Sublabial bioactive glass implantation for the management of primary atrophic rhinitis and empty nose syndrome: Operative technique
Abstract
Objectives
Atrophic rhinitis (AR) and empty nose syndrome (ENS) are chronic diseases characterized by a paradoxical nasal obstruction. These rare syndromes tend to occur after nasal surgery of the inferior turbinates in ENS and can be idiopathic in AR. Medical treatments alone are often insufficient. Surgical options are challenging and numerous resorbable and nonresorbable implants have been described in small series, with as many surgical techniques described. Whereas current surgical procedures are for risk of extrusions, graft rejections or poor lasting results, the use of GlassBONE™ (Sodimed®, Avignon, France), a bioactive glass, for a vestibular approach in AR and ENS has never been reported for this indication.
Methods
We described an original technique of nasal submucoperiosteal bilateral ceramic glass implantation in two patients with AR and ENS.
Results
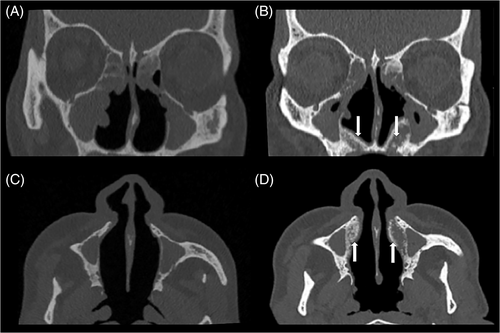
The two cases presented a postoperative satisfying endoscopic and sinus CT-scan results with filling of the nasal cavities, with less crusts and a complete wound healing. They had no short-term complications.
Conclusion
This innovative approach is easily feasible and could be an option considered for the surgical management of AR and ENS.
Level of evidence: 4.
1 INTRODUCTION
Nasal obstruction is a common symptom in otorhinolaryngology daily practice, caused by various etiologies. When nasal obstruction is resistant to appropriate medical treatment and is caused by inferior turbinate (IT) hypertrophy, surgical reduction is usually performed.1 Empty nose syndrome (ENS) and atrophic rhinitis (AR) are two chronic and socially disabling nasal diseases. These rare entities share a similar clinical presentation and some common pathophysiological elements but differ from their etiopathology. ENS is an iatrogenic condition that occurs after excessive loss of turbinate volume, whereas AR is commonly considered as idiopathic. However, some authors describe AR as “primary” if symptoms occur on previously healthy sinonasal structures and “secondary” after surgery, traumatism, infection, or immunological disorders. In our opinion, because the atrophy observed in AR implies a slow evolutive process, whereas turbinectomy leading to ENS is a sudden factor, it would be more appropriate to distinguish AR as “primary” and ENS as “secondary.” In the end, AR and ENS are characterized by reduced mucosal areas and nasal structures, especially at the level of IT leading to a loss of the physiological functions of humidification, warming, and filtration of the inhaled air. These modifications may generate a paradoxical nasal obstruction.2
Management of ENS is problematic and is based in first intention by avoiding excessive turbinate resections.3 After onset of AR or ENS symptoms, medical treatment is the first therapeutic option. The objective of medical treatment is to increase mucosal humidification with nasal irrigation or sprays of physiological saline or sulfur derivatives, nasal moisturizing agents, and humidifiers, directed antibiotics and local corticosteroids in case of additional chronic or acute sinusitis.4 Nasal stimulation with menthol may also decrease the sensation of nasal obstruction.5
Medical treatments are often unsuccessful and therefore surgical treatments may be discussed as a second option. Numerous surgical procedures and different implant materials have been proposed in the literature with a variable rate of clinical improvements. Their objectives are to restore part of the missing IT volume and, as a result, restore normal airflow pattern by reducing the empty nasal space.
The objective of the current study was to describe an innovative technique of a submucoperiosteal bilateral GlassBONE™ (Sodimed®, Avignon, France) bioactive glass implantation in two patients with AR and ENS, by a sublabial approach.
