Cochlear implantation under local anesthetic: A systematic review and meta-analysis
Abstract
Objectives
As the population ages and implantation criteria are relaxed, more patients with complex comorbidities are becoming eligible for cochlear implantation (CI). These patients have higher risks associated with general anesthesia. This systematic review assesses outcomes and complications following CI under local anesthetic to examine utility for patients deemed not suitable or at high risk for general anesthesia.
Methods
A systematic review and meta-analysis performed according to the 2020 PRISMA guidelines. Databases searched were MEDLINE, PubMed, EMBASE, CINAHL, Web of Science Core Collection, Cochrane Database of Systematic Reviews, and Cochrane Central Register of Controlled Trials and ClinicalTrials.gov. There were no limitations on year of publication or language.
Results
Then, 132 unique were identified. After screening abstracts and full texts for eligibility criteria a total of 18 articles were included. In the nine studies where audiological data were reported, all patients demonstrated improvement in audiological outcomes following implantation under local anesthetic (LA). Only minor complications of transient vertigo, wound infection, facial nerve paralysis, confusion, and tinnitus were reported but all were transient. Meta-analysis showed surgical time was significantly shorter under LA.
Conclusions
CI under LA is safe for patients with comorbidities which preclude them from general anesthesia, with minimal complications and an improved cost-effectiveness profile. However, larger scale, robust trials are required to assess this further.
1 INTRODUCTION
The World Health Organization predict that by 2050, nearly 2.5 billion people are projected to have some degree of hearing loss, with 700 million requiring some form of hearing rehabilitation. Currently, 5% of the world's population (430 million people) require rehabilitation as a result of disabling hearing loss greater than 35 decibels (dB).1 In the United States alone, approximately 150,000 patients meet the criteria for cochlear implantation. This number is only expected to rise further due to an aging population mirrored across the world.2
Aging increases the risks associated with general anesthesia due to a decreased physiological reserve and from preexisting cerebrovascular, cardiac, and/or pulmonary disease which increases their risk of perioperative morbidity and mortality. Elderly adults have been shown to be at increased risk of postoperative cognitive deficit after general anesthetic (GA) and delirium, which has been shown as an independent risk factor for increased mortality and leads to an increased decline in postoperative physical and social functioning.3, 4 However, untreated hearing loss has been shown to be one of the most significant reversible factors for dementia.5, 6 Cochlear implants have been shown to have significant auditory rehabilitation benefit. Benefits extend to those with comorbidities, including those aged 70 years over.7 This has led to surgeons exploring the possibility of cochlear implantation under local anesthetic (LA).
Another independent consideration is that local anesthetic may increase patient satisfaction by allowing them to feel in control, to raise awareness of pain and to remain grounded to their surroundings. Conversely, the often-alien environment of an operating theater may startle patients and lead to increased emotional trauma.8 There are cost implications too, with procedures under local often requiring less monitoring, less equipment, and a shorter hospital stay postoperatively.9
Cochlear implantation under local anesthetic as a viable alternative to general anesthesia and has been described by several centers. It is a technique used with increasing frequency in comorbid patients for whom general anesthesia poses too high a risk. It has been shown to decrease length of hospital stay and reduce morbidity associated with surgery under general anesthesia.10
The aim of this systematic review was to identify and synthesize documented cases of cochlear implantation under LA, and to assess preoperative and postoperative hearing outcomes and quality of life changes. We also aimed to evaluate surgical techniques, postoperative adverse outcomes and compare hospital stays between local and GA groups.
Population: Children or adults undergoing cochlear implantation under LA.
Intervention: Cochlear implantation under LA.
Comparison: Cochlear implantation under GA or other surgical technique.
Outcomes: Preoperative and postoperative hearing outcomes, quality of life changes, surgical techniques, postoperative adverse outcomes, and compare postoperative hospital stays.
