kg) than those in the normal gain group (3.45 ± 0.51 kg). BMI in the moderate gain group increased more during the first 6 months after birth and after age 5 years when compared with those in the normal gain group. The third trajectory crossed the +1 SD and +2 SD lines of the Swedish growth chart around ages 2 and 6 years, respectively; therefore, it exhibited excessive weight gain during both infancy and early childhood (12.6%, named excessive gain). The birth weight of individuals in the excessive gain group (3.62 ± 0.59 kg) was statistically significantly higher than those in the normal gain group, but it did not differ from the moderate gain group. Starting from 18 months after birth, significant differences were observed between the moderate gain and excessive gain groups, and these differences continued to widen with age. Therefore, individuals in the excessive gain group had cumulative exposure to higher BMI levels already from infancy and onward.
Visual inspection of the BMI trajectories revealed that the adiposity rebound, a period of increased adiposity after a decline in early childhood, occurred around age 6 years for the normal gain and moderate gain trajectories. However, for the excessive gain trajectory, the adiposity rebound was observed much earlier, i.e., around ages 2 to 3 years (Figure 1).
Birth length and gestational age did not differ among the three trajectories (data not shown). There was no pattern or relationship between the number of BMI data a child had and the BMI trajectory class they were assigned to (Table S6). The mean number of BMI measures available did not differ among the three BMI trajectories.
Associations of childhood BMI trajectories with health outcomes at age 13 years
Demographic characteristics and health outcome measures of participants are presented in Table 1. The distribution of sex was similar across the three BMI trajectories. The excessive gain group had a higher portion of individuals with a migrant background and lower parental earned income than the normal gain group. Statistically significant differences were found for BMI z score, WC, SBP, WBC, perceived stress, and psychosomatic symptoms, but not in diastolic blood pressure and PWV.
| Overall | Normal gain | Moderate gain | Excessive gain | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | 95% CI | N | Mean | 95% CI | N | Mean | 95% CI | N | Mean | 95% CI | |
| Age (y) | 1902 | 13.5 | (12.0–15.1) | 847 | 13.6 | (12.7–15.1) | 815 | 13.5 | (12.3–14.5) | 240 | 13.5 | (12.0–14.6) |
| BMI (kg/m2) | 1897 | 19.7 | 19.6–19.9 | 846 | 17.5 | 17.4–17.6 | 813 | 20.3 | 20.2–20.4 | 239 | 25.6 | 25.3–26.0 |
| BMI z score | 1897 | 0.262 | 0.219–0.305 | 846 | −0.504 | −0.547 to −0.461 | 813 | 0.596 | 0.563–0.629 | 239 | 1.839 | 1.783–1.895 |
| WC (cm) | 1897 | 72.3 | 72.0–72.7 | 844 | 67.1 | 66.8–67.4 | 813 | 73.5 | 73.1–73.9 | 240 | 86.7 | 85.6–87.8 |
| SBP (mm Hg) | 1893 | 112 | 111–112 | 843 | 110 | 110–111 | 812 | 112 | 112–113 | 239 | 114 | 113–116 |
| DBP (mm Hg) | 1893 | 64 | 64–65 | 843 | 64 | 64–65 | 812 | 64 | 64–65 | 239 | 64 | 63–64 |
| PWV (m/s) | 1879 | 5.8 | 5.8–5.9 | 837 | 5.8 | 5.8–5.9 | 808 | 5.8 | 5.8–5.9 | 235 | 5.9 | 5.8–6.0 |
| WBC (109/L) | 1792 | 5.4 | 5.4–5.5 | 793 | 5.3 | 5.2–5.4 | 774 | 5.4 | 5.3–5.5 | 226 | 6.0 | 5.8–6.2 |