2 METHODS
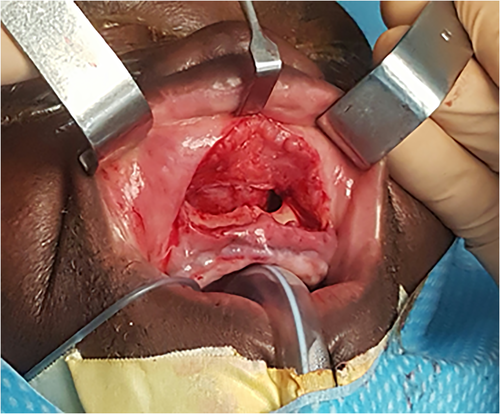
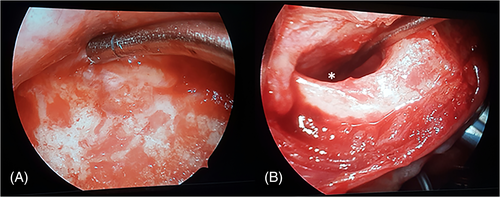
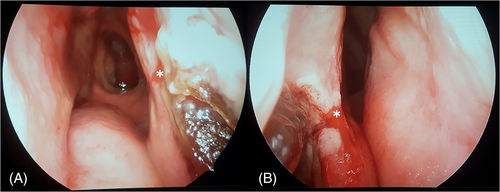
Surgery was performed under general anesthesia. The procedure lasted 1 h. After infiltration with 2 ml of xylocaine and adrenaline at 1%, a vestibular sublabial approach was performed to access the piriform aperture (Figure 1). The sublabial incision was median and unique for the patient in case 1, and two separate sublabial incisions were made for the patient in case 2 to expose separately the left and the right maxillary bone. The dissection was then continued under endoscopic control in a submucoperiosteal plane, with respect of the anterior nasal spine region (Figure 2). The dissection was conducted on both sides, until the nasal floor was widely exposed, and the lateral nasal wall was exposed up to the maxillary bone. Nonhumidified ceramic glass implant was then gradually placed using a spatula in the newly created submucoperiosteal space. Approximately 10 ml of GlassBONE™ was placed in each nasal cavity. The implant was sculpted to allow a good filling of the anterior and lateral part of nasal cavities, thus narrowing nasal cavities bilaterally (Figure 3). The vestibular mucosa was closed by a simple absorbable suture. The postoperative care consisted of grade I and II analgesics, nasal saline irrigation, daily mouthwashes and the application of an ice pack on the upper lip to prevent excessive swelling during the first 3 days.
The two patients included retrospectively gave their informed consent to participate in the study (Centre Hospitalier Intercommunal de Créteil Ethics Committee exemption).
3 RESULTS
3.1 Case 1
Patient 1 was a 57-year-old male with primary AR, in failure of conservative management. He complained of a paradoxical nasal obstruction, anosmia, nasal crusting, and dyspnea during exercise. Endoscopic examination showed severe bilateral atrophy of the IT, wide nasal cavities, and an anterior septal perforation with crusting. The preoperative sinus CT-scan showed significant bone remodeling with large nasal cavities and subcomplete opacities of the sinus. The Visual Analog Scale of nasal obstruction was 10/10 for both sides.
Surgery was performed according to the technique described below. No complication occurred and the patient was discharged home on the next day. One month after surgery, nasal obstruction decreased significantly and endoscopic control showed a satisfying filling of the nasal cavities, with less crusts and the wound healing was complete. Conversely, after 6 months, while the endoscopic aspect was unchanged, the patient asked for the GlassBONE™ to be removed because of a recurrent nasal obstruction (Figure 4). The patient has received concomitant psychological follow-up.
3.2 Case 2:
Patient 2 was a 73-year-old male with ENS. An inferior turbinectomy was performed 22 years ago to manage nasal obstruction. He self-complained of paradoxical nasal obstruction and nasal dryness, predominant during night. Rhinomanometry showed normal resistances and a paradoxical effect of vasoconstrictors. The preoperative sinus CT-scan showed hypertrophy of the posterior septal mucosa with large and empty nasal cavities. Surgery was performed according to the technique described below. No complication occurred and the patient was discharged home on the next day. Four months after the surgery, the endoscopic aspect was satisfying, and the patient experienced a long-term improvement of nasal obstruction.