2 MATERIALS AND METHODS
2.1 Study registration
This study was registered on the PROSPERO database of systematic reviews (reference number CRD42021251617). The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed.11
2.2 Inclusion criteria
Studies for inclusion were clinical studies of cochlear implantation under LA where audiological, surgical, postoperative, or quality of life outcomes at any postoperative time were reported. Studies included were experiential or observational of human subjects. Animal or laboratory studies were excluded, as were studies focusing on surgical techniques with no human subjects.
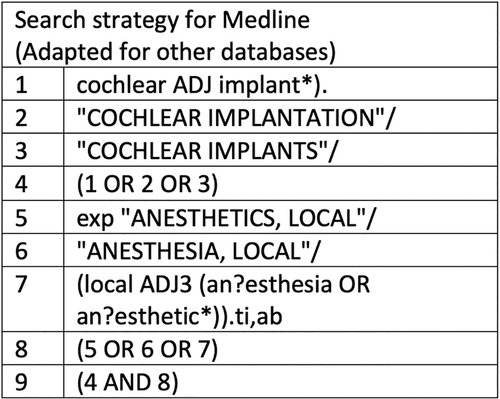
2.3 Study search strategy
BW performed the comprehensive searches using the search terms for MEDLINE as shown in Figure 1. Search terms were adapted for PubMed, CINAHL, and EMBASE. Searches for these databases were conducted using the National Institute for Health and Care Excellence Healthcare Databases Advanced Search (Health Education England). Web of Science Core Collection, the Cochrane Database of Systematic Reviews and Cochrane Central Register of Controlled Trial, and ClinicalTrials.gov were searched individually and exact search terminology for each database can be found in Appendix. There were no restrictions on language or date. These searches were rechecked by a clinical effectiveness librarian to ensure complete coverage of all available literature.
2.4 Study selection
Two reviewers (BW/PG) independently screened titles and abstracts. Full texts of studies potentially meeting the inclusion criteria were then reviewed by BW/PG to assess eligibility for inclusion. Where a full text could not be found, authors were contacted directly via email, if they remained unavailable, the study was excluded. Conflicts between reviewers were resolved by discussion. Reference lists of screened full texts were examined and reviewed for potential additional studies which met the inclusion criteria. The primary outcome measures were surgical technique, postoperative complications audiological outcomes. Secondary outcome measures were quality of life, comorbidities precluding GA, postoperative inpatient stay, and preoperative measures to aid postoperative recovery.
2.5 Data extraction
Data were independently extracted and checked by both BW and PG using a predetermined spreadsheet (Microsoft Excel).
2.6 Risk of bias analysis
Risk of bias of selected studies was completed using the Brazelli risk of bias tool12 for nonrandomized studies and the Oxford Centre for Evidence-Based Medicine (OCEBM) grading system.13 Biases were independently assessed and compared by both BW and PG using a spreadsheet (Microsoft Excel), with conflicts resolved by discussion. Where conflicts arose which could not be resolved by discussion, a senior reviewer (J. M.) provided a final decision.
3 RESULTS
3.1 Search results
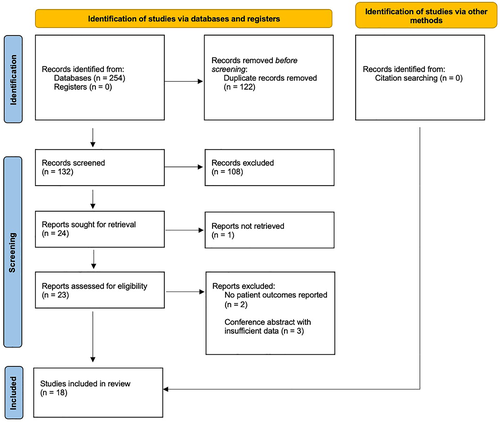
Searches were performed on April 25, 2021 and results of screening are shown in Figure 2. The initial search identified 254 studies. After removing duplicates, 132 full titles and abstracts were screened, of which 24 articles were shortlisted for full-text review. Six articles did not meet the inclusion criteria and were therefore excluded, leaving 18 articles for qualitative analysis. The heterogenicity of study design and outcome reporting precluded a quantitative analysis for outcomes other than operative time.
