Investigation of the Position and Angle of the Vocal Fold Projected onto the Thyroid Cartilage
This study was supported by JSPS KAKENHI Grant Number JP18K16862.
The author have no conflicts of interest directly relevant to the content of this article.
Abstract
Objective
To perform laryngeal framework surgery for unilateral vocal fold paralysis and obtain favorable voice improvement, it is necessary to accurately determine the vocal fold and arytenoid cartilage positions. Thus, the position and angle of the paralyzed vocal folds and arytenoid cartilage projected onto the affected thyroid plate were measured using computed tomography (CT) before and after surgery.
Methods
Forty-six male patients with thyroid cartilage ossification observed on preoperative CT and vocal fold paralysis were included. Using Adobe Illustrator®, the thyroid plate on the affected side was reconstructed from the continuous images of the sagittal section of the CT examination during participant's quiet breathing (reconstructed affected thyroid plate [RATP]).
Results
The anterior commissure mean position was slightly cranial to the midpoint of the thyroid cartilage midline. The paralyzed vocal fold angle was not parallel to the baseline. The average unaffected vocal fold angle during vocalization projected onto the affected thyroid plate was 13.83°, which differed significantly from the average paralyzed vocal fold angle before surgery (19.05°). However, no significant difference was observed in comparison with the average angle of the paralyzed vocal fold after arytenoid adduction. The average distance from the inferior notch of the affected side thyroid cartilage to the affected arytenoid cartilage was 16.7 mm.
Conclusion
By understanding the positional relationship between the thyroid cartilage plate and internal structure from preoperative CT images, more effective surgery can be performed according to individual differences.
Level of Evidence
IV Laryngoscope, 134:4088–4094, 2024
INTRODUCTION
Laryngeal framework surgery was devised and systematized by Isshiki et al.1 This surgery is not intended to cure diseases but to improve symptoms by manipulating the laryngeal framework cartilage to change the position and tension of the vocal fold for abnormal vocal fold movements caused by disease. Laryngeal framework surgery includes thyroplasty type I (TPI; lateral compression), II (lateral expansion), III (relaxation/shortening), IV (stretching/lengthening), and arytenoid adduction (AA; moved to adduction position and fixed).
TPI surgery is primarily performed to treat vocal fold paralysis; fenestration is performed at the site where the paralyzed vocal fold is projected onto the affected thyroid plate; and medialization is conducted. Figure 1 presents the usual positioning parameters in fenestration and medialization of TPI surgery. AA is also performed for vocal fold paralysis, similar to TPI, especially for cases of severe breathy hoarseness.2
In our hospital, computed tomography (CT) evaluation is performed before surgery to ensure effective and smooth surgeries. CT images are obtained under two conditions: during quiet breathing and vocalization, with the patient in the supine position. Multi-planar reconstruction (MPR) images with 1.0 mm slices were reconstructed from the original scans. The shape and degree of ossification of the thyroid cartilage, degree of vocal fold atrophy, position where the anterior commissure attached to the thyroid cartilage, and position of the arytenoid cartilage are confirmed. In addition, CT examinations are performed when it is necessary to confirm the position and condition of the implant placements after surgery.
However, I have encountered multiple cases in which the paralyzed vocal fold and implants were not in a parallel relationship on postoperative CT, despite thyroid cartilage fenestration and implant placement using the standard method previously described. Therefore, in this study, I examined the positional relationship between the thyroid plate on the affected side and the internal structures using CT conducted before and after surgery.
MATERIALS AND METHODS
This study was approved by the Ethics Committee of Toho University Medical Center Omori Hospital (M23146) and conducted in accordance with the 1964 Helsinki Declaration and its later amendments. In this study, the research information was publicly available on a website, with the opportunity to opt out.
