Pneumococcal conjugate vaccines reduce myringotomy with tympanostomy tube insertion in young children in Japan
Abstract
Objective
Pneumococcal conjugate vaccines (PCVs) have been reported to reduce the incidence of myringotomy with tympanostomy tube insertion (MTTI) in children. However, little information is available focusing specific ages. We examined the prophylactic efficacy of PCVs on the onset of complex otitis media (ComOM) that requires MTTI.
Method
From 2011, the public support for PCV7 started with the usual four-dose schedule and an emergency schedule for 2- to 4-year-old children in Japan. PCV7 was replaced with PCV13 in 2013. We reviewed the nationwide database obtained from the JMDC Claims Database (https://www.jmdc.co.jp/en/) to examine the MTTI incidence during the era before and after PCV introduction (from 2008 to 2010 and from 2011 to 2017, respectively). Subjects were analyzed by stratified age groups (from 0 to 8 years old) and in subdivided groups of 6 months (from 0 to 35 months old). We compared the MTTI incidence between the groups for each age as well as between those for each calendar year.
Results
A significant reduction in the MTTI incidence was detected in the 1-year-old children of the PCV era compared to those of the pre-PCV era. The reduction rates were more prominent in the 12–17 months group as compared to the 18–23 months group (PCV7 p = .005 and PCV13 p = .011, PCV7 p = .014 and PCV13 p = .153, respectively). The significant difference in the 1-year-old children continued in six of seven calendar years from 2011 to 2017, whereas no significant reduction was detected in children >3 years old.
Conclusions
The introduction of both PCV7 and PCV13 reduced MTTI incidences in children around 1 year old, and the effects were more prominent during the early half-periods. Our results support etiological evidence that pneumococcal infection in children aged 1 year and younger might play roles in the pathogenesis of ComOM that requires MTTI.
1 INTRODUCTION
Myringotomy with tympanostomy tube insertion (MTTI) is a surgical procedure designed to treat the prolonged conductive hearing loss that occurs due to otitis media with effusion (OME). MTTI is also one of the methods used to reduce the recurrence of acute otitis media (AOM). Many studies have indicated that a bacterial ribonuclear acid is present in the middle ear effusions (MEFs) of OME patients.1, 2 In their 2016 systemic review, Ngo et al. reported that higher rates of bacterial components were detected in the MEF of patients with AOM, recurrent AOM (ROM), and OME by a combination of standard bacterial analyses and PCR methods.3 Therefore, bacterial infection is speculated to play a role in the pathogenesis of OME.4
Streptococcus pneumoniae is one of the major causative microorganisms of AOM in children. The effectiveness of the heptavalent pneumococcal conjugate vaccine (PCV7) against AOM has been examined in respect to the total number of AOM episodes and the number of visits to healthcare facilities in pediatric patients. Meta-analyses indicated that PCV7 exerted preventive effects on pneumococcal AOM episodes and unidentified effects on AOM from all-causes.5-7 With the use of databases across the total age groups, this vaccination was shown to reduce the rates of ROM and MTTI. Some studies further suggest prophylactic effects on the onset of ROM and the incidence of MTTI caused by complex otitis media (ComOM).8-14 However, little information is available about specific age groups who would receive health benefit from the prevention of ComOM that requires MTTI.
We conducted the present study to investigate the etiological changes in the incidence of MTTI for pediatric ComOM in Japan after the introduction of PCV7 and PCV13 from the year of 2011 supported by a public health care program. For this purpose, we used the nationwide real-world database from multiple health insurance associations directed by the Ministry of Health and Welfare in Japan. The classification of otitis media (OM) was based on the International Classification of Diseases 10th Revision (ICD-10). The database was analyzed based on the groups of children stratified by age from 0 to 8 years old. We compared the MTTI incidence between the groups for each year of age as well as between those for each calendar year from 2008 to 2017. A subgroup analysis was conducted between the groups for every 6-month period from 0 to 35 months old. In Japan, mainly ear/nose/throat (ENT) specialists diagnose and manage OME cases on outpatient clinic base. We therefore consider that the ICD-10 classification of OM is reliable and tends to show a normalized distribution in terms of socioeconomic backgrounds.