3.2 Characteristics of included studies
Study characteristics are displayed in Table 1. Included studies consisted of eight case series, five case controls and five case reports from 1998 to 2021. There were a total of 450 participants, of which 262 (58%) received cochlear implants under LA and 188 (42%) received cochlear implantation under GA. From available demographic data, there were 241 males and 209 females (with a male predominance of 1:1.5). The average age of implantation under LA was 59.9 years (range: 13–93). A single study reviewed cochlear implantation in children, others compared outcomes between adults. The implant models used were: Med-El (Synchrony, Flex 28, Concerto, Sonata, Form 24); Advanced Bionics (HiFocus 1J, HiFocus Mid-Scala); and Cochlear (CI532, Freedom Contour Advance, Freedom, N512, CI632, N22, CI422, CI24M, Contour advance CI24RE, Nucleus CI522). Full electrode insertion was achieved by the majority of authors, with only three implants by two authors experiencing partial electrode implantation.14, 15
| Authors | Year | Country | Study type | Number of patients | Population | OCEBM grade |
|---|---|---|---|---|---|---|
| Abrar et al.14 | 2020 | United Kingdom | Case report | 1 | Adults | V |
| Alzahrani et al.20 | 2014 | France | Case report | 1 | Adult | V |
| Connors et al.28 | 2020 | United States | Case control | 150 | Adults | IV |
| Dietz et al.21 | 2016 | Finland | Case series | 7 | Adults | IV |
| Djalilian et al.22 | 2005 | United States | Case report | 1 | Adult | V |
| Hamerschmidt et al.10 | 2012 | Brazil | Case control | 40 | Adults | IV |
| Hamerschmidt et al.26 | 2010 | Brazil | Case series | 3 | Adults | IV |
| Kecskemeti et al.27 | 2018 | Hungary | Case series | 4 | Adults | IV |
| Mistry et al.16 | 2017 | United Kingdom | Case series | 7 | Adults | IV |
| Pateron et al.15 | 2015 | France | Case control | 61 | Adults | IV |
| de Oliveira et al.36 | 2012 | Brazil | Case report | 1 | Children | V |
| Shabashev et al.23 | 2017 | United States | Case control | 40 | Adults | IV |
| Spitzer and Waltzman30 | 2021 | United States | Case series | 76 | Adults | IV |
| Svrakic et al.18 | 2014 | United States | Case control | 17 | Adults | IV |
| Toner et al.17 | 2013 | United Kingdom | Case series | 16 | Adults | IV |
| Toner et al.24 | 1998 | United Kingdom | Case series | 4 | Adults | IV |
| Vaid et al.25 | 2016 | India | Case report | 1 | Adults | V |
| Vincenti et al.29 | 2020 | Italy | Case series | 20 | Adults | IV |
3.3 Comorbidity grading
A total of 242 participants across seven articles had an American Society of Anesthesiologists (ASA) Physical Status grade identified. Of 161 with reported ASA grades who received cochlear implantation under LA, the majority were ASA II (n = 82) and III (n = 64), followed by ASA IV (n = 9) and I (n = 6). Of the 81 receiving cochlear implantation under GA with an identified ASA grade, none were ASA IV, and the majority were ASA II (n = 48) and III (n = 31), with ASA I accounting for only two participants. In cases where a range of ASA grading was reported, the lowest ASA grading was taken.