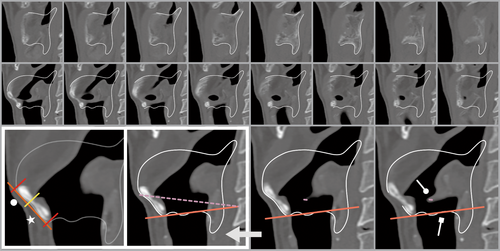
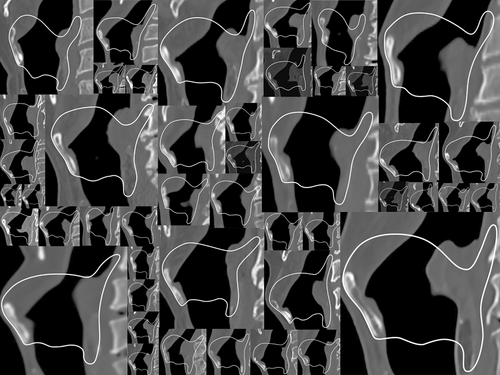
Between 2014 and 2022, Omori Hospital staff operated on 138 patients with unilateral vocal fold paralysis. Among them, the 46 participants of this study were those with thyroid cartilage ossification observed in preoperative CT examinations with an identified paralyzed vocal fold. Participant inclusion was determined by a CT value of 500 for the window level and 2000 for the window width. Using Adobe Illustrator® (Adobe Inc, San Jose, California, USA), the thyroid plate on the affected side was reconstructed from continuous images from the sagittal section of the CT examination during the quiet breathing of the participant (Fig. 2).
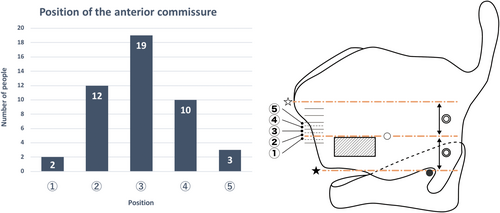
-
Height of the anterior commissure in the midline thyroid cartilage (preoperative sagittal CT under quiet breathing condition)
First, a tangential line was drawn at the midline of the thyroid cartilage. Second, a line was drawn perpendicular to the tangential line passing through the upper and lower ends of the thyroid cartilage and the upper surface of the anterior commissure. Then, the distance from the top and bottom ends of the thyroid cartilage to the vocal fold was measured and the ratio was calculated (Fig. 2).
-
Angle of the paralyzed vocal fold projected onto the affected thyroid plate (preoperative sagittal CT under quiet breathing condition)
From the MPR image, the vocal process tip position was identified, and a line connecting the anterior commissure was drawn (Supplemental Video S1). Then, the angle between the line of the paralyzed vocal fold and the line connecting the lower end of the median thyroid cartilage and the inferior notch (baseline) was determined. Furthermore, the results from the aerodynamic testing of the patients were evaluated as an indicator of the severity of vocal fold paralysis.
-
Angle of the unaffected vocal fold projected onto the affected thyroid plate (preoperative sagittal CT of vocalization condition)
These participants had the RATP shape under vocalization conditions consistent with the RATP shape under quiet breathing conditions. From the MPR image, the position of the vocal process tip was identified, and a line connecting the anterior commissure was drawn. The angle between the line of the unaffected vocal fold and baseline was determined.
-
Angle of postoperative paralyzed vocal fold projected onto affected thyroid plate (postoperative sagittal CT under quiet breathing condition)
Among the participants in [3], those whose RATP shape during quiet breathing on postoperative CT matched that of RATP during quiet breathing on preoperative CT were targeted. From the MPR images, the positions of the tips of the vocal processes were identified, and a line connecting the anterior commissure was drawn. Then, the angle between the postoperative paralyzed vocal fold line and the baseline was determined.
-
Distance from the inferior notch of the affected thyroid cartilage to the arytenoid cartilage of the paralyzed vocal fold (preoperative sagittal CT under quiet breathing condition)
The participants from [1, 2] were targeted. However, those in which the lateral lower part of the arytenoid cartilage was not ossified and the cricoarytenoid articular surface was not exposed were excluded.
