Molecular targets of isothiocyanates in cancer: Recent advances
Abstract
Cancer is a multistep process resulting in uncontrolled cell division. It results from aberrant signaling pathways that lead to uninhibited cell division and growth. Various recent epidemiological studies have indicated that consumption of cruciferous vegetables, such as garden cress, broccoli, etc., reduces the risk of cancer. Isothiocyanates (ITCs) have been identified as major active constituents of cruciferous vegetables. ITCs occur in plants as glucosinolate and can readily be derived by hydrolysis. Numerous mechanistic studies have demonstrated the anticancer effects of ITCs in various cancer types. ITCs suppress tumor growth by generating reactive oxygen species or by inducing cycle arrest leading to apoptosis. Based on the exciting outcomes of preclinical studies, few ITCs have advanced to the clinical phase. Available data from preclinical as well as available clinical studies suggest ITCs to be one of the promising anticancer agents available from natural sources. This is an up-to-date exhaustive review on the preventive and therapeutic effects of ITCs in cancer.
Abbreviations
-
- AITC
-
- allyl isothiocyanate
-
- BITC
-
- benzyliso-thiocyanate
-
- CYP
-
- cytochrome P450
-
- EGFR
-
- epidermal growth factor receptor
-
- EGG
-
- epigallocatechin gallate
-
- EMT
-
- epithelial to mesenchymal transition
-
- FOXO
-
- forkhead box protein
-
- GST
-
- glutathione-S-transferase
-
- ITC
-
- isothiocyanate
-
- PEITC
-
- phenethyl isothiocyanate
-
- ROS
-
- reactive oxygen species
-
- SFN
-
- sulforaphane
-
- STAT3
-
- signal transducer and activator of transcription 3
-
- TRAIL
-
- TNF-related apoptosis-inducing ligand
-
- VEGF
-
- vascular endothelial growth factor
1 Introduction
Cancer is the leading cause of deaths worldwide, accounting for 7.6 million deaths according to recent statistics. The number of deaths due to cancer is projected to increase to 13.1 million in 2030. These figures implicate marginal efficacy of present standard available therapies to cancer patients, implying the urgent need to identify new strategies/agents that can be included in cancer preventive or therapeutic regimen.
Historical evidence purports nature being a prodigious source of many drugs and drug leads for various ailments, including cancer 1. Several epidemiological studies have been published over the past few decades that indicate a strong correlation between intake of fruits and vegetables and reduced risk of cancer 2-4. Basic benefits of using bioactive dietary agents are low cost, well-known applications in traditional medicinal system, accessibility, and minimal or no toxicity.
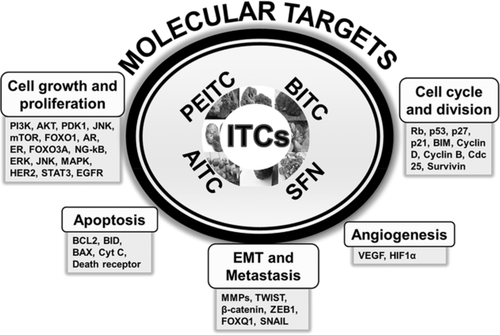
Epidemiological and case–control studies continue to support the notion that consumption of cruciferous vegetables reduces the risk of developing various types of cancers, such as pancreatic, prostate, ovarian, and breast 5-11. Isothiocyanates (ITCs) occur in cruciferous vegetables as glucosinolates and are converted to ITCs by the action of the enzyme myrosinase. ITCs from these vegetables are also released by cutting or chewing or by intestinal microflora present in humans 12 (Fig. 1). ITCs have been shown to have substantial chemopreventive activity against various human malignancies 13, 14. Some of the widely studied ITCs that have potent anticancer effects are allyl isothiocyanate (AITC), benzylisothiocyanate (BITC), phenethylisothiocyanate (PEITC), and sulforaphane (SFN). Unless stated, most of the studies mentioned in this article used 95–98% pure ITCs for evaluating anticancer effects. This exhaustive review highlights the specificity of ITCs against various targets in cancer.
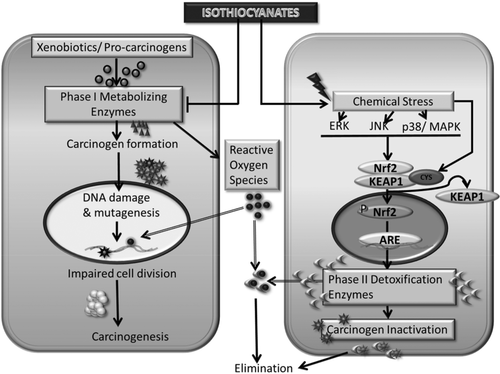
2 Chemoprevention by ITCs
An individual's susceptibility to cancer is determined by numerous factors, including maintenance of a critical balance between phase I and II enzymes. Phase I primarily consists of cytochrome P450 enzymes that play an important role in metabolizing the xenobiotics and carcinogens. However, in this process, several chemicals or procarcinogens are activated or converted into highly reactive electrophilic metabolites. The generated electrophiles can disturb the genomic stability by causing DNA damage. Chemopreventive effects of ITCs are exerted by inhibition of the bioactivation of carcinogens by phase I drug metabolizing enzymes (Fig. 1) 15-18. The mechanistic studies by Morse et al. and others indicate that administration of ITCs prevents the tumor promoting effects of various chemical carcinogens in different animal models 19-21. PEITC has been shown to possess significant chemopreventive properties against tobacco-induced carcinogens in rodent models of lung and esophageal cancers 22, 23. AITC also inhibits NNK (a tobacco-derived carcinogen) induced tumors in rats 24. Similar to other ITCs, AITC induces phase II detoxifying enzymes quinone reductase and glutathione-S-transferase (GST) in the animal tissues 25. Cytochrome P450E1 and N-dimethylnitrosoamine demethylase are major enzymes that cause bioactivation of tobacco specific nitrosoamines. These enzymes can be inhibited by glutathione conjugates of ITCs 26. ITCs also inhibit various isoforms of cytochrome P450 (CYP450) directly, for example, BITC suppresses cytochrome P450 2E1, while SFN inhibits cytochrome P450 1A2 27, 28. SFN also has been shown to inhibit steroid and xenobiotic receptor, a nuclear hormone receptor that regulates expression of CYP3A4 29. Zhou et al. showed specific antagonism by SFN to inhibit drug clearance due to steroid and xenobiotic receptor induced activity of CYP3A4.

Phase II enzymes, such as GST, NADPH quinine oxidoreductase, and UDP-glucuronosyltransferases play an important role in detoxifying carcinogens as well as xenobiotics. ITCs are known to induce phase II enzymes that further explain the cancer chemopreventive activity of ITCs 28, 30-34. GST catalyzes the conjugation of glutathione with electrophilic compounds making them more water-soluble and facilitating their removal from the body 35, 36. It is well known that ITC–GSH conjugate is exported out by MRPs 37. As a result of continuous conjugation and efflux of the conjugate, intracellular GSH level drops significantly within 3 h of ITC treatment. This time also coincides with the induction of GST and mitogen-activated protein kinase 38. Due to nonavailability of GSH, ITCs bind with other vital cellular proteins causing their thiocarbamoylation 37. Although being electrophilic, no studies have reported direct binding of ITCs to cellular DNA 39. In addition, PEITC has been shown to demethylate the promoter region of GSTP1 to induce the expression of GSTP1 40. ITCs also induce GSTs that scavenge reactive oxygen species (ROS) 41. The action of phase II enzymes is primarily regulated by the antioxidant or electrophile response element. The latter can be activated by the transcription factors, such as the basic leucine zipper (bZIP) Nrf2, that heterodimerizes with Maf G/K to exhibit its effects. ITCs induce the Nrf2 transcription factor to activate antioxidant response element that in-turn translates in the activation of mitogen activated protein kinase ERK/JNK, PI3K, and PKC 41-44. SFN induces epigenetic modifications by inhibition of histone deacetylase (HDAC) 1, 4, 5, and 7. In addition, SFN-induced demethylation at the promoter region of Nrf2 causes enhanced expression of Nrf2 in the TRAMP mice model for prostate cancer 45. SFN's chemopreventive effects mainly depend on induction of phase II enzymes through the activation of antioxidant response elements, such as Keap1/Nrf2 31, 46, 47. SFN-mediated induction of Nrf2 was found to be through the activation of heme oxygenase 1 and inhibition of p38 in hepatoma cells 42. Furthermore, several studies have shown induction of thioredoxin reductase as well its substrate thioredoxin by SFN in various cancer cell lines 48-50. Inhibition of key survival pathway, such as NF-κB and AP-1, by ITCs also contributes to the chemopreventive effects of ITCs 44.