2 SUBJECTS AND METHODS
The study protocol was approved by the Ethics Committee at Hiroshima University (protocol No. E-953-1). PCV7 was launched and gained public funding in early 2011 of the Japanese market. In 2011 and 2012, the Japanese Government Policy on Emergency Vaccination (JGPonEV) encouraged three vaccinations of 7- to <12-month-old infants, two vaccinations of 12- to <24-month-old children, and a single vaccination of 24- to <60-month-old children. Typically, infants were vaccinated four times with PCV7: three doses before 12 months of age and one dose at 12–15 months of age as a booster dose. PCV7 was replaced with PCV13 in November 2013.
We used nationwide data collected from the JMDC Claims Database (https://www.jmdc.co.jp/en/) which is Japan's largest epidemiological receipt database. They accumulate health insurance receipts of insured individuals and their families those who were covered by the multiple health insurance associations. The maximum number of monthly enrollments for each age group in each calendar year served as the study population for the present analyses. The data of patients <15 years of age were used for this pediatric OM analysis. The following diagnoses in the ICD-10 were used to identify the targets for the OM analysis (Table 1): H65.2 (chronic serous OM), H65.3 (chronic mucoid OM), H65.4 (other chronic nonsuppurative OM), H65.9 (unspecified nonsuppurative OM), H66.0 (acute suppurative OM), H66.4 (suppurative OM, unspecified), and H66.9 (otitis media, unspecified). We consider that these disease categories include nearly 90% of the causative diseases for MTTI indications in the study.
| Codes of nonsuppurative otitis media | Codes of suppurative and unspecified otitis media |
|---|---|
| H65, Nonsuppurative otitis media | H66, Suppurative and unspecified otitis media |
| H65.1, Other acute nonsuppurative otitis media | H66.0, Acute suppurative otitis media |
| # H65.2, Chronic serous otitis media | H66.1, Chronic tubotympanic suppurative otitis media |
| # H65.3, Chronic mucoid otitis media | H66.2, Chronic atticoantral suppurative otitis media |
| # H65.4, Other chronic nonsuppurative otitis media | H66.3, Other chronic suppurative otitis media |
| # H65.9, Unspecified nonsuppurative otitis media | H66.4, Suppurative otitis media, unspecified |
| H66.9, Otitis media, unspecified |
- Note: Codes with # were used as OME.
- Abbreviations: ICD-10, International Classification of Diseases 10th Revision; OME, otitis media with effusion.
Changes in the average rate of MTTI were analyzed for the 10-year period from 2008 to 2017. The period was subdivided into three eras based on the PCV introduction and types. They are called the pre-PCV era (2008–2010), the PCV7 era (2011–2013), and the PCV13 era (2014–2017). The comparison was made among the three era groups classified by year age (from 0 to 8 years old) and by 6-month age (from 0 to 35 months old). The distribution of the overall MTTI rates was calculated for each year age group, and the difference was compared between the pre-PCV era and the two PCV eras.
2.1 Statistical analyses
We used the χ2-test to examine differences in the MTTI incidences between the groups for era and for each age (years and months).
3 RESULTS
To estimate the actual vaccination rate in children in Japan, we obtained the medical records from the Health Services and Welfare Division of Hiroshima City. The records indicated that the rate of PCV7 vaccination in infants born in Hiroshima City as of March 2012 was 100% based on the calculated number of vaccine lots and the targeted age population.15 The average population of children from 0 to 14 years old in Japan during 2008–2017 was 17,963,400 (51% males, 49% females) according to the Ministry data. We used the data of the total of 4,593,845 cases among children of all ages on the JMDC Claims Database; the number of MTTIs in this population was 7600 (62% males, 38% females).
Table 2 shows summarized data of the number of cases, total population, incidence rates, and statistical results for each age group under 8 years old from 2008 to 2017. We found that approx. 90% of the MTTI cases were identified as derived from OME listed on ICD-10 codes (# in Table 1). The remaining 10% were suspected to be caused by ROM.