Statistical Analyses
The averages and standard deviations were calculated from the angles and distances obtained in each study. The Wilcoxon signed-rank test was used for statistical analyses between groups. Statistical significance was set at p < 0.05.
RESULTS
-
Height of the anterior commissure in the midline thyroid cartilage (preoperative sagittal CT under quiet breathing condition)
A total of 46 cases were included. The median part of the thyroid cartilage was divided into 20 equal parts, the anterior commissure was examined to determine which parts, and 5 parts were found, as shown in Figure 1. The largest number of patients were categorized in position ③, which was slightly higher than the centerline of the upper and lower ends of the thyroid cartilage, and a normal distribution centered on position ③ was observed. The anterior commissure was present at an average distance of 57% from the lower end of the midline of the thyroid cartilage toward the superior notch (shortest: 48%; longest: 65%).
-
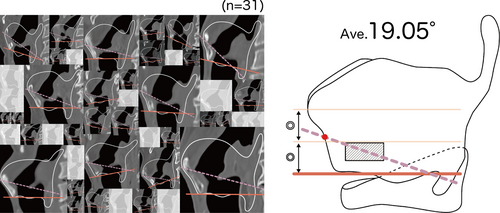
Angle of the paralyzed vocal fold projected onto the affected thyroid plate (preoperative sagittal CT under quiet breathing condition)
Of the 46 cases, 31 had the RATP shape in the vocalization condition consistent with the RATP in the quiet breathing condition were included. Preoperative aerodynamic testing was conducted on 29 of the 31 patients included in the study. The average maximum phonation time was 3.2 s, with a mean airflow rate of 957 ml/s. The average angle between the paralyzed vocal fold line and the baseline was 19.05° (Fig. 4).
-
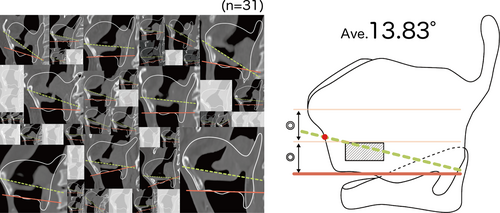
Angle of the unaffected vocal fold projected onto the affected thyroid plate (preoperative sagittal CT of vocalization condition)
The 31 patients as described in [2] were included. The average angle between the line of the unaffected vocal fold and baseline was 13.83° (Fig. 5). In a comparison of the same 31 cases, a significant difference was observed for the angle of the paralyzed vocal folds in [2].
-
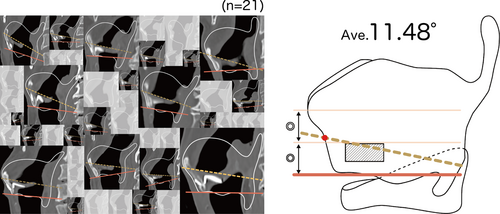
Angle of postoperative paralyzed vocal fold projected onto affected thyroid plate (postoperative sagittal CT under quiet breathing condition)
Of the 46 participants, 21 had their preoperative RATP shape matched the postoperative RATP shape when CT was performed postoperatively. The average angle between the paralyzed vocal fold line and the baseline was 11.48° (Fig. 6). In a comparison of these same 21 cases, a significant difference was observed for the angle of the paralyzed vocal fold in [2]. However, no significant difference was observed in comparison with the angles of the unaffected vocal folds [3] (Fig. 7). Postoperative voice was not evaluated in this study, as it is influenced not only by the angle but also by TPI. However, the postoperative voice of some patients in this study has been described in a previously published article by the author.3
-
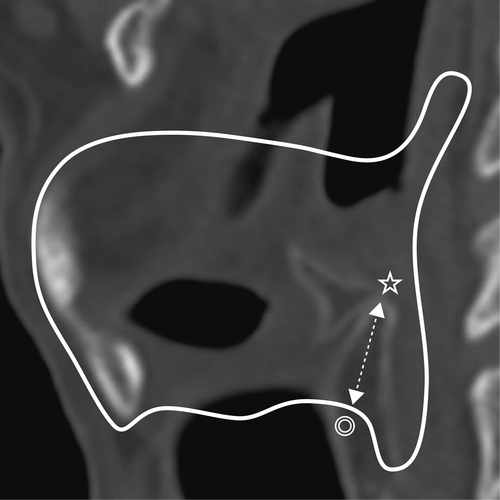
Distance from the inferior notch of the affected thyroid cartilage to the arytenoid cartilage of the paralyzed vocal fold (preoperative sagittal CT under quiet breathing condition)
Of the 46 patients, the 33 with ossification of the lateral lower part of the arytenoid cartilage, with the cricoarytenoid articular surface observable, were included. The shortest average distance from the inferior notch of the affected side to the arytenoid cartilage of the paralyzed vocal fold was 16.7 mm (Fig. 8).