ITCs thus modulate phase I and II enzymes to reduce the bioactivation of carcinogens as well as enhanced detoxification. This dual mechanism leads to reduced binding of carcinogens with the DNA and hence less mutagenic or carcinogenic effects.
These studies suggest existence of mutually distinct mechanisms of chemopreventive and chemotherapeutic effects of ITCs. Specific targets have been identified that mediate chemotherapeutics effects of different ITCs against human cancers 30, 41, 44, 51-53. These targets might vary with the structural variations among ITCs as well as the nature and origin of cancer. Several studies demonstrate that ITCs modulate cancer cell signaling by acting on multiple targets to suppress growth and progression of cancer cells 41, 53.
3 Uptake of ITCs by cancer cells
The uptake of anticancer agents is an important limiting factor for efficacy. Most of the ITCs can be taken up by the cells through passive diffusion. The cellular uptake of ITCs correlates with the induction of phase II detoxifying enzymes important for chemopreventive activity. It was observed that the intracellular concentrations of ITCs can reach up to 100- to 200-fold higher than the extracellular concentrations. For example, when hepatoma cells were incubated with 100 μM SFN for about 30 min, the intracellular concentrations reached about 6.4 mM 38. The magnification of intracellular concentration was due to the formation of dithiocarbamates, as ITCs rapidly conjugate with thiols, particularly GSH (Fig. 2). Uptake of ITCs in cancer cells was GSH dependent. The uptake was reduced if GSH concentration was increased. The ITC–GSH conjugate being the substrate of MRPs is transported out of the cells (Fig. 2). This mechanism of uptake and cellular accumulation can be vital in designing the dose regimens of these ITCs. The dose will require the adjustment for high accumulation as well as to compensate for the rapid export through transport proteins, such as MRPs 54. The shuttling of ITC–GSH causes prompt depletion of intracellular GSH, resulting in the perturbation of cellular redox homeostasis. This could be one plausible mechanism of ROS generation by ITCs.
4 Chemotherapeutic targets
4.1 Benzylisothiocyanate (BITC)
BITC occurs in cruciferous vegetables like cabbage, mustard, watercress, cauliflower, and horseradish that constitute a significant proportion of our daily diet (Fig. 3). Accumulating evidence suggests the anticancer effects of BITC through suppression of initiation, growth, and metastasis of human cancers in various mouse models 55-61. BITC induces apoptosis selectively in cancer cells through multiple mechanisms 55, 60, 62. Major anticancer effects of BITC are due to the generation of ROS. BITC causes cell-cycle arrest as well as disruption of mitochondrial membrane potential to initiate mitochondrial pathway of apoptosis 57, 63. Studies from our laboratory have demonstrated the anticancer effect of BITC against pancreatic tumor growth via inhibition of key molecules overexpressed in cancer, such as protein kinase B (AKT) signal transducer and activator of transcription 3, HDAC, and nuclear factor kappa B (NFκB) (Table 1) 7, 55, 56, 59. The targets of BITC can be divided as per their role against cancer-promoting mechanisms.
| Compounds | Efficacy | Organ | Mechanism | Dose/duration | Cell line | References | |
|---|---|---|---|---|---|---|---|
| BITC | Antiangiogenesis | Pancreas | ↓VEGF, MMP-2, HIF-α ↑RhoB ↓STAT3 phosphorylation (Tyr-705), HIF-α, VEGFR-2, VEGF, MMP-2, CD31, RhoC |
In vitro In vivo |
5, 10, 20 μM/24 h 12 μmol/40 days |
BxPC-3, PanC-1 | 77 |
| BITC | Antiangiogenesis | Breast | ↓CD31, VEGF, VEGFR | In vitro In vivo |
2.5, 5, 7.5 μM/24 and 48 h 6 and 9 μmol/14 days |
MDA-MB-231 | 78 |
| BITC | Apoptosis | Pancreas | ↓PI3K, AKT, PDK1, mTOR, FOXO1, FOXO3a ↑Bim, p27, and p21 |
In vitro In vivo |
5, 10, 20 μM/24 h 12 μmol/45 days |
BxPC-3, PanC-1 | 55 |
| BITC | Apoptosis | Breast | ↓mTOR, FOXO1 | In vitro | 2.5, 5 μM/6 and 9 h | MDA-MB-231, MCF-7, MDA-MB-468, BT-474, BRI-JM04 | 68 |
| BITC | Apoptosis | Pancreas | ↓NF-kappaB, cyclin D1, ↑HDAC1, and HDAC3 | In vitro | 10 μM/24 h | BxPC-3, Capan-2 | 56 |
| BITC | Apoptosis | Pancreas | ↑ERK, JNK, P38, ROS | In vitro | 10 μM/24 h | Capan-2, MIA PaCa-2 | 57 |
| BITC | Apoptosis | Pancreas | ↑ATR (Ser-428), Chk2 (Thr-68), Cdc25C (Ser-216), Cdk-1 (Tyr-15), and induction of p21Waf1/Cip1 ↓NF-kappa B |
In vitro | 2.5, 5, 10 μM/24, 48 h | BxPC-3, PanC-1 | 58 |
| BITC | Apoptosis | Pancreas | ↓STAT3, MCL-1, BCL-2 | In vitro In vivo |
5–40 μM/24 h 60 μmol/wk /6 wk |
BxPC-3, AsPC-1, Capan-2, MIA PaCa-2, Panc-1 | 59 |
| BITC | Apoptosis, cell-cycle arrest |
Brain | ↑ROS | In vitro | 10, 20 μM/24 h | U87MG | 82 |
| BITC | Apoptosis | Pancreas | ↑H2A.x, p21, Chk2 ↓CyclinB1, Cdc2, Cdc25C |
In vivo | 10 μmol/L/24 h | Capan-2 | 60 |
| BITC | Apoptosis, cell-cycle arrest |
pancreas | ↓Cdk1, cyclin B1, Cdc25B, NF-κB ↑IkappaBa |
In vitro | 5, 10 μM/24 h | BxPC-3 | 61 |
| BITC | Apoptosis | Ovary | ↓BCL-2, ERK1/2, and AKT ↑Caspase-3, caspase-9, Bax, JNK1/2, and p38 |
In vitro | 10 μM/48 h | SKOV-3, KLE, SW954, SW756, HL60 | 62 |
| BITC | Apoptosis, cell-cycle arrest |
Bone | ↓Cyclin A, cyclin B1, ↑Chk1, p53, caspase-9, and caspase-3, ROS |
In vitro | 7.5 μM/0, 12, 18, and 24 h | U-2 OS | 79 |
| BITC | Antimetastasis | Lung | ↓MMP-2, Twist, β-catenin, AKT, and NF-κB ↑ROS |
In vitro | 5 μM/24 h | L9981 | 80 |