Four studies (n = 43 participants)14, 16-18 used the Portsmouth Physiological and Operative Severity Score for the enumeration of Mortality and morbidity (P-POSSUM) scoring tool, a tool which was developed by Copeland et al.19 which predicts mortality in patients undergoing different types of surgery. A combined 32 participants in the LA groups of these studies had an average predicted morbidity of 46.38% (10.2–93.6%) and average predicted mortality of 6.76% (0.4–36%), compared with 39.16% (18.5–70.3) and 2.94% (0.8–7.1%) of 11 participants who underwent CI under general anesthesia (GA), respectively. A single case report utilizing the surgical outcome risk tool calculated their patient's predicted risk of 1%, with a frailty score of four.14
3.4 Audiological outcomes
Audiological outcomes were reported in nine studies (113 patients) and are presented in Table 2. Overall, there was a trend toward benefit from cochlear implantation under LA.
| Study | Preoperative data | Postoperative data | Follow-up |
|---|---|---|---|
| Abrar et al. (2020)14 | Wearing bilateral hearing aids since aged 27. Audiology—Acoustic reflexes and transient otoacoustic emissions were absent bilaterally. PTA—Profound hearing loss. Speech discrimination—Unable to identify a single keyword from BKB sentences presented at 70 dB hearing loss in quiet, whilst wearing bilateral hearing aids. Otology—Unremarkable. Tympanometry—Bilateral middle ear function was normal. |
A three-month audiological assessment showed a significant improvement in audiometry assessments. Speech discrimination—The patient was able to identify 100% of BKB sentences presented in quiet and 88% in noise. The patient could identify 82% of AB word lists with bilateral implants (53% with left, 65% with right). Aided free field audiogram results using warble tones with bilateral implants switch on—Right ear—250 Hz: 30, 500 Hz: 35 1 kHz: 35, 2 kHz: 30, 4kHz: 40, 8 kHz: 35. Left ear—250 Hz: 35, 500 Hz: 30 1 kHz: 35, 2 kHz: 30, 4kHz: 35, 8 kHz: 35. |
4 months |
| Alzahrani et al. (2014)20 | Severe bilateral sensorineural hearing loss, 90 dB hearing loss and 20% speech discrimination at 60 dB under best aided conditions with mono-syllabic roads. | Not reported | 3 weeks |
| Dietz et al. (2016)21 | Speech reception at 65 dB—21, 0, 56, 52, 0, 0, and 60%, respectively. | Speech reception at 65 dB—100, 98, 89, 92, 85, 94, and 76%, respectively. | 2–4 weeks |
| Djalilian et al. (2005)22 | Audiology—Severe sensorineural hearing loss on the right and profound deafness on the left. Hearing in noise testing under best aided condition showed word recognition (NU-6) on the right ear was 24%, this could not be tested on the left due to profound deafness. Aided thresholds were mild-moderately severe with a 52% score on CID sentences. The left ear was unresponsive even with a hearing aid. |
PTA of 20 dB. | 16 months |
| Spitzer and Waltzman (2021)30 | Preoperative group PTA was 94.94 dB hearing loss. | Average speech perception for words in quiet improved by 37% (preop: 9.24%, 1 year: 46.18%). Scores for sentences in quiet improved by 45% (13.0–58.13% at 1 year). Scores for sentences in noise improved by 28% (8.85–36.54%). CNC scores at 3 months, 1, 2 and 3 years post-activation were significantly better than preoperative scores (3 months: t(60.0) = 9.64, p < .001; 1 year: t(54.2) = 10.56, p < .001; 2 years: t(30.1) = 11.18, p < .001; 3 years: t(10) = 5.85, p < .001). Post hoc pairwise comparisons found a significant improvement in scores from 3 months to 1 year. No difference was detected between scores at 1 and 2 years or between 2 and 3 years. For AzBio sentences, scores at 3 months, 1 and 2 years were significantly better than preoperative scores (3 months: t(47.4) = 7.56, p < .001; 1 year: t(27.4) = 8.05, p < .001; 2 years: t(11.6) = 6.18, p < .001). There was no significant improvement in scores between 3 months and 1 year or between 1 and 2 years. For AzBio sentences in +10 dB scores at 3 months, 1 and 2 years were all significantly better than preoperative scores. There was no significant improvement in scores between 3 months and 1 year or between 1 and 2 years. HINT scores at 3 months and year postoperatively were significantly better (3 months: t(10.13) = 6.24, p < .001; 1 year: t(11.22) = 9.35, p < .001). Post hoc analyses showed no significant improvement between 3 months and 1 year. |