| Stress | 1895 | 15.4 | 15.2–15.7 | 846 | 15.0 | 14.6–15.4 | 811 | 15.6 | 15.2–16.0 | 239 | 16.4 | 15.6–17.2 |
| PSP | 1896 | 11.7 | 11.4–11.9 | 846 | 11.3 | 10.9–11.7 | 811 | 11.9 | 11.5–12.3 | 240 | 12.2 | 11.5–13.0 |
| N | % | N | % | N | % | N | % | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||||||
| Male | 829 | 43.6 | 364 | 43.0 | 361 | 44.3 | 104 | 43.3 | ||||
| Female | 1073 | 56.4 | 483 | 57.0 | 454 | 55.7 | 136 | 56.7 | ||||
| Migration background | ||||||||||||
| Migrant | 231 | 12.2 | 84 | 9.9 | 93 | 11.5 | 54 | 22.5 | ||||
| Swedish | 1664 | 87.8 | 761 | 90.1 | 717 | 88.5 | 186 | 77.5 | ||||
| Total parental earned income | ||||||||||||
| Quintile 1 | 318 | 17.2 | 111 | 13.5 | 132 | 16.6 | 75 | 32.3 | ||||
| Quintile 2 | 370 | 20.0 | 158 | 19.2 | 160 | 20.1 | 52 | 22.4 | ||||
| Quintile 3 | 391 | 21.1 | 171 | 20.8 | 173 | 21.8 | 47 | 20.3 | ||||
| Quintile 4 | 393 | 21.2 | 192 | 23.3 | 163 | 20.5 | 38 | 16.4 | ||||
| Quintile 5 | 378 | 20.4 | 191 | 23.2 | 167 | 21.0 | 20 | 8.6 | ||||
- Note: Data are presented as mean and 95% CI, except age, for which mean and minimum/maximum in brackets are presented.
- Abbreviations: DBP, diastolic blood pressure; PSP, psychosomatic symptom; PWV, pulse wave velocity; SBP, systolic blood pressure; WBC, white blood cell count; WC, waist circumference.
Table 2 presents the associations of childhood BMI trajectories with health outcomes at age 13 years. After controlling for sex, age, migrant background, and parental earned income, individuals in the excessive gain group exhibited a significantly larger WC (estimated mean difference 19.2 cm), higher SBP (3.6 mm Hg), increased WBC (0.7 × 109 cells per L), and higher stress scores (1.1) compared with adolescents in the normal gain group. However, there were no significant differences in PWV or psychosomatic symptoms between these two groups. Adolescents in the moderate gain group exhibited higher WC (6.4 cm), higher SBP (1.8 mm Hg), and a higher stress score (0.7) compared with those in the normal gain group.
| Unadjusted | Adjusteda | |||||
|---|---|---|---|---|---|---|
| b | 95% CI | Model R2 (%) | b | 95% CI | Model R2 (%) | |
| WC (cm) | ||||||
| Moderate gain | 6.4 | 5.8 to 7.0 | 54.6 | 6.4 | 5.8 to 6.9 | 59.0 |
| Excessive gain | 19.5 | 18.7 to 20.3 | 19.2 | 18.4 to 20.0 | ||
| SBP (mm Hg) | ||||||
| Moderate gain | 1.7 | 1.0 to 2.5 | 2.4 | 1.8 | 1.0 to 2.5 | 3.5 |
| Excessive gain | 3.5 | 2.4 to 4.6 | 3.6 | 2.4 to 4.7 | ||
| PWV (m/s) | ||||||
| Moderate gain | −0.0 | −0.1 to 0.0 | 0.2 | −0.0 | −0.1 to 0.0 | 3.8 |
| Excessive gain | 0.1 | −0.0 to 0.1 | 0.1 | −0.0 to 0.1 | ||
| WBC (109/L) | ||||||
| Moderate gain | 0.1 | −0.0 to 0.3 | 2.5 | 0.1 | −0.06 to 0.2 | 5.8 |
| Excessive gain | 0.7 | 0.5 to 1.0 | 0.7 | 0.4 to 0.9 | ||
| Stress | ||||||
| Moderate gain | 0.7 | 0.1 to 1.3 | 0.6 | 0.7 | 0.1 to 1.2 | 8.7 |
| Excessive gain | 1.4 | 0.5 to 2.3 | 1.1 | 0.2 to 1.9 | ||
| PSP | ||||||
| Moderate gain | 0.7 | 0.1 to 1.2 | 0.4 | 0.7 | 0.1 to 1.2 | 10.2 |
| Excessive gain | 0.9 | 0.1 to 1.7 | 0.6 | −0.2 to 1.4 | ||
- Note: Results are presented as unstandardized linear slope coefficient (b) with 95% CI. Bold values indicate a significant difference compared with the normal gain trajectory.