| Year | Age, years → | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|---|---|
| 2008 | No. VTI | 9 | 46 | 23 | 21 | 22 | 24 | 12 | 5 | 4 |
| Population | 6352 | 6619 | 6566 | 6237 | 6593 | 6477 | 6557 | 6489 | 6739 | |
| Rate per 10,000 | 14 | 69 | 35 | 34 | 33 | 37 | 18 | 8 | 6 | |
| 2009 | No. VTI | 15 | 64 | 25 | 16 | 18 | 32 | 25 | 16 | 10 |
| Population | 8736 | 8889 | 9009 | 8851 | 8572 | 8917 | 8840 | 9013 | 8957 | |
| Rate per 10,000 | 17 | 72 | 28 | 18 | 21 | 36 | 28 | 18 | 11 | |
| 2010 | No. VTI | 39 | 125 | 50 | 38 | 47 | 51 | 31 | 27 | 10 |
| Population | 15,379 | 15,521 | 15,209 | 15,101 | 14,734 | 14,153 | 14,789 | 14,624 | 14,772 | |
| Rate per 10,000 | 25 | 81 | 33 | 25 | 32 | 36 | 21 | 18 | 7 | |
| Total of pre-PCV | No. VTI | 63 | 235 | 98 | 75 | 87 | 107 | 68 | 48 | 24 |
| Population | 30,467 | 31,029 | 30,784 | 30,189 | 29,899 | 29,547 | 30,186 | 30,126 | 30,468 | |
| Rate per 10,000 | 21 | 76 | 32 | 25 | 29 | 36 | 23 | 16 | 8 | |
| 2011 | No. VTI | 58 | 109 | 69 | 57 | 59 | 47 | 64 | 25 | 14 |
| Population | 19,186 | 19,499 | 19,250 | 19,094 | 18,931 | 18,523 | 18,114 | 18,827 | 18,566 | |
| Rate per 10,000 | 30 | 56 | 36 | 30 | 31 | 25 | 35 | 13 | 8 | |
| CHISQ.TEST | 0.0355* | 0.0083** | 0.4493 | 0.2946 | 0.6834 | 0.0407* | 0.0091** | 0.4591 | 0.8967 | |
| 2012 | No. VTI | 50 | 154 | 81 | 60 | 70 | 59 | 54 | 33 | 26 |
| Population | 24,699 | 25,056 | 25,133 | 24,583 | 24,600 | 24,252 | 23,970 | 23,416 | 24,305 | |
| Rate per 10,000 | 20 | 61 | 32 | 24 | 28 | 24 | 23 | 14 | 11 | |
| CHISQ.TEST | 0.9107 | 0.0429* | 0.9346 | 0.9184 | 0.8892 | 0.0134* | 0.9998 | 0.5868 | 0.2775 | |
| 2013 | No. VTI | 71 | 214 | 115 | 86 | 101 | 108 | 93 | 54 | 30 |
| Population | 38,741 | 39,910 | 39,394 | 39,394 | 38,576 | 38,769 | 38,314 | 37,844 | 36,799 | |
| Rate per 10,000 | 18 | 54 | 29 | 22 | 26 | 28 | 24 | 14 | 8 | |
| CHISQ.TEST | 0.4849 | 0.0002*** | 0.5277 | 0.4123 | 0.4695 | 0.0534 | 0.6394 | 0.5777 | 0.9001 | |
| Total of PCV7 | No. VTI | 179 | 477 | 265 | 203 | 230 | 214 | 211 | 112 | 70 |
| Population | 82,626 | 84,465 | 83,777 | 83,071 | 82,107 | 81,544 | 80,398 | 80,087 | 79,670 | |
| Rate per 10,000 | 22 | 56 | 32 | 24 | 28 | 26 | 26 | 14 | 9 | |
| CHISQ.TEST | 0.7503 | 0.0002*** | 0.9568 | 0.9027 | 0.7622 | 0.0062** | 0.2723 | 0.4490 | 0.6439 | |
| 2014 | No. VTI | 75 | 231 | 99 | 81 | 107 | 112 | 98 | 66 | 36 |
| Population | 40,163 | 41,927 | 42,259 | 41,762 | 41,565 | 40,882 | 40,996 | 40,642 | 40,001 | |
| Rate per 10,000 | 19 | 55 | 23 | 19 | 26 | 27 | 24 | 16 | 9 | |
| CHISQ.TEST | 0.5502 | 0.0005*** | 0.0305* | 0.121 | 0.3951 | 0.0381* | 0.7065 | 0.92 | 0.6127 | |