3 years |
| Toner et al. (1998)24 | Not reported. | Aided free fluid audiogram 45–50, 40–45, 40–50, and 40 dB postoperatively. | Not reported |
| Toner et al. (2013)17 | Not reported. | The average postoperative BKB sentence score was 72%. | Not reported. Average length of use of implant was 5 years 6 months. |
| Vaid et al. (2016)25 | First audiogram—Bilateral moderate to severe sensorineural hearing loss with a PTA of 80 dB hearing loss in right ear and 78 dB hearing loss in the left ear. Second audiogram 2–7 months later—Bilateral profound sensorineural hearing loss with PTA of 103 dB hearing loss. Aided audiogram showed thresholds below the speech spectrum with a PTA of 88 dB hearing loss in right and 81 dB hearing loss in the left ear. CAP score was level 1. Listening process profile was 02/42 and telephone profile test was 00/32. |
Aided thresholds of 33 dB hearing loss on right and 75 dB hearing loss on left. Word recognition score was 66%. CAP score was level 7. Listening process profile was 42/42 and telephone profile was 26/32. |
3 months |
- Abbreviations: AB, Arthur Boothroyd Isophonemic Monosyllabic Word Test; Azbio, Arizona State University Sentences; BKB, Bamford, Kowal and Bench; CAP, Categories of Auditory Perception Score; CID, Central Institute for the Deaf; CNC, Consonant Nucleus Consonant Scores; Db, decibels; HINT, Hearing in Noise Sentence Test; PTA, Pure Tone Audiometry.
Preoperative data were available for seven studies, of which every patient demonstrated severe to profound sensorineural hearing loss through different audiological outcome measures. Pure tone average (PTA) was the most used (n = 6) method of assessing audiological function. Speech discrimination was assessed in seven studies, with Bamford–Kowal–Bench (BKB) sentences and Arizona State University (AzBio) sentences commonly used, in two instances best-aided conditions were used. Otoacoustic emission, Hearing In Noise Test (HINT) scoring, Categories of Auditory Performance (CAP) scoring, listening progress profiles and telephone profile testing were each utilized preoperatively once.
Of the eight studies where postoperative audiological function testing is recorded, only six compare these with preoperative results. Of these six articles, all patients with implants implanted under LA showed improvement from preoperative audiological function testing. Similar to preoperative testing, multiple heterogenous methodologies were employed to assess audiological function postoperatively, as identified in Table 2.
3.5 Surgical techniques and outcomes
Surgical incision and approach was reported in 14 studies, a post auricular (standard) approach was used in 12 studies,10, 14-16, 18, 20-26 with a posterior suprameatal approach used in two further studies.21, 27 Facial nerve monitoring was only reported for one patient undergoing local anesthetic-conscious sedation (LA-CS).20 Procedures under LA were largely successful, with only one patient requiring conversion to GA,28 although the reasons for converting from LA-CS to GA were not specified. Sedation agents varied greatly and were reported in 16 studies.10, 14-18, 20-29 Methods of sedation and nausea control used were propofol (n = 5), dexmedetomidine (n = 6), fentanyl (n = 7), midazolam (n = 11), remifentanil (n = 4), sufentanil (n = 2), hydroxyzine (n = 1), meperidine (n = 2), and clonidine (n = 2). The majority of the 16 reported LA regimens used lidocaine (n = 14), with all except one regimen also using adrenaline/epinephrine.25 Alternative agents to lidocaine included bupivacaine (n = 2) and levobupivacaine (n = 1).