- Abbreviations: PWV, pulse wave velocity; PSP, psychosomatic symptoms; SBP, systolic blood pressure; WBC, white blood cell count; WC, waist circumference.
- a Adjusted for sex, age, migrant background, and parental income.
The variance explained by BMI trajectory was largest for WC (54.6%) and much smaller for SBP and WBC (~2.5%). For PWV, stress, and psychosomatic symptoms, only 0.2% to 0.6% of the variance was explained by BMI trajectory.
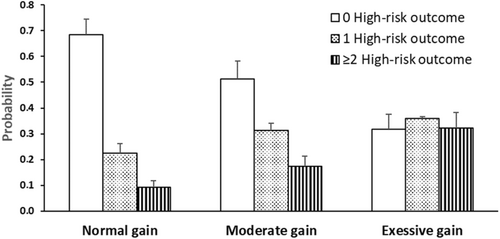
The numbers of adolescents having 0, 1, and ≥2 health risks were 977 (56.6%), 480 (27.8%), and 269 (15.6%), respectively. Ordinal logistic regression showed that the probability of having ≥2 risks increased two- to four-fold, from 0.09 in those with normal gain to 0.17 and 0.32 in those with moderate and excessive gain, respectively (Bonferroni-corrected p < 0.001; Figure 2).
Association (Spearman Rho) of early-life BMI values with health outcomes at age 13 years
After establishing the associations between BMI trajectories and health outcomes at age 13 years, our subsequent analysis aimed to explore potential variations among these trajectories concerning the time frames in which early-life BMI influences the observed health outcomes.
We found that a significant positive correlation of early-life BMI values with SBP started approximately at age 6 years for participants with excessive gain, i.e., much earlier than for participants with normal gain and moderate gain, for which it started at age 12 years (Figure 3A). We observed that, during infancy, there was a negative association between BMI and SBP at age 13 years. Notably, this negative association persisted for a longer duration in individuals with normal gain and moderate gain BMI trajectories (up to age ~5 years) compared with those with excessive gain.
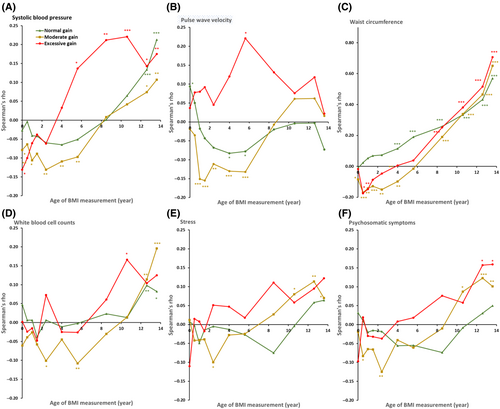
The patterns of how early-life BMI values were associated with PWV at age 13 years also differed across the three BMI trajectories (Figure 3B). For individuals with excessive gain, the associations were positive from birth to adolescence. However, for individuals with normal gain and moderate gain, the associations were negative during infancy and early childhood.
The associations of early-life BMI values with WC, WBC, stress, and psychosomatic symptoms at age 13 years were similar across the three BMI trajectories (Figure 3C–F).
DISCUSSION
In this retrospective longitudinal study involving 1902 participants, we identified, convincingly, associations between childhood BMI trajectories and health outcomes. Specifically, moderate and excessive gain trajectories were found to be associated with increased WC, SBP, and stress at age 13 years. In addition, the excessive gain trajectory was linked to increased WBC at age 13 years. Notably, individuals with excessive BMI gain during childhood exhibited SBP levels ~4-mm Hg higher than those with normal gain. Furthermore, the influence of early-life BMI on SBP in the excessive gain group began around age 6 years, which was much earlier than in the normal and moderate gain groups, in which it commenced at age 12 years. Although the last data point for BMI trajectory modeling overlapped with the health outcome measures, the differences distinguishing these trajectories were established before age 2 years, suggesting a temporal association between childhood BMI trajectories and health outcomes at age 13 years. Our findings underscore that high BMI gain during childhood is a potential burden for 13-year-old individuals because it is associated with a two- to four-fold increase in cumulative health risks at age 13 years.