| 2015 | No. VTI | 80 | 311 | 119 | 94 | 120 | 133 | 105 | 53 | 39 |
| Population | 49,258 | 49,726 | 50,659 | 50,712 | 50,229 | 50,106 | 49,635 | 49,715 | 49,340 | |
| Rate per 10,000 | 16 | 63 | 23 | 19 | 24 | 27 | 21 | 11 | 8 | |
| CHISQ.TEST | 0.1502 | 0.0261* | 0.0251* | 0.0574 | 0.1602 | 0.0162* | 0.6859 | 0.0422* | 0.9894 | |
| 2016 | No. VTI | 93 | 355 | 110 | 134 | 149 | 177 | 117 | 72 | 36 |
| Population | 49,877 | 52,285 | 51,353 | 52,309 | 52,349 | 52,007 | 51,990 | 51,578 | 51,639 | |
| Rate per 10,000 | 19 | 68 | 21 | 26 | 28 | 34 | 23 | 14 | 7 | |
| CHISQ.TEST | 0.5255 | 0.1921 | 0.004** | 0.8314 | 0.8699 | 0.6115 | 0.9947 | 0.4772 | 0.6427 | |
| 2017 | No. VTI | 77 | 314 | 163 | 125 | 119 | 160 | 142 | 79 | 52 |
| Population | 49,020 | 51,430 | 52,192 | 51,220 | 52,059 | 52,055 | 51,812 | 51,762 | 51,293 | |
| Rate per 10,000 | 16 | 61 | 31 | 24 | 23 | 31 | 27 | 15 | 10 | |
| CHISQ.TEST | 0.1042 | 0.012* | 0.8807 | 0.9027 | 0.0859 | 0.188 | 0.1823 | 0.814 | 0.3051 | |
| Total of PCV13 | No. VTI | 325 | 1211 | 491 | 434 | 495 | 582 | 462 | 270 | 163 |
| Population | 188,318 | 195,368 | 196,463 | 196,003 | 196,202 | 195,050 | 194,433 | 193,697 | 192,273 | |
| Rate per 10,000 | 17 | 62 | 25 | 22 | 25 | 30 | 24 | 14 | 8 | |
| CHISQ.TEST | 0.1881 | 0.0047** | 0.0281* | 0.3566 | 0.2187 | 0.0648 | 0.6809 | 0.3927 | 0.7367 |
- Note: Populations are the maximum number of children who belonged to the JMDC Claims Database for each age group in each calendar year. *p < .05. **p < .01. ***p < .001 by χ2-test.
- Abbreviations: MTTI, myringotomy with tympanostomy tube insertion; PCV, pneumococcal conjugate vaccine.
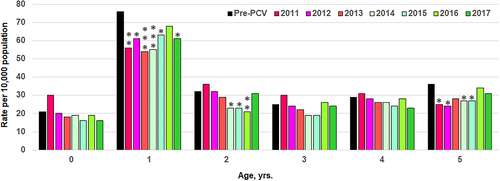
Figure 1 illustrates changes in the mean rates of MTTI for each year age in the pre-PCV era (2008–2010), the PCV7 era (2011–2013), and the PCV13 era (2014–2017). The mean rates of MTTI in 1-year-old children were significantly reduced in both the PCV7 and PCV13 eras compared to that in the pre-PCV era. The rates (per 10,000 age population) were 56 for PCV7, 62 for PCV13, and 76 for pre-PCV. As shown in Figure 2, the significant reduction of MTTI in the group of 1-year-old children continued in six of seven consecutive calendar years after the introduction of the PCV program from 2011; the exception was 2016. Partial reduction was observed in the groups of 2- and 5-year-old children. No significant reduction was observed in the groups of 0-, 3-, and 4-year-old children. This is in contrast with the fact that all of the enrolled children <5 years old had been vaccinated more than once due to the JGPonEV rescue program since 2011.