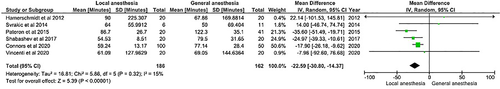
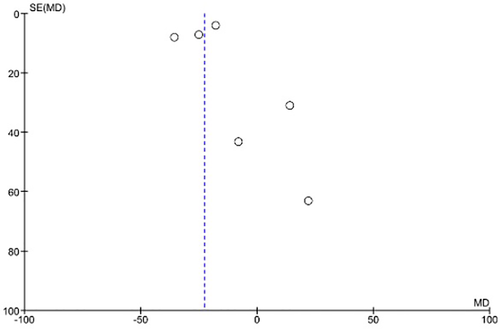
Of six studies which compared operative times between LS-CS and GA,10, 15, 18, 23, 28, 29 four examined the statistical relationship between duration of both procedures.10, 15, 23, 29 Of these, three found a statistically significant difference with a p < .05, and the other by Hamerschmidt et al.10 approached significance. Surgery times for LA-CS compared with GA were: 61.09 compare 69.05 (p = .046),29 54.53 compare 79.50 (p = .001),23 and 86.7 compare 122.3 min (p = .00002).15 In a study by Hamerschmidt in 2012, a Wilcoxon test was performed to compare time of surgery, with a W result of 65.5 this was not significant, but did approach significance, at a p value of .05.10 Meta-analysis using a random effects model showed the mean duration of surgery to be shorter in the LA group by 22.59 min (CI −30.80 to −14.37, p < .00001). The forest plot for this is displayed in Figure 3 and the funnel plot in Figure 4.
Adverse events during or in the postoperative period following cochlear implantation under LA were rare. There were no major adverse events. Of 33 instances of minor adverse events, the most common experienced was vertigo (n = 17), followed by postoperative wound infection (n = 6), temporary facial nerve paralysis (n = 4), confusion (n = 4), residual/new tinnitus (n2). There were no instances of taste disturbance, and no patients required a repeat or revision operation.10, 15, 22, 23, 28-30
Postoperative inpatient hospitalization was compared between groups in six studies and is shown in Table 3. Five studies statistically analyzed differences in inpatient hospitalization following participants procedure, of which three were statistically significant differences.
| Study | Average length of stay (LA) | Number of patients | Average length of stay (GA) | Number of patients | p-Value (<.05 significance) |
|---|---|---|---|---|---|
| Connors et al. | Overnight | 1 | Overnight | 48 | <.001* |
| Hamerschmidt et al. | 394.3 min | 20 | 500 min | 20 | .01* |
| Pateron et al. | 1.15 days | 20 | 1.07 days | 41 | 0.6 |
| Shabashev et al. | 0 day | 20 | 0.3 days | 20 | <.009* |
| Svrakic et al. | Same day 4 Overnight 2 |
6 | Overnight 2 | 2 | Not reported |
| Vincenti et al. | 51.40 min | 20 | 58.30 min | Not reported | .085 |
- Abbreviations: GA, general anesthetic; LA, local anesthetic.
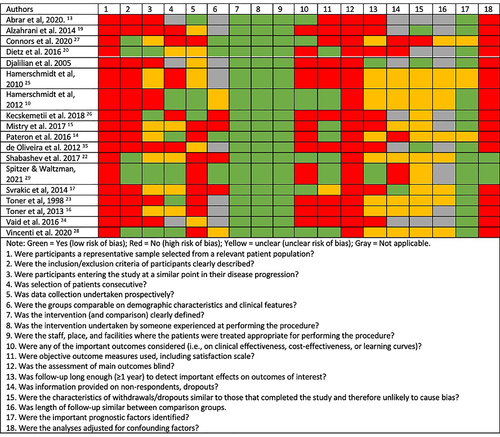
3.6 Risk of bias of included studies
All studies were retrospective with all studies either single case reports, case series or case–control studies with OCEBM grade IV-V. Significant heterogenicity existed between study populations and reporting of primary and secondary outcome measures. Risk of bias assessment is presented in Figure 5. The majority of studies had a high risk of bias. No studies presented a representative sample from a relevant population, the majority of studies did not state clear inclusion or exclusion criteria for entry into their study, with appropriate prognostic and comorbid factors identified. In the majority of studies, patients were not selected consecutively and data collection was not undertaken prospectively, or this was unclear. Most studies did not disclose the qualifications, experience or facilities. In the majority of instances, follow-up was minimal or length of follow-up was unspecified.