| BITC | Antitumorigenesis | Leukocyte | ↓Hydrogen peroxide, ROS | In vitro In vivo |
1, 10, 100 μM/24 h 81 or 810 nmol/20 wk |
HL-60 | 81 |
| PEITC | Apoptosis | Breast | ↓HER2, EGFR, STAT3, BCL-XL, XIAP, ROS ↑Bax, Bim, HER2 ↓HER2, EGFR, STAT3 |
In vitro In vivo |
10 μM/24 h 12 μmol/33 days |
MDA-MB-231, MCF-7 | 95 |
| PEITC | Apoptosis | Prostate | ↓BCL-2, XIAP ↑Bax, Bak |
In vitro In vivo |
1 μM/24 h 9 μmol/38 days |
PC-3, DU145 | 97 |
| PEITC | Apoptosis | Leukemia | ↑ROS, NO ↓GSH |
In vitro | 10 μM/1–6 h | HL-60 | 98 |
| PEITC | Apoptosis | Breast | ↑ROS, caspases 9 and 3 ↓GSH, Bax |
In vitro | 20 μM/6 h | MDA-MB-231, MCF-7 | 99 |
| PEITC | Apoptosis | T-cell | ↑JNK | In vitro | 20 μM/24 h | Jurkat | 101 |
| PEITC | Apoptosis | Lung | ↑JNK, p38, Erk1/2, AP-1 | In vivo | 15 μM/g/140 days | 102 | |
| PEITC | Apoptosis | Colon | ↓SOS-1, PKC, ERK1/2, Rho A, MMP-2 and -9, GRB2, NF-κB, iNOS, COX-2 | In vitro | 2.5 μM/24, 48 h | HT29 | 103 |
| PEITC | Antimetastasis | Liver | ↓MMP-2,MMP-9 ↑TIMP1, 2 |
In vitro | 0.1–5 μM/24 h | SK-Hep1 | 104 |
| PEITC | Antiangiogenesis | Prostate | ↓VEGF, VEGF receptor 2, AKT, EGF, G-CSF |
In vitro | 4 μM/24 h | HUVEC, PC-3 | 105 |
| PEITC | Antiangiogenesis | Breast | ↓HIF-1α, CAIX, GLUT1, BNIP3, VEGF-A, 4E-BP1 | In vitro | 16 μM/24 h | MCF7 | 106 |
| PEITC | Apoptosis, cell-cycle arrest |
Prostate | ↑p21WAF-1/Cip-1 and p27Kip1 ↓Cyclins D and E, Rb |
In vivo | 8 μmol/g/9 wk | BALB/c male mice | 122 |
| PEITC | Apoptosis, cell-cycle arrest |
Oral squamous cell | ↑p53, p21, p17, Bax, Bid ↓cyclin E, CDK2, BCL-2 |
In vitro | 5 μM/72 h | HSC-3 | 116 |
| PEITC | Apoptosis | Multiple myeloma | ↑PARP, caspase-3 and caspase-9, c-jun, HSP27 ↓Mcl-1, X-IAP, c-IAP, and survivin |
In vitro | 2.5, 5, and 10 μM/12, 24, 48 h | MM.1S | 51 |
| PEITC | Apoptosis | Breast | ↑p57 Kip2, p53, BRCA2, IL-2, and ATF-2 | In vitro | 3 μM/48 h | MCF-7 | 124 |
| PEITC | Apoptosis, cell-cycle arrest |
Prostate | ↑p53, WEE1, caspase-3, caspase-8, caspase-9 ↓CDC25C |
In vitro | 20 μM/24, 48 h | DU 145 | 117 |
| PEITC | Cell-cycle arrest | Lung | ↓Cell growth | In vitro | 3, 6, 9 μM/24, 48, 72 h | A549, H1299 | 125 |
| PEITC | Apoptosis | Ovary | ↓EGFR, AKT, p-GSK ↓Tumor growth |
In vitro In vivo |
40 μM/24 h 12 μmol/42 days |
SKOV-3, OVCAR-3, TOV-21G | 109 |
| PEITC | Apoptosis | Oral cancer | ↑Caspase-3, caspase-8, BID, DR5 | In vitro | 10 μM/48 h | HN22 | 113 |
| PEITC | Apoptosis | Cervical cancer | ↑DR4, DR5, caspase-3, PARP ↓ERK1/2 |
In vitro | 5 μM/48 h | HEp-2, KB | 114 |
| PEITC | Apoptosis | Breast | ↑Caspases 7 and 9, PARP ↓BCL-2, XIAP |
In vitro | 3–30 μM/24 h | MCF-7 | 118 |
| PEITC | Apoptosis | Breast | ↓ER-α36, ERK 1/2 | In vitro | 10 μM/48 h | MCF7, H3396, MDA-MB-231,SK-BR-3 | 110 |
| SFN | Apoptosis | Liver | ↑TrxR1 | In vitro | 12 μM/24 h | HepG2 | 49 |
| SFN | Apoptosis | Breast | ↑TrxR1 | In vitro | 3, 6 μM/24 h | MCF-7 | 50 |
| SFN | Apoptosis | Prostate | ↑Ac-histone H4, Bax, P21, ↓HDAC |
In vitro | 15 μM/24 h | BPH-1, LnCaP, PC-3 | 133 |
| SFN | Apoptosis, cell-cycle arrest |
Bladder | ↑p27 | In vitro | 5–20 μM | T24 | 147 |
| SFN | Apoptosis, cell-cycle arrest |
Colon | ↑Cyclins A and B1, bax, cytochrome c | In vitro | 15 μm/24 h | HT29 | 148 |
| SFN | Apoptosis, cell-cycle arrest |
Lymphoblastic leukemia | ↑Caspases 3, 8, and 9, p21 ↓Cdc2/Cyclin B1, AKT, mTOR |
In vitro | 7.5 μM/24 h | LCL, Nalm-6, Jurkat, KOPTK1 | 149 |
| SFN | Apoptosis | Bladder | ↓Tumor volume ↑Caspase 3 and cytochrome c |
In vivo | 12 mg/kg/5 wk | Athymic mice | 135 |
| SFN | Apoptosis | Prostate | ↓p65, VEGF, cylcin D1, and BCL-X | In vitro | 20 and 30 μM/24 h | PC-3 | 136 |
| SFN | Cell-cycle arrest | Colon | ↑ERK, JNK, p38, p21 ↓Cyclin D1 |
In vitro | 6.25, 12.5, 25, 50, and 100 μM/24 h | HT-29 | 150 |
| SFN | Apoptosis | Colon | ↑ERK1/2 and AKT | In vitro | 20, 30 μM/24 h | Caco-2 | 151 |
| SFN | Apoptosis | Breast | ↑Caspase-8, caspase-3, cytochrome c ↓BCL-2, HDAC, ERalpha, EGFR, EGFR2 |
In vitro | 0, 5, 15, or 25 μmol/L for 48 h | MDA-MB-231, MDA-MB-468, MCF-7, T47D | 137 |
| SFN | Apoptosis | Prostate | ↓IAP, cIAP1, cIAP2, XIAP, p65 ↑Apaf-1, E2F1 |
In vitro | 20 μM/24 h | LNCaP, PC3 | 143 |
| SFN | Antiangiogenesis, antimetastasis | Pancreas stem cell | ↓Nanog, Oct-4, VEGF, platelet derived growth factor receptor alpha, ZEB-1 | In vivo | 0–20 mg/kg/6 wk | non-obese diabetic (NOD)/severe combined immunodeficiency (SCID)/IL2Rgamma mice | 144 |
| SFN | Apoptosis | prostate | ↑ROS, Fas, caspase-8, Bid | In vitro | 40 μM/4 h | PC-3 | 145 |
| SFN | Antimetastasis | Oral carcinoma | ↓MMP-1, MMP-2 | In vitro | 1 μM/24 h | YD8, YD10B, YD15 | 152 |
| SFN | Apoptosis | Breast | ↓Tumor growth | In vitro In vivo |
25 or 50 mg/kg/24 days | KPL-1 Athymic mice |
153 |
| SFN | Antimetastasis | Bladder | ↓ZEB-1, SNAIL ↑E-cadherin |
In vitro | 0–20 μM/24 h | T24 | 154 |
| AITC | Apoptosis, cell-cycle arrest |
Prostate | ↓BCL-2, cyclin B1, Cdc25B, Cdc25C ↑BID |
In vivo | 10 μmol/26 days | Nude mice | 168 |
| AITC | Antiproliferation | Colon | ↓Mitosis | In vitro | 12 μM/24 h | HT-29 | 164 |
| AITC | Apoptosis | Prostate | ↑AP-1, ERK1/2, JNK1/2, Elk-1, and c-Jun | In vitro | 50 μM/24 h | PC-3 | 165 |
| AITC | Apoptosis, cell-cycle arrest |
Bladder | ↓α- and β-Tubulin ↑cytochrome c, caspase-9, caspase-3, BCL-2, JNK |
In vitro | 30 μM/24 h | UM-UC-3 | 167 |
| AITC | Antimetastasis | Liver | ↓MMP-2/-9 | In vitro | 0.1-5 μM/24 h | SK-Hep 1 | 169 |
- ER, estrogen receptor; Rb, retinoblastoma protein.