Using group-based trajectory modeling, we identified three childhood BMI trajectories. The character and composition of these trajectories are consistent with two small studies that utilized more than 15 measures of growth data covering birth, infancy, the typical period of adiposity rebound, and late childhood to early adolescence [(9, 10)]. Three or four trajectories were the most common number of trajectories identified in previous studies [(6)].
One of the trajectories that we identified is the excessive gain with accelerated infant weight gain and maintenance of high adiposity. This trajectory was associated with ~4-mm Hg higher SBP than the normal gain trajectory. Interestingly, in the excessive gain group, a significant positive correlation of early-life BMI with SBP started at age ~6 years, which was much earlier than for the other two trajectories. In line with our findings, others have also identified similar excessive gain trajectories and found that, compared with those following an optimal adiposity trajectory, the excessive gain trajectories were associated with 4- to 8-mm Hg higher SBP at age 14 [(10)] or 17 years [(11)]. In addition, with repeated measures of blood pressure at different ages, Huang et al. showed that an increase in SBP in the excessive gain trajectories can be observed already at age 3 years [(11)]. It is interesting to note that, in a meta-analysis that examined the age-specific relevance of usual blood pressure to vascular mortality, even a reduction of 2 mm Hg in SBP could lead to ~10% lower stroke mortality in middle age [(30)]. The magnitude of increase in SBP, i.e., 4 mm Hg in 13-year-old individuals (present study) and 4 to 8 mm Hg in 14- or 17-year-old individuals [(10, 11)], may have long-term consequences because it is well known that elevated blood pressure in early life tracks into adulthood [(31)]. Indeed, a recent study showed that SBP measured at a mean age of 12 years was associated with adult fatal/nonfatal cardiovascular events [(32)].
We did not observe any statistically significant difference in PWV at age 13 years across the three trajectories. Previous studies that investigated the association between childhood BMI trajectory and adolescent PWV have reported mixed results. Higher childhood BMI trajectory was shown to be linked to higher PWV in some studies [(12-14)], but not in others [(9, 10)]. This controversy does not appear to be explained by the time period used for childhood BMI trajectory because three studies included data from birth, infancy, and childhood [(9, 10, 14)], whereas the other two studies focused on childhood [(12, 13)]. The patterns of how early-life BMI values were associated with PWV at age 13 years also differed across the three BMI trajectories, similar to what we observed for SBP.
As expected, we found that individuals in the excessive gain group exhibited a significantly greater WC and higher WBC than those in the normal gain group. This suggests that individuals with excessive gain are more prone to central obesity and low-grade inflammation. The impact of early-life BMI on adolescents' WC values and WBC demonstrated an increasing trend with age, and the patterns were similar across three BMI trajectories. Therefore, spending more years with a higher BMI did not appear to have an earlier impact on these variables, as observed for SBP. Instead, WC and WBC were primarily associated with BMI at age 13 years.
Interestingly, previous studies in adults have also shown that the patterns of association with BMI trajectories were different for different cardiovascular risk factors. The risk of adult hypertension has been found to be stronger in trajectory groups that developed high BMI early in life and consequently had obesity for a prolonged duration. Conversely, the absence of BMI stabilization in adulthood, rather than the age of obesity onset, was strongly associated with the risk of adult type 2 diabetes [(33)]. The findings from the present study, corroborating others, suggest that weight loss at any point during the life course, which reduces the time exposed to high BMI, may have a beneficial impact on blood pressure.