4 DISCUSSION
To the authors' knowledge, this systematic review and meta-analysis is the first on the outcomes of cochlear implantation under LA. Overall, results indicate positive audiological and surgical outcomes for the majority of patients who undergo CI under LA and reduced operative time, with potential resource saving implications.
Audiological outcomes from studies which reported these for patients who underwent cochlear implantation under LA showed trends toward improvement. Results showed an overall improvement in PTA, speech discrimination, aided free field audiograms, AzBio sentences, and HINT and CAP scores and were congruent with previous studies published from cohorts who received implants under general anesthesia, with postoperative speech perception scores showing statistically significant increases.31, 32
The results of this systematic review show that LA CI can be used in patients with significant comorbidities. Then, 73/262 patients (46% of those with a recorded ASA) had a severe systemic disease (ASA grade III or IV) without significant complications showing that this surgery is acceptable for high risk patients. Similarly, average P-POSSUM scores for morbidity and mortality were high, at 46.38 and 6.76%, respectively. It is worth noting that data of eight patients presented by Svrakic et al.18 included that of patients with multiple comorbidities which resulted in an average P-POSSUM morbidity of 70.4 ± 6.5% and mortality of 14.8 ± 4.4% for this cohort alone. Excluding this data from the analysis resulted in an average morbidity and mortality of 38.36 and 4.1% for the remaining cohort, respectively. Reported rates of complications were better or comparable to that reported in the literature for GA CIs. Postoperative vertigo is reported to be in the region of 45% after GA which is much higher than that reported for LA CIs in this review 17/262 (6.5%). Wound infection rates are reported to be approximately 4.1% which is similar to this review 6/262 (2.3%).33 Facial nerve paralysis one of the most significant complications of CI surgery widely reported to be approximately 1% for GA CIs was similarly reported in this review as 4/262 (1.5%) with all four temporary.34 In a large-scale review of complications of 403 individuals following cochlear implantation under general anesthesia, Farinetti et al. reported 60 (14.9%) instances of minor complications, and 20 (5%) instances of major complications. Of minor complications, wound infection was reported at a rate of 1.16% and transient facial palsy at a rate of 0.46%, 3.72% vertigo, and 1.24% tinnitus. Major complications reported included revisional surgery in 3.72% and infectious complications such as meningitis, mastoiditis, and tinnitus in 1.24%.35
Lidocaine was most the most commonly used LA, used by 14/18 authors. This was at different stages of the procedure, primarily at the start or end for hemostasis and postoperative pain anesthesia, or during the procedure they can be infiltrated into the surgical field through the tympanotomy and titrated to control pain while approaching the round window.16, 29 Lidocaine is a popular choice; its duration is 30–60 min (increasing to 120 min with adrenaline).14 Bupivacaine acts over 120–240 min (increasing to 240 with adrenaline)14 and levobupivacaine is the longest acting over 240–480 min.14 Intraoperatively, gelfoam soaked with LA can be intermittently administered for local pain relief; however, prolonged application risks paralytic nystagmus from LA absorbing into the round window.28 Paralytic nystagmus was not reported by any authors.