4 DISCUSSION
The persistent nasal obstruction felt in AR and ENS is unusual because associated with a paradoxically wide nasal fossa at clinical examination and often normal/sub-normal nasal resistances. The associated symptoms are nasal crusting, facial pain, dyspnea, sleeping disorders and smelling foul odors in AR.6 The physiopathology of secondary ENS after surgery of the inferior turbinates is controversial and still poorly understood because it is multifactorial. Two main hypotheses have been retained. The first physiological hypothesis involves disruption of the inhaled air by the loss of sensory, tactile and thermal receptors due to the reduced turbinal mucosal7 decreasing humidification, filtration and reducing nasal airflow resistance.5 The second physical hypothesis involves disruption of the nasal flow regime with an unbalance between the superior and inferior nasal cavity, resulting in an alteration of pulmonary gas exchange. The nasal resistance plays a role in the opening of pulmonary bronchioles and physiological alveolar oxygenation.2 Reduced nasal resistance may be perceived by central respiratory centers as a respiratory distress and leads to hyperventilation syndrome in 77% of cases of ENS.5, 8 Disorders of the central nervous system in ENS are currently being studied and could explain the subjective nasal congestion by a perturbation of neural mucosal efferent pathways and impaired intranasal trigeminal function.5, 9 A recent study on histopathological characteristics of ENS found significantly more squamous metaplasia, a higher rate of submucosal fibrosis, a lower number of submucosal glands and a lower expression level of thermoreceptor-like transient receptor potential channel melastatin 8 (TRPM8).10 While ENS and AR share the same symptoms, an extra inflammatory process can be found on mucosal histology of patients with primary AR.11 Primary AR is a debilitating chronic nasal disease of unknown etiology, whose diagnosis is essentially made by exclusion of other nasal atrophic conditions. The main etiopathological factors described in literature are heredity, chronical bacterial infection of the nasal cavities by Klebsiella species (especially K. Ozaenae), and poor hygienic conditions.12
Management of these two pathologies is problematic because of a high rate of failure of medical treatments, which are purely symptomatic with use of nasal irrigations. Only few data are available on the success rate of the medical treatment alone. Only one randomized controlled trial has compared medical treatments of AR and measured the subjective improvement as perceived by the patient on a scale of 1–10 (1 being the worst score and 10 being the best score). It was found that alkaline nasal douching only provided a subjective improvement score of 2.8/10 after 12 weeks of treatment.13 In case of strong patient demand, a surgical procedure can be performed as a second option. In all cases, it is necessary to remain prudent about therapeutic objectives that can reasonably be reached. It may be appropriate to consider a psychological evaluation before surgery.4
Surgical procedures are challenging on many aspects. First, finding the most suitable material for implantation is of great importance. The ideal material used to restore volume in the nasal cavity should be well tolerated and present a low risk of rejection, extrusion, and infection. All implants have specific advantages and disadvantages. Numerous different nonresorbable filler materials and implants have been previously used in both these entities: autologous costal/septal/conchal cartilage,14, 15 acellular dermis graft,2 plastipore plates,16 and ß-tricalcium phosphate,17 goretex, or teflon implants. Cartilage graft has the advantage of being an autologous material, with excellent tolerance and integration, but implies a new mucosal trauma by removing septal cartilage and adds donor-site morbidity with costal or conchal grafts. Cartilage implants also tend to resorb over time.14, 15 Acellular dermis graft filling shows a durable volume restoration and is easy to handle because of its readily shaped presentation but has the inconvenient of initial shrinkage that must be anticipated during the procedure. Cases of minor exposure have been described in the first 2 weeks after implantation, with spontaneous healing.2 Implantation of plastipore plates with micropores offers good results and can be performed under local anesthesia, but a case of late rejection has been described 18 months after a surgery.16 All these techniques use mucosal flaps with risks of flap necrosis and implies new mucosal traumas. To avoid this, resorbable filler materials use have also been described: glycerin gel injections, injectable hyaluronic acid gel and hydroxyapatite, and showed good results on symptoms with no further complications in small series. Resorbable fillers can be interesting in the first line of treatment for patients initially reluctant to surgical treatment but they only provide transient volume augmentation and their benefits start to decrease after 3 months.18 Filler injection techniques are also limited by the maximal volume that can be injected at each site, the risk of mucosal rupture, filler leakage, and waste, depending on mucosal characteristics.2, 19 GlassBONE™ is a well-known synthetic bioactive ceramic, composed of natural elements similar to bone tissue composition. In form of glass granules, it stimulates osteogenesis and bone regeneration. The biocompatibility and good tolerance of ceramics implanted under sinonasal mucosa has previously been shown in preclinical and clinical studies.17, 20 Bioactive glass is also widely used for mastoid obliteration in chronic otitis surgery, with very good cutaneous and inner ear tolerance.21 Nevertheless, to our knowledge, it is the first time that GlassBONE™ has been used in primary AR and ENS.