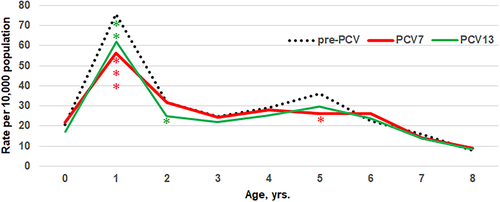
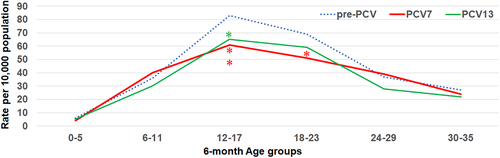
Because the mean MTTI rates in the group of 1-year-old children decreased significantly after the introduction of PCV, we conducted a subgroup analysis in a group of children <3 years old (Table 3). Figure 3 summarizes the changes in the mean MTTI rates subdivided into 6-month period in the three era groups. We observed that the decrease was significant especially in the 12- to 17-month-old group rather than in the 18- to 23-monthold group (PCV7 p = .005 and PCV13 p = .011 for the 12- to 17-month-old group; PCV7 p = .014 and PCV13 p = .153 for the 18- to 23-month-old group). These results suggest that the prophylactic effects appear more prominent during the early half periods of the one-year-old group.
| Year | Age, months | 0–5 | 6–11 | 12–17 | 18–23 | 24–29 | 30–35 |
|---|---|---|---|---|---|---|---|
| Pre–PCV | No. VTI | 9 | 54 | 131 | 104 | 58 | 40 |
| Population | 15,556 | 14,911 | 15,854 | 15,175 | 15,731 | 15,053 | |
| Rate per 10,000 | 6 | 36 | 83 | 69 | 37 | 27 | |
| PCV7 | No. VTI | 17 | 162 | 268 | 209 | 169 | 96 |
| Population | 42,383 | 40,243 | 43,629 | 40,836 | 43,076 | 40,701 | |
| Rate per 10,000 | 4 | 40 | 61 | 51 | 39 | 24 | |
| CHISQ.TEST | n.a. | 0.500 | 0.005** | 0.014 | 0.682 | 0.526 | |
| PCV13 | No. VTI | 44 | 281 | 658 | 553 | 287 | 204 |
| Population | 96,077 | 92,241 | 101,420 | 93,948 | 102,225 | 94,238 | |
| Rate per 10,000 | 5 | 30 | 65 | 59 | 28 | 22 | |
| CHISQ.TEST | n.a. | 0.243 | 0.011 | 0.153 | 0.057 | 0.234 |
- Note: Populations are the maximum number of children who belonged to the JMDC Claims Database for each age group in each calendar year. *p < .05. **p < .01 by χ2-test. n.a.: not available.
- Abbreviations: MTTI, myringotomy with tympanostomy tube insertion; PCV, pneumococcal conjugate vaccine.
4 DISCUSSION
OME is usually treated medically, and MTTI is indicated mainly for prolonged cases, although controversy remains regarding the indications. The incidence of MTTI thus reflects the rate of severe OME among children and pediatric ROM (which often accompanies uncontrollable repeated eustachian tube infection). Altogether, our findings indicate that the MTTI incidence can be employed as a useful marker that reflects the prevalence of severe ComOM. In this sense, etiological analyses using a large database require accurate diagnoses. In the study, we used the nationwide real-world database from multiple health insurance associations directed by the Ministry of Health and Welfare of Japan. The system maintains healthcare standards through the public health insurance coverage system.16 We therefore consider that the dataset used herein is unlikely to contain any bias in the distribution of patient demographics in respect to socioeconomic status, residence area, and income.
Prophylactic effects of PCV were examined in studies of the 10-valent pneumococcal non-typable Hemophilus influenzae protein D conjugate vaccine (PHiD-CV); most of the studies reported a reduction in the MTTI incidence by PHiD-CV.17-19 Investigations conducted after the introduction of PCVs indicated that both PCV78-14, 20 and the subsequent introduction of PCV13 continued to reduce the incidence of MTTI.21-23 However, most of those etiological studies were conducted based on the use of the whole data with all age groups of children. There are few studies available for the specific age groups who would receive benefit for the prevention of ComOM that requires MTTI.
In 2016, Dagan et al. hypothesized that the prevention of early episodes of OM by pneumococcal vaccines might reduce the progression to complex diseases.24 Their results suggest that PCVs are useful to reduce the frequency of severe ComOM. However, they did not discuss the specific ages at which PCVs may act most effectively or how long the vaccination effects will last. It is difficult to answer these questions with a prospective cohort study and multiple-center analysis, because the research entails high costs and requires a large pediatric population. Against this background, we used a nationwide real-world database in the present study because it has the advantages of providing a large population for each age during designated years with little bias based on the reliable health insurance records.