4.1.1 Cell proliferation and growth
Phosphoinositide 3 kinase (PI3K)/AKT pathway has been shown to be activated in about 59% of the pancreatic tumors, and it also promotes cell division in other cancer forms 64, 65. PI3K stimulation results in the phosphorylation of AKT at Thr-308 and Ser-473 through phosphatidylinositol-dependent kinase (PDK1) activation 66. Studies by Boreddy et al. have shown that BITC inhibits PI3K/AKT signaling. BITC prevents the phosphorylation of AKT at both Thr-308 and Ser-473 along with suppression of PI3K (Tyr-458), PDK1 (Ser-241), mammalian target of rapamycin (mTOR) (Ser-2448) 55. The inhibition of mTOR signaling by BITC was also observed in human prostate cancer cells 67. These studies showed that BITC had negligible effect on normal human pancreatic ductal epithelial 6 cells, suggesting the specificity of BITC toward cancer cells 55. These results also showed upregulation of proapoptotic proteins, such as Bim, p21, and p27, due to nuclear accumulation of Forkhead Box Protein 1 (FOXO1). Inhibition of phosphorylation of FOXO1 (Ser-256) and FOXO3a by BITC was due to the dephosphorylation of AKT in pancreatic cancer cells 55. Interestingly, BITC also reduced acetylation of FOXO proteins by reducing the level of CREB-binding protein (CBP) protein 55. FOXO1 suppression was also shown to be responsible for BITC initiated cell death in breast cancer cells 68.
NF-κB is a transcription factor that regulates cellular inflammation, immunity, and proliferation 69, 70. Batra et al. showed that BITC-mediated downregulation of HDAC1 and HDAC3 expression was associated with the acetylation of NF-κB in pancreatic cancer cells 56. BITC treatment significantly suppressed the phosphorylation of NF-κB at Ser-276 and Ser-536 in BxPC-3 and Capan-2 cells in a dose and time dependent manner 56, 61. BITC reduced NF-κB protein expression in BxPC-3 cells but not in Capan-2 cells, indicating that BITC acts differentially on different cell lines 56. The Capan-2 cells have wild-type p53, whereas BxPC-3 cells harbor mutated p53, hence the role of p53 in BITC-mediated downregulation of NF-κB expression cannot be ruled out and remains to be explored further. The mechanistic studies revealed that neither I kappa B (IκB) phosphorylation nor expression levels were altered by BITC, whereas IκB kinase (IKK) expression was downregulated. Hence, downregulation of IKK by BITC treatment could be the reason for inhibition of NF-κB phosphorylation (Ser-536) 56, 61.
STAT3 is hyperactivated in significant number of malignancies, such as breast cancer, pancreatic cancer, gastric cancer, and head and neck cancer as well as in cancer stem cells where it enhances tumor aggressiveness and progression 71-73. Sahu and Srivastava have shown that BITC suppresses the phosphorylation (Tyr-405 and Ser-727) and expression of STAT3 in pancreatic cancer cells lines, such as BxPC-3, PanC-1, Capan-2, and MIA PaCa-2 59. The role of STAT3 in the anticancer effects of BITC was confirmed by STAT3α overexpression or through activation by IL6, which abrogates the effects of BITC (Table 1) 59.
4.1.2 Angiogenesis
The growing tumors are nourished through processes such as angiogenesis and neovascularization. Angiogenesis is mainly promoted by hypoxia inducible factor (HIF-1α) and vascular endothelial growth factor (VEGF) 74. STAT3 has been shown to be a positive regulator of VEGF and HIF-1α 75, 76. Boreddy et al. demonstrated that BITC inhibits angiogenesis in chicken chorioallantoic membrane and rat aortic ring assay 77. This clearly indicates the antiangiogenic potential of BITC. BITC-mediated suppression breast cancer xenografts was associated with inhibition of critical angiogenic factors, such as CD31 and VEGF 78. Furthermore, BITC downregulated the expression of HIF-1α; vascular endothelial growth factor receptor (VEGFR); MMP-2 (where MMP is matrix metalloproteinase); Rho A; Rho C; and ras-related C3 botulinum toxin substrate 1 (RAC1), 2, and 3 in pancreatic, but the inhibition of VEGF, HIF-1α, and MMP-2 was not observed in STAT3 overexpressing BxPC-3 cells 77. This undoubtedly suggests that inhibition of tumor growth and angiogenesis by BITC correlates with STAT3 inhibition.
4.1.3 Mitochondrial cell death
Generation of ROS is an important mechanism to induce cell death, specifically in cancer cells. As shown by us and others, BITC significantly induced ROS generation in pancreatic cancer cells and glioma as well as other cancer models 57, 79-82. ROS generation leads to disruption of mitochondrial membrane potential and release of proapoptotic molecules resulting in activation of caspase-mediated cell death 63, 81, 83. Furthermore, BITC-mediated downregulation of myeloid cell leukemia marker 1 (MCL-1) in human leukemia cells was also found to be correlated with the mitochondrial pathway of apoptosis 84.
4.1.4 Cell-cycle arrest
ROS induced by BITC also damage DNA and causes G2/M cell-cycle arrest as detected through increased phosphorylation of H2A.X (Ser-139) and ChK2 (Thr-68) 57, 60, 61. Antioxidants block the effects of BITC confirming the role of ROS in cell-cycle arrest 57. BITC treatment increased the phosphorylation of the MAP kinases, such as ERK (Thr202/Thy204), JNK (Thr183/Tyr185), as well as p38 (Thr180/Tyr182), in a dose-dependent fashion 57, 62. It was later found that BITC-induced cell-cycle arrest was executed only through ERK, while the other MAP kinases were playing role in the induction of apoptosis 57.
4.1.5 Invasion and metastasis
Metastasis is initiated by key regulators, such as matrix metalloproteinases, Twist, and β-catenin. A study showed that BITC treatment inhibited cell migration and invasion in lung cancer cells. This was accompanied with reduced expression of MMP-2, Twist, and β-catenin 80. Another study showed that oral administration of 5 and 10 mg/kg BITC suppressed the expression of MMP-2 and MMP-9 in the sera and lungs of mice injected with 4T1 breast cancer cells 85. BITC also inhibits the process of epithelial to mesenchymal transition through FOXQ1 suppression in breast cancer cells, leading to reduced metastatic potential 86. The data available for antimetastatic effects of BITC are insufficient to prove the antimetastatic efficacy. Hence, additional elaborate studies are required to establish the role of BITC in metastasis.
4.1.6 In vivo studies
Our in vivo studies indicated that BITC is well tolerated at a dose of 12 μmol/day (72 mg/kg) in mice. Interestingly, in vivo tumor growth was markedly arrested by BITC treatment in athymic nude mice as compared to controls 59. These results showed that after 6 wk of 12 μmol/day BITC treatment by oral gavage, average tumor volume in BITC-treated mice was about 48% less as compared to the control group 59. LC-MS analysis showed that after 46 days of BITC (12 μmol/day) treatment, mean concentration of 6.5 ± 0.1 μmol/L (39 mg/L; n = 10) and 7.5 ± 0.3 μmol/g (45 mg/g; n = 10) BITC was observed in the plasma and tumors of treated mice, respectively 55. These results suggest a reasonable bioavailability of BITC and also that the therapeutic concentration could be achieved in vivo by oral administration. No untoward side effect or change in body weight was observed, suggesting that 12 μmol/day BITC was relatively safe. Furthermore, suppression of in vivo angiogenesis by 12 μmol/day (72 mg/kg) treated mice was observed by reduction of hemoglobin content by 76% in matrigel plugs implanted in the mice as well by 61% in the excised tumor xenografts, as compared to respective controls 77. These results signify the potential antitumor and antiangiogenic effects of BITC. The molecular targets of BITC have been described in detail in Table 1. Interestingly, dietary BITC also suppressed the growth of cancer stem cell in mouse mammary tumor virus-neu (MMTV-neu) breast cancer transgenic mice model along with inhibition of major stem cell markers, such as Oct4, SOX-2, and Nanog 87. In contrast, the activation of NOTCH2 signaling by BITC was found to impede the therapeutic benefits of BITC 88. A recent study from our group showed that the absorption and bioavailability of BITC can be enhanced by making the nanoemulsion of BITC 89.