Second, the most suitable surgical approach according to previous surgical history of the patient must be thought out and anticipated. In previous studies, the implant placement by nasal endoscopic approach was made in the septum, floor, or lateral nasal wall and was possible only if there was some residual turbinate left.22 Mucosal incisions and septal flaps in patients suffering from AR and ENS can be challenging if patients have undergone previous septoplasty or endoscopic nasal surgery. The transmucosal approach has the disadvantage of creating a new trauma of the nasal mucosa, and thus, increasing inflammatory phenomena, which participate in the pathophysiology of AR and ENS. Exclusive endonasal approaches may also cause crusting, flap necrosis, implant extrusion, infection, synechia, lacrimal obstruction, postoperative swelling, wound rupture, and implant exposure.2 To avoid this, an alternative approach of medialization of the intersinonasal wall has been described, with however, a risk of nasolacrimal duct obstruction and postoperative epiphora.22 Few authors described a vestibular sublabial approach to reduce the size of the nasal cavities in AR. In the Raghav Sharan's operation, a Caldwell-Luc procedure was performed followed by antrostomy through the inferior meatus and the mucosa of the maxillary antrum was elevated and brought into the nasal cavity.2 Lautenschlager et al. used the same approach to medialize the lateral nasal wall or the medial wall of the maxillary antrum.23 Bertrand et al. used a labial vestibule approach to place a triosite implant with fibrin glue in nine patients, with no case of rejections.24 Bastier et al. implanted ß-Tricalcium phosphate ceramic implants under the mucoperiosteal plane of the lateral nasal wall in 14 patients suffering from ENS, with good tolerance and long term results, and only one case of implant exposure.17
Our study describes the first case of a vestibular submucoperiosteal bioceramic GlassBONE™ implantation in primary AR and ENS. The advantage of this approach is to avoid the incision of the nasal mucosal, therefore reducing the above-mentioned risks. The approach is exclusively vestibular and has the advantage of being possible when there is no more residual turbinate left. Given its presentation in form of glass granules, GlassBONE™ allows a good modeling of the newly created mucosal volume and no suture is needed to fix the implant. Nevertheless, the manipulation of granules can be challenging during implantation with a potential risk of secondary extrusion in the sublabial tissues if the wound is not perfectly closed. There is also a risk of mucosal perforation during the creation of the submucoperiosteal tunnel, with extrusion or exposure of granules in the nasal fossa. The volume to be implanted is left to the appreciation of the surgeon, with a potential risk of under or overcorrection and a risk of failure. This technique seems to be a good alternative to the transmucosal nasal approach in severe selected cases of AR and ENS, especially for patients who had previously undergone nasal surgery. The site of implantation should still be chosen given the medical history and preoperative endoscopic and sinus CT findings. Further cohorts extended follow-up are needed to assess this technique in AR and ENS surgical management.
5 CONCLUSION
We describe a novel and original technique of surgical management of primary AR and ENS with GlassBONE™ implant in a submucoperiosteal approach in two patients. Short-term endoscopic and radiologic images provided promising results with an improvement of nasal symptoms. Long term results of this technique in terms of long-lasting volume, tolerance and symptoms scores must be evaluated in larger series.
ACKNOWLEDGMENT
The authors would like to thank Pamela Haylock for English-language editing.
CONFLICT OF INTEREST
All the authors have read and agreed with the article's content. No authors have financial or personal conflicts. Neither the work nor any part of its essential substance, tables or figures have been or will be published or submitted to another scientific journal or are being considered for publication elsewhere.