DISCUSSION
Since Payr's report,7 various techniques and implants have been used in vocal fold medialization surgery. Isshiki et al.1 systematized and reported on the surgical procedure for dysphonia as laryngeal framework surgery. TPI corresponds to the medialization of vocal fold. To obtain a good voice, it is necessary to perform fenestration of the thyroid cartilage that matches the position of the paralyzed vocal fold during surgery.
Position and Angle of the Vocal Fold
Until now, the position of the vocal folds projected onto the thyroid plate has been determined based on anatomical indices. Payr7 reported that the line parallel to the horizontal through the midpoint of the thyroid cartilage is used as the position of the vocal fold for medialization. Isshiki8 reported the line that passes through the midpoint of the thyroid cartilage midline and is parallel to the line connecting the lower end of the midline of the thyroid cartilage and the inferior notch should be used as the position of the paralyzed vocal fold for medialization. Similar indices are used to determine the fenestration of previously developed implant systems. In the APrevent® VOIS implant system reported by Ho et al.9 surgery is performed assuming that the line that passes through the midpoint of the thyroid cartilage midline and is parallel to the line that connects the anterior and posterior parts of the inferior thyroid tubercle is used as the position of the paralyzed vocal fold for medialization.
Regarding the position of the anterior commissure during surgery, all reports have used the midpoint of the thyroid cartilage midline. However, individual differences in the examination of Japanese cadavers have been reported.10 In the present study, the anterior commissure was located slightly above the midpoint of the thyroid cartilage midline. Considering that the median distance of the thyroid cartilage in adult Japanese males is 18 mm,10 the anterior commissure is located at an average position of 10.26 mm from the lower end of the midline thyroid cartilage. However, the measurement results had a normal distribution, with the shortest distance of 8.64 mm and the longest distance of 11.7 mm, a difference of approximately 3 mm. It is suggested that this 3 mm difference greatly affects surgical outcomes.
Previous cadaver dissection studies have reported that the angle of the paralyzed vocal fold is horizontal or parallel to the baseline. However, in the present study, by using CT images, an average inclination of 19.05° was observed relative to baseline. The cause is presumed to be the difference between a cadaver and a living body; however, this angle difference has a significant impact on surgery. This is because most implants that have been developed thus far are shaped to fit into the fenestration of the thyroid cartilage, and the angle of medialization is defined by the angle of fenestration. This difference in angle causes the implant to push the back of the vocal fold cranially. This situation reduces the voice improvement effect and becomes a risk factor for exposing the implant to the airway. If fenestration can be performed according to the inclination of the paralyzed vocal fold, this problem can be solved. However, tilting in fenestration may be difficult because the inferior border of the thyroid cartilage is just below the fenestration. If only TPI is performed, the arytenoid cartilage remains unfixed. Therefore, performing fenestration near the lower border of the thyroid cartilage reduces the risk of exposing the posterior part of the implant, since the implant will elevate the vocal fold process. However, if AA is also performed, the arytenoid cartilage is stabilized, increasing the risk of implant exposure due to a mismatch between the angle of the vocal fold and the implant placement angle. Therefore, when AA surgery is performed, particular attention to the angle is necessary.