4.1.7 Toxicity studies
No major evidence of BITC side effect exists for the doses that are commonly used for anticancer studies. A study has shown that oral administration of BITC (0, 50, 100, and 200 mg/kg) for 4 wk caused reduction in body weight and reduced food consumption only at highest doses 90. In addition, the study revealed that BITC treatment caused increase in serum cholesterol and decrease in triglycerides, accompanied with renal dysfunction. Furthermore, in this study BITC treatment reduced the weight of almost all the organs except the adrenals, where the weight was increased. Some transitory hematological changes, such as reduced hemoglobin and lymphocyte count, with increased platelets, eosinophils, and neutrophils were observed in BITC-treated rats. It is pertinent to note that no significant signs of toxicity were observed at the dose of 50 mg/kg. Although these changes were observed at higher doses (100 and 200 mg/kg) of BITC, no mortality was reported 90. The high doses such as 100–200 mg/kg BITC, which were associated with some side effects, are unlikely to be used for antitumor effects. So far the therapeutic doses of BITC, which suppresses in vivo tumor growth, are much lower and not associated with any side effects and hence can be considered relatively safe.
4.2 Phenethylisothiocyanate (PEITC)
PEITC is another isothiocyanate that occurs conjugated with glucosinolate in many cruciferous plants. PEITC is abundantly present in plants, such as watercress, garden cress and in some noncruciferous plants, such as turnips and radishes 30, 91. Watercress is the most prolific source of PEITC, which can release approximately 2–6 mg PEITC/ounce (0.07–0.21 mg of PEITC/g) in humans 91, 92.
The effective concentrations of PEITC vary from 0.12 to 14 μM 93, 94. Like BITC, PEITC also induces ROS generation selectively in cancer cells 95, 96. Mechanistic studies have shown that PEITC disrupts mitochondrial electron transport chain by inhibiting complex I and III activity and reduces oxygen consumption rate in prostate cancer cells 97, 98. Furthermore, PEITC is known to inhibit ROS-detoxifying mechanisms to enhance ROS-mediated cytotoxicity 96-98. This was further proven in cells with varying levels of anti-ROS mechanisms that showed differential sensitivity toward PEITC 99, 100.
Two general mechanisms that have been identified for the anticancer activity of PEITC include cell-cycle arrest and apoptosis induction 44, 101, 102. Few studies also suggest antiangiogenic and antimetastatic effects of PEITC by mechanisms similar to BITC 80, 103-106. PEITC has been shown to act on about 30 different targets present in cancer cells (Fig. 3) 107. Mi et al. have shown that PEITC alters the function of critical amino acids of proteins and peptides through covalent interactions 107.
4.2.1 Cell proliferation and growth
Studies suggest that PEITC has multiple targets, such as AKT, epidermal growth factor receptor (EGFR), and human epidermal growth factor receptor 2 (HER2), in cancer cells that promote antiapoptotic mechanisms in cancer cells. As discussed earlier, AKT (protein kinase B) is frequently overexpressed in cancers and regulated by oncogenes, such as EGFR and HER2 108. Our studies demonstrated that PEITC inhibits EGFR and HER2 in ovarian and breast cancer cells 95, 109. PEITC caused significant inhibition of activated EGFR (Tyr1068) to suppress the growth of ovarian cancer cells. Furthermore, PEITC reduced the phosphorylation of AKT and mTOR expression 109. In this study, PEITC also disrupted the complex of Raptor and Rictor with mTORC1 and mTORC2 109. In another study, we observed inhibition of HER2 and AKT in breast cancer cells. These observations suggest that PEITC inhibits AKT activation by suppressing EGFR and HER2 expressions to suppress antiapoptotic signaling in cancer cells (Table 1). Furthermore, PEITC also inhibits HDACs, the major epigenetic regulators resulting in the inhibition of androgen receptor in prostate cancer cells 40.
4.2.2 Angiogenesis
Similar to BITC, PEITC also inhibits VEGF, a major promoter of angiogenesis. Xiao and Singh showed suppression of VEGF by PEITC, which was later shown to be mediated through suppression of HIF-1α 105, 110-112. Based on the evidence provided in these studies, it can be suggested that PEITC inhibits angiogenesis mainly by inhibiting VEGF.
4.2.3 Mitochondrial cell death
Accumulating evidence from several studies showed induction of apoptosis signaling by PEITC. PEITC has been shown to activate death receptors and Fas-mediated extrinsic apoptotic pathway in oral and cervical cancer cells 113-115. PEITC treatment also resulted in the activation of intrinsic pathway of apoptosis. PEITC modulates mitochondrial proteins, such as BCL-2, BID, and BAX, causing the release of cytochrome c into cytosol to induce intrinsic apoptosis pathway 94, 116-119. However, the release of cytochrome c by PEITC treatment into cytosol to induce apoptosis was contradicted by a study conducted by Wu et al. 120. Further in-depth studies are thus required to delineate the exact mechanism of PEITC.
4.2.4 Cell-cycle arrest
PEITC as well as its N-acetyl cysteine conjugate causes activation of retinoblastoma protein in prostate cancer cells, leading to attenuation of cell-cycle progression 39, 121. Furthermore, a G0/G1 phase cell-cycle arrest by PEITC was associated with activation of p53 in oral squamous carcinoma cells, in multiple myeloma, osteogenic sarcoma and breast cancer cells, and G2/M cell-cycle arrest in prostate cancer cells 51, 52, 116, 117, 122, 123. Interestingly, lung carcinoma cells expressing mutated p53 were shown to be more sensitive to PEITC as compared to cells with wild-type p53 expression 107, 124.
4.2.5 Invasion and metastasis
PEITC inhibits cancer cell invasion by inhibiting MMPs and suppresses activity of ERK and NF-κB to inhibit metastasis 103, 104. We recently demonstrated in vivo antimetastatic potential of PEITC using a unique mouse model of breast cancer metastasis 94. This model utilizes MDA-MB-231-Luc2 brain-seeking breast cancer cells that lodge in the brain from blood circulation when injected into the left ventricle of mouse heart. These cells later grow to form metastatic tumors in brain. Oral administration of 10 μmol PEITC (65 mg/kg) for 10 days significantly prevented the seeding of breast cancer cells into the brain in this model. We also observed that PEITC administration suppressed the growth of metastasized tumor in the brain and enhanced the survival of mice bearing tumors in the brain 94. This was the first evidence of in vivo antimetastatic effects of PEITC in breast cancer model, but further studies are required to establish similar efficacy in other cancer forms. The molecular targets of PEITC have been described in detail in Table 1.
4.2.6 In vivo studies
PEITC-mediated inhibition of anti-apoptotic pathways was observed in the preclinical mouse model studies 125. PEITC has a dose-dependent bioavailability of about 70–110% by oral administration, which is a probable reason for in vivo efficacy 126. Treatment of brain metastatic breast cancer has always been a problem due to the presence of blood–brain barrier. Organ distribution study has revealed a fair availability of PEITC in brain, suggesting better chances of PEITC to cross blood–brain barrier 127. This could be the reason for the antimetastatic effects of PEITC 94. These studies indicate a high antitumor efficacy of PEITC in all organs including brain by oral administration. Orally administered PEITC causes significant inhibition of major oncogenic pathways, such as EGFR, HER2, and AKT, in various in vivo cancer models leading to tumor growth suppression 94, 95, 109, 128. These results clearly reenforce potential for in vivo efficacy of PEITC.
4.2.7 Toxicity studies
In addition to the beneficial effects, it is also essential to evaluate the probable side effects of PEITC. It was observed that intra-peritoneal (i.p.) administration of 80 and 160 mg/kg PEITC caused increase in body weight of mice, but reduction in the weights of liver and spleen 129. Interestingly, preventive effects of PEITC were observed on acetaminophen-induced hepatotoxicity and mortality 130. These mutually contradicting observations make it important to establish a well-defined toxicity profile of PEITC using appropriate controls and population size.