Much less is known about the impact of childhood BMI trajectory on mental health problems in adolescents. Previous studies have shown that high childhood BMI trajectory was linked to poorer psychosocial well-being such as low self-esteem at age 11 years [(20, 21)]. However, their BMI trajectory modeling was based on growth data covering ages 3 to 11 years [(20)] or 6 to 11 years [(21)]. Using growth data that encompassed not only childhood but also birth and infancy, the present study revealed that excessive childhood BMI gain was linked to high levels of perceived stress and psychosomatic symptoms at age 13 years. The associations were partly attenuated, and the latter did not remain statistically significant after adjusting for covariates, suggesting that the covariates, especially parental earned income and migrant background, are important contributors for stress and psychosomatic problems. It is known that obesity itself can be a stressful state due to the high prevalence of weight stigma [(34)]. Therefore, we anticipated that, apart from experiencing higher stress, the influence of early-life BMI on stress would manifest earlier in individuals in the excessive gain trajectory who had a longer duration of higher BMI. However, we found that the patterns of association between early-life BMI and stress were similar across three BMI trajectories. Interestingly, a recent study examined the association between BMI trajectories from age 1 to 24 years and adult depression and found that a puberty-onset major increase in BMI trajectory, rather than a persistently high BMI trajectory, was associated with depression at age 24 years [(35)]. The reasons underlying these observations are not clear, but they may be partly explained by the findings that weight stigma experiences increase as children get older and may coincide with the awareness and internalization of cultural norms regarding weight [(36)].
Strengths of the study include the large sample size, multiple measures of growth data covering birth, infancy, the typical period of adiposity rebound, and late childhood to early adolescence, as well as employing group-based trajectory modeling to examine the dynamic changes in BMI over time. The present study goes beyond physical health and incorporates mental health outcomes at age 13 years, offering a comprehensive understanding of the relationship between childhood BMI trajectory and the individual's overall well-being during this critical developmental stage.
Despite its strengths, the present study faces some limitations that should be considered when interpreting the results. The inclusion criteria of having a minimum of five growth data, especially birth and infancy, led to loss of participants with migrant backgrounds and lower family SES, potentially limiting the generalizability of the findings to these specific populations. The study lacks information on early-life mental health, making it difficult to explore potential bidirectional relationships between mental health and BMI during earlier stages of development. Due to lack of data, the study cannot reveal factors influencing childhood BMI trajectory, including breastfeeding status and maternal pre-pregnancy BMI.
CONCLUSION
Our study revealed compelling evidence of associations between childhood BMI trajectories and health outcomes at age 13 years. Specifically, moderate and excessive BMI gain trajectories were linked to adverse health indicators, including increased WC, SBP, stress, and WBC levels. Notably, individuals with excessive BMI gain during childhood exhibited significantly higher SBP levels from as early as age 6 years, emphasizing the importance of early intervention. These findings emphasize the potential burden of high BMI gain during childhood because it appears to be associated with a two- to four-fold increase in cumulative health risks at age 13 years. Our findings stress the importance for researchers and policy makers to look beyond BMI, considering broader health risks from an early age and encompassing both mental and physical well-being.
AUTHOR CONTRIBUTIONS
Yun Chen, Peter Friberg, and Frida Dangardt conceived the study. Yun Chen conducted the statistical analysis. Yun Chen and Peter Friberg interpreted data. Yun Chen drafted the manuscript. Frida Dangardt and Lars Gelander assisted with the interpretation of the results. All authors critically reviewed and approved the final manuscript.
ACKNOWLEDGMENTS
The authors thank the schools, adolescents, and parents who participated in this study, as well as Gun Bodehed Berg, Eva Gronowitz, Ann-Katrine Karlsson, Gustav Andersson, and Sandra Isaksson from Sahlgrenska University Hospital for their excellent efforts in recruiting and examining adolescents.
FUNDING INFORMATION
This study was funded by Swedish Research Council (project number: 2014-10086), the Swedish state under the agreement between the Swedish government and the country councils (the Avtal om Läkarutbildning och Forskning agreement, project number: 239371), the Swedish Research Council for Health, Working Life and Welfare (project number: 2021-00566), Region Västra Götaland, Gothenburg University, Carl Bennet AB, and the Public Health Agency of Sweden. The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
CONFLICT OF INTEREST STATEMENT
The authors declared no conflict of interest.