In this study, the postoperative angle of adduction of the vocal fold was smaller than that of pre-surgery, which contrasts with the expected outcome of normal adduction movement.11 This indicates that the AA technique does not replicate physiological adduction motion. The cricoid cartilage, which gradually increases in height from the ventral to the dorsal side, and the cricoarytenoid capsular along with the attached posterior cricoarytenoid ligament, limits the range of motion of the arytenoid cartilage. It is anticipated that the traction effect of the adductor thread, in conjunction with the action of the arytenoid muscle, also innervated by the recurrent laryngeal nerve on the unaffected side, produces a rotational and sliding motion, resulting in the movement toward the physiological direction of adduction (the angle is decreased).
The angle of the unaffected vocal fold during vocalization was significantly smaller than that of the affected vocal fold; however, there was no significant difference in the paralyzed vocal fold after AA. This indicated that the position of the vocal fold after adduction could be estimated using preoperative CT. AA is a powerful voice-improving procedure. If the direction of TPI medialization, which is often performed together with the AA, is known, voice improvement is expected to be further enhanced.
In this study, a RATP was developed to gain a deeper understanding; however, implementing RATP in actual clinical settings is impractical due to its time-consuming nature and high risk of errors. Instead, visualizing the lower end of the median thyroid cartilage, the inferior notch, and the angle of the vocal folds is comparatively straightforward. Understanding the relationship among these three anatomical landmarks would enable surgeons to effectively account for individual differences.
Arytenoid Cartilage Position
When AA was first performed, a method for identifying the arytenoid cartilage was proposed based on anatomical studies.12, 13 To identify the arytenoid cartilage based on anatomical landmarks, it is necessary to remove the external laryngeal muscle and expose the thyroid cartilage plate. However, the external laryngeal muscles, pharyngeal constrictor muscles, external branch of the superior laryngeal nerve, and cricothyroid muscle function are auxiliary and compensatory for paralyzed vocal folds, whose function is reduced because of damage to the recurrent laryngeal nerve.14 Therefore, procedures that damage these muscles and impair laryngeal function should be avoided. The position of the dorsal end of the thyroid cartilage to be fenestrated to identify and manipulate the arytenoid cartilage can be determined during surgery by measurements taken before surgery of the distance from the inferior notch to the arytenoid cartilage. The adductor thread can be attached to the arytenoid cartilage with minimal sublation and fenestration, without excision of the pharyngeal constrictor muscle or the external branch of the superior laryngeal nerve. This makes it possible to improve voice while preserving laryngeal function. This procedure has been reported as the all-muscles preserved method.5
Since this study did not target female patients with a weak ossification tendency, the findings obtained are limited to male patients. In the future, it will be necessary to investigate a method that can indicate female thyroid cartilage and examine the condition of the paralyzed vocal fold. Moreover, if the reconstruction technology applied to original images becomes as standardized in MRI examinations as it is in CT examinations, it will then be possible to evaluate the larynx in females as well.
CONCLUSION
The position and angle of the paralyzed vocal fold projected onto the thyroid cartilage plate and the position of the arytenoid cartilage were examined from CT images obtained before and after surgery. The anterior commissure was positioned slightly cranial to the midpoint of the thyroid cartilage midline. The angle of the paralyzed vocal fold was not parallel to the previously reported baseline but at an angle of approximately 20°. To perform more effective medialization according to individual differences, it is necessary to understand the positional relationship between the thyroid plate and internal structure. In addition, it has been suggested that existing implants for medialization, which are defined by the angle of fenestration, cannot cope with this inclination. In other words, by developing an implant that can accommodate this inclination, greater voice improvement effects could be achieved more than ever before. During AA, the impact on muscles and nerves can be minimized by approaching the arytenoid cartilage based on the distance from the inferior notch of the thyroid cartilage to the arytenoid cartilage.
ACKNOWLEDGMENTS
I would like to express my sincere gratitude to my advisor and mentor, Professor Nobuhiko Isshiki.