4.2.8 Clinical studies
Three clinical studies are currently under progress to test anticancer effects in humans. A phase I lung cancer study with PEITC conducted at MD Anderson Cancer Center was recently completed; however, the findings have not yet been published. Another phase I clinical study at the same institution has been planned to test the anti-leukemic effects of PEITC. Notably, a recent phase I clinical trial (NCI CN-55120) reported that 10 μM PEITC can be achieved in the plasma after intake of 200 mg PEITC orally in human volunteers 131. A phase II trial is also under progress in lung cancer patients at the Masonic Cancer Center, University of Minnesota in collaboration with the National Cancer Institute. The outcomes of these studies will provide data on the efficacy and toxicity of PEITC in humans.
4.3 Sulforaphane (SFN)
SFN is an isothiocyanate mainly present in broccoli and Brussels sprouts. Studies have shown that SFN is highly effective in blocking carcinogenesis (Fig. 3). SFN inhibits HDAC activity to promote cell-cycle arrest and apoptosis in Nrf2−/− cells suggesting Nrf2 independent mechanism of SFN 132, 133.
4.3.1 Cell proliferation and growth
SFN acts on certain molecular targets, such as survivin and NF-κB, that are vital for cancer cell survival 134, 135. SFN induces apoptosis in breast cancer cells by the inhibition of estrogen receptor, EGFR1, and HER2, which are particularly important for the growth of breast cancer 136. Recently SFN was shown to cause DNA damage through enhanced acetylation of DNA repair proteins. This effect was shown to be specific for cancer cells as there were no epigenetic changes or DNA damage observed in noncancer cells 137. Interestingly, based on the methylation of DNA and cyclin D2 by SFN, a clinical trial (NCT01265953) has also been initiated at Portland, VA Medical Center 138. Studies suggest significant epigenetic changes induced by SFN in various cancer models.
4.3.2 Angiogenesis
Very few studies have reported the antiangiogenic effects of SFN. The suppression of VEGF and MMP-2 has been shown by SFN treatment 139, 140. Another study indicated that VEGF suppression was mediated through inhibition of FOXO1/AKT pathway 141. However, no further evidence exists for the antiangiogenic effects of SFN. Due to the lack of sufficient evidence, antiangiogenic activity cannot be considered as a critical mechanism of SFN.
4.3.3 Mitochondrial cell death
Another important mechanism of action of SFN was inactivation of inhibitors of apoptosis proteins 142. SFN-mediated inhibitors of apoptosis protein inhibition was associated with BCL-2 inhibition, suggesting activation of intrinsic apoptosis pathway 143. SFN also causes generation of mitochondrial ROS in cancer cells that further leads to release of cytochrome c into cytosol augmenting cell apoptosis 144. Interestingly, an ROS independent activation of MEK/ERK pathway was shown to lead to caspase-dependent apoptosis in neuroblastoma cells 145.
4.3.4 Cell-cycle arrest
SFN was shown to induce p27-mediated G0/G1 phase cell-cycle arrest 146. In addition, SFN causes irreversible cell-cycle arrest in G2/M phase followed by caspase-mediated apoptosis 147. Recent studies have shown that SFN induces G2/M arrest through the activation of p21 (CIP1/WAF1) and inhibition of Cdc2/Cyclin B1 complex independent of p53 148. This study showed that apoptosis following G2/M arrest was induced by caspase and PARP activation in leukemia cells 148. Specific activation of MAP kinases, such as ERK, JNK, and p38, in response to SFN treatment was shown to be involved in inducing cell-cycle arrest 149, 150.
4.3.5 Invasion and metastasis
SFN exhibits potent antimetastatic effects by suppressing cell migration and invasion. Jee et al. observed that the anticell migratory effect of SFN was associated with MMP suppression 151. Recently epithelial to mesenchymal transition (EMT) was shown to be an important mechanism of SFN to inhibit cell migration and metastasis in different cancer types 143, 151-153. Li et al. have shown that SFN modulates Sonic hedgehog pathway to suppress self-renewal capacity of the pancreatic cancer stem cells and reduce EMT characteristics 143. Significant suppression of SNAIL and ZEB-1 marked by the reexpression of E-cadherin was observed by SFN treatment that lead to reversal of EMT 153. EMT prevention by SFN was also associated with induction of miR-200c and reexpression of the estrogen receptor 154. The details of molecular targets of SFN have been described in Table 1.
4.3.6 In vivo studies
Kanematsu et al. demonstrated the in vivo efficacy of SFN against tumor growth and metastasis in breast cancer 152. Pharmacokinetic studies show good bioavailability of SFN after oral administration. A concentration of 20 μM in plasma was achieved after oral administration of 50 μmol SFN/rat (35 mg/kg) 155. In a human study it was shown that after consumption of 200 μmol SFN (35.5 mg), about 2 pmol/mg (0.355 ng/mg) SFN was detected in the breast tissue, suggesting its availability at the tumor site 156. The cumulative concentration of SFN in the small intestine was shown to be sufficient to inhibit tumor growth in the colonic tissue 157. These studies clearly indicate bioavailability and favorable pharmacokinetic profile of SFN that can be instrumental for future development of SFN as an anticancer agent.
4.3.7 Toxicity studies
Along with the anticancer activity of SFN, it is important to study its toxicity to assess to benefit to risk ratio. An increase in hepatoxicity indicators aspartate aminotransferase (AST), alanine aminotransferase (ALT), and lactate dehydrogenase (LDH) in plasma was observed with SFN (1.6 mg/mouse/day [64 mg/kg] for 14 wk) administration in mouse bearing benzo(a)pyrene-induced (B(a)P; 100 mg/kg b.wt.) lung cancer 158. Interestingly, opposite findings were reported in another study. The rats were pretreated with 3 mg/kg SFN by intraperitoneal injection. One hour later an intestinal ischemia/reperfusion surgery was performed to induce toxicity. It was observed that SFN administration increased the SOD levels along with reduction of myeloperoxidase, ALT, and AST levels in serum 159. Both the studies used significantly different concentrations of SFN, which can explain the opposite observations. However, due to the lack of confirmatory evidence, overall no conclusion can be drawn about the toxicity of SFN.
4.4 Allyl isothiocyanate (AITC)
AITC is an aliphatic isothiocyanate derived from sinigrin and is excreted as NAC conjugates in the urine 160. A recent study demonstrated a short-term reversible DNA damage when AITC was provided in the diet 161. Cancer cells in general are more susceptible to DNA damage leading to cell death. This explains the enhanced sensitivity of cancer cells toward AITC. The cytotoxic effects of AITC were shown to be specific to cancer cells (Fig. 3) 162. Smith et al. demonstrated apoptosis induction by AITC in colorectal cancer cells 163.
4.4.1 Cell Proliferation and growth
AITC targets specific signaling molecules to suppress cancer cell growth. ERK and JNK signaling were involved in the activation of AP-1 by AITC to suppress cancer cell growth 164, 165.
4.4.2 Mitochondrial cell death
Geng et al. observed that AITC resulted in the phosphorylation of BCL-2 to induce apoptosis, whereas mutated BCL-2 abrogated the cytotoxic effects of AITC 166.
4.4.3 Cell-cycle arrest
Srivastava et al. demonstrated the in vivo efficacy of AITC in prostate cancer 167. This study indicated that cell growth arrest in G2/M phase by AITC was associated with the inhibition of cyclin B1, cell division cycle (Cdc)25B and Cdc25C.
4.4.4 Invasion and metastasis
The antimetastatic effects of AITC have been demonstrated through suppression of cell migration and invasion. It was observed that AITC inhibits MMP2/9 to exhibit antimetastatic effects in hepatoma cells 168. Furthermore, AITC exerts antiangiogenic effects to suppress tumor growth by downregulating angiogenic factors, such as nitric oxide and tumor necrosis factor α (TNF-α; Table 1).