Whether to administer antiemetics is a further question, with three authors stating they used antiemetics to control perioperative and postoperative nausea and emesis risk. Anti-emetics chosen were a combination of dexamethasone and ondansetron, prochlorperazine, droperidol, and ondansetron and dexamethasone.15, 16, 25 Alongside antiemetic effects, Dexamethasone has an added vestibular suppressant effect as well as being used as part of many regimens for hearing preservation. Furthermore, sedation with remifentanil has also been shown to decrease levels of nausea.22
Complications were rare, with only a minor proportion of patients experiencing any complications perioperatively or postoperatively. Vertigo or dizziness were by far the most common minor complication, followed by minor postoperative infections, confusion and transient facial nerve injury. Connors et al. reported an incidence of LA-CS vertigo occurring in as many as 8% of their cohort. Techniques discussed to reduce this intraoperative complication are body-temperature irrigation and temporarily pausing for 2–3 min to allow for IV diazepam administration. They also reported that facial nerve paresis appears to occur at a higher rate in LA-CS operations, at a rate of approximately 1.5% and postulate a cause of higher concentration and volume of LA administration when compared with GA operations, which may infiltrate the stylomastoid foramen, resulting in transient facial palsy.34 They reported that despite this complication, all facial nerve paresis resolved within 2 h postoperatively.28
In the majority of articles, a trend existed toward CI under LA-CS being more cost effective than its GA counterpart. Shabashev et al. found that LA-CS operations had shorter operating and anesthesia times, recovery room times and postoperative length of stay, with significantly cheaper drug costs for those operations performed under LA.23 In these instances, anesthesia drug costs ($47.86 cf. $8.02, p < .0015), anesthesia time (132.45 cf. 89.75 min, p < .0001), surgery time (79.50 cf. 54.53, p < .001), and length of stay postoperatively (0.30 cf. 0.00, p < .009) were all statistically significant. The findings of our meta-analysis support this conclusion for surgery time; however, heterogenicity in studies precluded a meta-analysis of other outcomes.
Unfortunately, the articles identified displayed a high risk of bias, with many either single case reports or small case series with heterogenous reporting and outcome measures. No randomized control trials existed which compared CI under LA-CS to operating under GA. While results were generally positive and indicated that CI under LA-CS was a viable option with minimal risks for patients with multiple comorbidities which excluded them from general anesthesia, larger-scale trials are required to establish a more robust evidence base for this procedure.
5 CONCLUSION
Cochlear implantation under LA with CS is a safe, effective, cost-saving method with results equivalent to implantation under GA and can be utilized for patients with comorbidities which preclude them from general anesthesia. However, larger, more robust studies in direct comparison to general anesthesia are needed to assess this modality further before this technique can be adopted more widely.
APPENDIX
SEARCH TERMS USED FOR ALL DATABASES SEARCHED
- (cochlear ADJ implant*)
- “COCHLEAR IMPLANTATION”/
- “COCHLEAR IMPLANTS”/
- (1 OR 2 OR 3)
- exp “ANESTHETICS, LOCAL”/
- ‘ANESTHESIA, LOCAL”/
- (local ADJ3 (an#esthesia OR an#esthetic*))
- (5 OR 6 OR 7)
- (4 AND 8)
- (cochlear ADJ implant*)
- "COCHLEAR IMPLANTATION"/
- exp "COCHLEA PROSTHESIS"/
- (1 OR 2 OR 3)
- exp "LOCAL ANESTHETIC AGENT"/
- exp "LOCAL ANESTHESIA"/
- (local ADJ3 (an#esthesia OR an#esthetic*))
- (5 OR 6 OR 7)
- (4 AND 8)
- (cochlear ADJ implant*)
- "COCHLEAR IMPLANT"/
- (1 OR 2)
- exp "ANESTHETICS, LOCAL"/
- "ANESTHESIA, LOCAL"/
- (local ADJ3 (an#esthesia OR an#esthetic*))
- (4 OR 5 OR 6)
- (3 AND 7)
- (cochlear implant*)
- (local anesthesia)
- (local anesthesia)
- (local anesthetic*)
- (local anesthetic*)
- (2 OR 3 OR 4 OR 5)
- 1 AND 6
- "cochlear-implant"
- "local anesthetic*"
- "local anesthetic*"
- "local anesthesia”
- "local anesthesia"
- 1 AND (2 OR 3 OR 4 OR 5)
- "cochlear implant*"
- "local anesthetic*"
- "local anesthetic*"
- "local anesthesia”
- "local anesthesia"
- 1 AND (2 OR 3 OR 4 OR 5)