Jardine et al. noted that PCV7 administered on a three-dose schedule at 2, 4, and 6 months of age was routinely used in Australia without a booster shot, and they observed a significant effect on the total number of MTTIs.13 They reported the adjusted incidence of MTTI in children was significantly reduced by 23, 16, and 6% for children aged <1, 1, and 2 years old, respectively. In contrast, the standard four-dose schedule in Japan includes a booster shot at 12–15 months of age. We found that the incidences of MTTI in 1-year-old significantly decreased by 26 and 18% in the PCV7 and PCV13 eras, respectively. These results might imply the augmented prophylactic effects of the last booster shots on the onset of severe ComOM that requires MTTI around this period.
Our present study contains three main findings. (1) A significant reduction of the MTTI incidence was detected among 1-year-old children after the introduction of PCVs (26% for PCV7 and 18% for PCV13, respectively). (2) No significant reduction was observed for infants (0-year-old) and 3- to 4-year-old children. (3) The results of the 6-month age-group analysis demonstrated that the prophylactic effects were more prominent during the early half of the first year of 1 year old, especially in the 12- to 17-month-old group. Taken together, these results suggest that the reduction in the MTTI incidence is not evenly distributed among all children, except for the group of 1-year-old children, who often suffer severe ComOM that requires MTTI.
Our results coincide with reports from randomized studies that estimated the vaccine effects for older children with ROM or OME who were vaccinated with PCV7 followed by a 23-valent pneumococcal polysaccharide vaccine (PPSV23)25-27 Veenhoven et al. reported that combined vaccination did not affect the next occurrence of AOM and MTTI reduction in children >1 year old in Netherlands.25 There was no protective effect of combined vaccination on AOM recurrences in older children aged 1–7 years in a study in Belgium.26 Van Heerbeek et al. reported that a combined vaccination did not prevent the recurrence of OME among children aged 2–8 years old.27 Considering the findings of these studies together with ours, it appears that the first vaccination for children >1 year old seems to have no ability to reduce the development of ROM or OME.
Few studies have compared the MTTI incidence before and after the introduction of PCV in different age groups of children. In the present study, the notable changes in the MTTI incidence mainly reflected the fact that >90% of the MTTIs were performed for children with severe OME based on the ICD-10 codes. In Japan, ENT specialists examine and treat most of patients with middle ear disease on an outpatient clinic basis. We speculate that the risk of MTTI patients being left off the database might be low enough to obtain reliable statistics in this study.
It remains to be determined whether the prevalence of MTTI derived from other causes including ROM shows the same tendency. Earlier studies including meta-analyses have shown that the effects of PCV7 on AOM remain unclear. The controversies include the vaccine's ability to reduce the incidence of AOM episodes and the frequency of emergency room visits for AOM.5-7 Other studies have reported that PCVs reduce the incidence of MTTI caused by OME and recurrent OM. The Japanese guidelines for pediatric AOM recommend a myringotomy for moderate-grade cases with severe local findings, severe-grade cases, and treatment-resistant cases. The incidence of myringotomy thus reflects the prevalence of severe AOM in Japan.28
Sugino et al. reported that the rate of myringotomies performed for AOM in 1-year-old infants decreased significantly 2 years after the introduction of PCV7 compared to the rate before its introduction.15 Our previous investigations also revealed a significant decline in the rate of myringotomies for AOM among 1- and 5-year-old children after the introduction of PCV7.29 The present results together with those of the previous studies further indicate a close relationship between the pathogeneses of prolonged OME and ROM and eustachian tube dysfunction triggered by bacterial infection in children, especially those ≤1 year old. This may also explain the etiological findings that effects of PCVs do not manifest in children >2 years old.
5 CONCLUSION
Our analysis of a nationwide database in Japan indicates that both the PCV7 and PCV13 inoculations reduced the incidence of MTTI for ComOM in younger children. The prophylactic effects were more prominent in the early half of the first year of age. Our results support etiological evidence that pneumococcal infection in children ≤1 year old might play roles in the pathogenesis of ComOM that requires MTTI.
ACKNOWLEDGMENT
The authors thank the clinical research center of Hiroshima University for their support for the statistical analyses.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.