4.4.5 In vivo studies
AITC was shown to inhibit tumor and ascites formation from Ehrlich ascites tumor cells in mice. This study also revealed enhanced survival of ascites-bearing mice with AITC treatment 169. Furthermore, i.p. administration of 25 μg AITC/animal (1 mg/kg) in mice inhibited tumor-directed capillary formation, suggesting inhibition of angiogenesis. AITC treatment also reduced serum nitric oxide and TNF-α levels indicating reduction in inflammatory markers by AITC 170. These studies suggest a good in vivo efficacy of AITC. Nonetheless, more studies are required to confirm the in vivo activity against contemporary targets in cancer.
4.4.6 Toxicity studies
Preclinical studies have demonstrated some toxicity induced by AITC. Significant hematological changes were observed with AITC treatment. Subcutaneous administration of 20 mg/kg AITC reduced WBC counts by 25% along with marked reduction of lymphocytes and monocytes. In addition, increase in neutrophil and corticosteroid levels were observed, indicating stress induced by AITC. The AITC treatment caused reduction in thymus weights while increasing the weights of adrenals 171. These observations suggest significant effect of AITC on blood profile and organ weights. Interestingly in another study, i.p. administration of 25 μg AITC/animal every day for five consecutive days showed reduced WBC count at the 9th day after starting the treatment 172. Perhaps the differences between these observations could be due to different doses and the time points of analysis after AITC administration. Another study showed increased AST levels at high doses of AITC (100–150 mg/kg), but no change was observed at lower dose (50 mg/kg), suggesting dose-dependent toxicity induced by AITC 173. Interestingly, oral administration of AITC resulted in bladder toxicity in rats. This was found due to free AITC cleaved from urinary metabolites 174. Taken together, studies suggest that AITC exhibits toxic side effects, cautioning its use. Further in-depth studies are required to establish the toxicity profile of AITC so that the dose for anticancer effects can be titrated effectively.
5 Potential for combination therapy
Cancer cells contain multiple aberrant signaling pathways that lead to drug resistance and therapy failure in many patients. Combination therapy is known to kill cancer cells more effectively through diverse mechanisms simultaneously. ITCs exhibit a diverse range of cellular targets for anticancer effect. This property of ITCs makes them highly desirable for combinatorial therapeutic approaches. Several combination strategies have been tested in preclinical studies by combining ITCs among themselves or with conventional or new anticancer therapies (Table 2) 58, 175-182.
| ITCs | Concentrations and treatment time of ITCs | Combination with other agents | Concentrations | Cancer type | Targets affected by combination treatment | Effect of combined treatment | References |
|---|---|---|---|---|---|---|---|
| BITC | 5 μM (18 h) | TRAIL | 10 ng/mL (6 h) | Pancreatic | ↑Caspase cleavage, ↓XIAP, ↑ BID cleavage, ↑ PARP cleavage | Synergistic | 192 |
| 20 μM (1 h) | Cisplatin | 15, 30, 45 μM (48 h) | Lung | ↓ β-Tubulin | Sensitization | 193 | |
| 10 μM (3 days) | SFN | 10 μM (3 days) | Pancreatic | ↓ STAT3 | Synergistic | 202 | |
| 9, 12 μmol (10 wk) | PEITC (10 wk) | 12 μmol | Lung | ↓ Chemically induced tumorigenesis | Synergistic | 203 | |
| 2.5 μM (24 h) | Radiation | 5 Gy (24–48 h) | Pancreatic | ↑ Caspase cleavage, ↑ G2/M cell-cycle arrest, ↑ ATR, ↑ Chk2, ↑ Cdc25c, ↑ Cdk-1, ↑ p21Waf1/Cip1 | Synergistic | 58 | |
| PEITC | 5, 10 μM (8, 24 h) | Cisplatin | 5, 10 μM (8, 24 h) | Cervical | ↑ ERK, ↑ JNK, ↑ p38, ↑ MAPK | Synergistic | 181 |
| 20 μM (1 h) | Cisplatin | 15, 30, 45 μM (48 h) | Lung | ↓ β-Tubulin | Sensitization | 193 | |
| 0.1, 0.5, 2.5, 5 μM (24 h) | Adriamycin | 20, 25 μM (24 h) | Cervical | ↓ PKC, ↓ telomerase |
Synergistic | 195 | |
| 0.1, 0.5, 2.5, 5 μM (24 h) | Etoposide | 20, 25 μM (24 h) | Cervical | ↓ PKC, ↓ telomerase |
Synergistic | 195 | |
| 5 μM (48 h) | Paclitaxel | 10 nM (48 h) | Breast | ↑ G2/M cell-cycle arrest | Synergistic | 196 | |
| 5 μM (24 h), 25 mg/kg (50 days) | Platinum agents | 40 μM (24 h), 5 mg/kg (50 days) | Lung | ↓ GSH-mediated export, ↑ ROS, ↑ DNA damage | Sensitization | 177 | |
| 5 μM (24 h) | Metformin | 8 mM (24 h) | Ovarian (cisplatin resistant) | ↑ ROS | Synergistic | 178 | |
| 2.5 μM (6 h) | Vorinostat | 2 μM (18 h) | Leukemia | ↑ ROS | Synergistic | 179 | |
| 2 μM (24 h) | Docetaxel | 1nM (24 h) | Prostate | ↑ XIAP, ↓ BCL-2 | Synergistic | 97 | |
| 0.025% in diet (10 and 16 wk) | Curcumin | 1% in diet (10 and 16 wk) | Prostate | ↓ PDK-1/AKT | Synergistic | 208 | |
| 2.5 μmol (28 days) | Curcumin | 3 μmol (28 days) | Prostate | ↓ AKT | Synergistic | 209 | |
| 10 μM (24 h) | Curcumin | 25 μM (24 h) | Prostate | ↓ EGFR, ↓ AKT, ↓ NF-κB | Synergistic | 210 | |
| 2 μM (24 h) | SFN | 0.4 μM (24 h) | Leukemia | ↓ iNOS, ↓ COX-2, ↓ prostaglandin E2, ↓ tumor necrosis factor (TNF), ↓ IL-1 | Synergistic | 206 | |
| 0.008% in diet (17 wk) | d-Limonene, indole-3 carbinol | 0.63%, 0.18% in diet (17 wk) | Lung | ↓ Chemically induced tumorigenesis | Synergistic | 183 | |
| SFN | 20 μM (24, 48 h) | Radiation | 2 Gy (24, 48 h) | Osteosarcoma | ↑ Caspase cleavage, ↓ ERK, ↓ AKT, ↓ G2/M cell-cycle arrest | Synergistic | 176 |
| 10 μM (0, 12, 24, 48, 72 h) | Radiation | 4 Gy (0, 12, 24, 48, 72 h) | Head and neck cancer | ↓ AKT, ↓ MCL-1 | Synergistic | 184 | |
| 3 μM (24 h) | Arsenic trioxide | 1 μM (24 h) | Multiple myeloma | ↑ ER stress, ↑ HSP90, ↑ PERK, ↑ eIF2α, ↑ unfolded protein response, ↑ ROS | Synergistic | 185 | |
| 20–30 μM (16 h) | 5-FU | 45–60 μM (16 h) | Salivary gland adenoid cystic carcinoma | ↓ NF-κB | Synergistic | 182 | |
| 25 μM (24 h) | Adriamycin | 0.6–10 μM (24 h) | Adriamycin resistant mouse fibroblasts with mutant p53 | ↑p53 | Sensitization | 194 | |
| 1–20 μM (6, 24 h) | Oxaliplatin | 100 nM–10 μM (6, 24 h) | Colorectal cancer | ↑ DNA fragmentation | Synergistic | 197 | |
10 μM (72 h) 3 mg/kg (3 days) |
Sorafenib | 20 μM (48 h) 60 mg/kg (3 days) |
Pancreatic cancer stem cells | ↓ ALDH1, ↓ NF-κB | Synergistic | 180 | |
| 25 μM (24 h) | Resveratrol | 25 μM (24 h) | Glioma cells | ↓ LDH, ↓ AKT, ↑ caspase-3 cleavage | Synergistic | 186 | |
| 20 μM (48, 72 h) | Diindolylmethane | 20 μM (48, 72 h) | Colon | ↑ G2/M cell-cycle arrest | Antagonistic (at low concentrations) Synergistic (at higher concentrations) |
201 | |
| Quercetin | Pancreatic cancer stem cells | ↓ BCL-2, ↓ XIAP, ↑ caspase 3 cleavage | Synergistic | 187 | |||
| 10, 20 μM (16 h) | Quercetin | 25, 50 μM (16 h) | Melanoma | ↓ MMP-9 | Synergistic | 188 | |
| 10 μM (6 days) | EGG | 20 μM (6 days) | Ovarian | ↓ hTERT, ↓ BCL-2 | Synergistic | 213 | |
25 μM (24 h) 45 mg/kg (3, 12 h) |
EGG | 20, 100 μM (24 h) 100 mg/kg (3, 12 h) |
Prostate | ↓ Nrf2, ↓ AP-1 | Synergistic | 212 |
- ER, estrogen receptor; MAPK, mitogen-activated protein kinase.
Radiation therapy is an important intervention for majority of cancers. Radiation has been shown to activate some important cancer cell survival signaling molecules, such as AKT, ERK, and MCL-1 that lead to reduced efficacy. Our studies have shown that when BITC was combined with radiation therapy, a 2.8-fold increase in apoptosis and cleavage of caspase-3 was achieved in pancreatic cancer cells 58. In addition to increased apoptosis, inhibition of NF-κB and activation of p38 was also observed with the combination of BITC and radiation therapy 58. The combination of BITC or SFN with the radiation therapy caused increased G2/M cell-cycle arrest 58, 175. Combination of SFN with radiation therapy also showed inhibition of activation of critical molecules, such as AKT, ERK, and MCL-1, along with induction of ER stress, explaining its efficacy 175, 183-187.
TNF-related apoptosis-inducing ligand (TRAIL) is a potential chemotherapeutic agent. Interestingly, TRAIL death receptors are highly expressed on cancer cells but not on normal cells making the cancer cells more susceptible to TRAIL-induced apoptosis as compared to normal cells 188, 189. However, resistance to TRAIL is reported in many cancer cells 189, 190. Our studies showed that BITC sensitized pancreatic cancer cells to TRAIL-induced apoptosis by activating both intrinsic and extrinsic pathway 191.
Accumulating evidence shows that combination of ITCs with conventional chemotherapeutics improves the efficacy against resistant cancer cells. Studies suggest synergistic activity of ITCs with common anticancer agents, such as cisplatin, adriamycin, etoposide, paclitaxel, metformin, vorinostat, and docetaxel 176, 181, 192-194. Both BITC and PEITC increased the apoptotic effects of cisplatin through depletion of β-tubulin, but the combination did not affect DNA platination 180, 192. Furthermore, reversal of the resistance to cisplatin was observed with PEITC, which was mediated by depletion of cellular GSH 176. The combination of metformin and PEITC also showed high efficacy in cisplatin resistant cancer cells 177. PEITC and SFN caused inhibition of antiapoptotic proteins, such as protein kinase C (α, β, ε, and ς), and telomerase, while increasing proapoptotic protein kinase Cб to enhance the apoptosis caused by adriamycin and etoposide 194. Also, the combination of adriamycin with SFN induced sensitivity in resistant cancer cells by the effect of adriamycin independent of p53 193. An HDAC inhibitor, vorinostat, induced ROS to increase resistance in cancer cells. PEITC treatment suppressed the cytoprotective antioxidant response through depletion of cellular ROS to reverse the resistance in leukemia cells 178. The efficacy of taxanes was also enhanced by PEITC in different forms of cancer 97, 195. The combination of SFN with oxaliplatin caused increased DNA fragmentation, suggesting synergism through oxaliplatin dependent mechanism 196. NF-κB is a known target of SFN 197. NF-κB inhibition by SFN mediated synergism with sorafenib and 5-fluorouracil to inhibit pancreatic cancer stem cell survival and salivary gland adenoid cystic carcinoma, respectively 179, 181. These observations suggest that ITCs can utilize the mechanisms of action of conventional agents or can induce independent effects to exhibit synergism.
Although most of the combinations exhibited synergistic effects in cancer cells, a combination of 5-fluorouracil with SFN showed antagonistic activity in the normal cells by modulating G2/M cell-cycle phase 198. This suggests that ITCs protect normal cells from the toxic effects of conventional therapeutic agents. Another study showed that the combination of cisplatin with ITCs was selectively effective in cancer cells 180. Although the mechanism of selectivity remains to be elucidated, these observations clearly suggest an urgent need for clinical testing of the combination therapies of ITCs with conventional anticancer chemotherapeutics.
ITCs have been shown to offer synergism among themselves and other anticancer compounds. 3,3′-diindolylmethane is an important constituent of cruciferous vegetables and exhibits anticancer effects 199. 3,3′-diindolylmethane synergizes with SFN leading to enhanced cell-cycle arrest in colon cancer cells 200. Among other ITCs, combination of BITC with SFN or PEITC was more effective in preventing pancreatic and lung cancer than the individual treatment 201, 202. Curcumin is a well-known dietary agent with remarkable anticancer activity 203, 204. The combination of curcumin with ITCs caused significant reduction in the levels of inflammatory markers. These observations advocate the possible synergistic or additive effect of curcumin in combination with ITCs 205, 206. Several other studies reenforce the enhanced anticancer effect of PEITC with curcumin through inhibition of prosurvival pathways, such AKT, EGFR, and NF-κB 207-209. Epigallocatechin gallate (EGG), a green tea agent, has significant anticancer potential 210. The chemopreventive effects of the combination of SFN with EGG were successfully shown in transgenic model of prostate cancer through the induction of Nrf2 and AP-1 in Nrf2-deficient mice 211. Furthermore, the combined treatment of SFN with EGG enhanced apoptosis in paclitaxel-resistant cancer cells by inhibiting hTERT and BCL-2 expression, showing therapeutic anticancer potential 212. Taken together, it is clear from the above the studies that ITCs can be used for combination therapeutics in cancer treatment, especially for the resistant cancers. The combinations of ITCs with various anticancer agents and their prime mechanism of action have been summarized in Table 2.
6 Conclusion
Current epidemiological studies have certain limitations, such as differential exposure of the populations leading to misclassification, improper controls, and possibility of recall bias. Hence, better designed studies are required to establish the role of ITCs as neutraceuticals for cancer prevention and treatment. Furthermore, better designed studies along with detailed mechanistic studies can provide us with an opportunity to use ITCs as the lead for synthesis of more potent and safe drugs through chemical modifications. It is important to note that some studies were done using extracts of ITCs from the vegetables. Few studies have shown that ITCs are susceptible to hydrolytic degradation at high temperatures and basic conditions 213, 214. Thus, the observations made by extracts of ITCs could be questionable especially if the extraction procedure was not appropriate or standard. These observations require further confirmation using pure forms of ITCs.
Recent studies have revealed many novel cancer targets. Specifically, targeting these can enhance the efficacy of new as well as conventional therapies. Hence, it is important to test the efficacy of ITCs against new targets. Current preclinical evidence presented in the review provides an insight into potential anticancer mechanisms of action of the ITCs as well as their selectivity toward the cancer cells. Some clinical studies have been initiated already for some ITCs. Nonetheless, further detailed studies are required to establish the safety and efficacy profiles of these agents based on which they can be streamlined for further human studies. Based on the current data, it is evident that ITCs possess highly potential anticancer activity, but further detailed toxicity and clinical studies are required to warrant their future clinical benefits.
It should be noted that although we tried to include most of the published papers related to the objective of this review, it is possible that by mistake we may have missed a few papers. For this we would like to apologize to those authors.
In order to maintain consistency, we converted all the doses of ITCs into metric units, which initially appeared in different forms in the literature. The conversion was made assuming the average weight of mice as 25 g and average weight of rats as 250 g. We would like to apologize for any deviation that might have occurred during unit conversion from the dose used in the actual study. We therefore included the units reported by the authors as well as values converted into metric units by us in parenthesis.
Acknowledgments
Sanjay K. Srivastava is currently an International Scholar at Kyung Hee University, Seoul, South Korea. This work was supported in part by R01 grants CA106953 and CA129038 (to S. K. S.) awarded by National Cancer Institute, NIH, and MRC grant 2007–0054931 (to S. H. K.). Critical reading of the manuscript by Shari Morris is greatly appreciated.
The authors have declared no conflict of interest.