Intra-articular pressure characteristics of the knee joint: An exploratory study
Abstract
Inflammation-predominant osteoarthritis is an important clinical type of osteoarthritis, with synovitis suggested as its distinct pathophysiology. We investigated whether the synovium's mechanical properties in knees differed by osteoarthritis and other clinical parameters through retrospectively analyzing intra-articular pressure–volume characteristics. We analyzed 60 knees that were administered intra-articular corticosteroids while undergoing pressure monitoring. McMurray's test, pain complaints at end-range knee flexion, Kellgren–Lawrence classification from standing anteroposterior radiographs, and suprapatellar effusion from ultrasound constituted clinical parameters. Pressure–volume profiles—phasic changes in pressure by volume infusion, the volume of Phase 1—the potential volume of the synovial space, the pressure at 45 ml infusion—intra-articular pressure at a standardized volume, and the slope of Phase 2—synovial stiffness were compared with clinical parameters. All graphs were biphasic. Knees with suprapatellar effusion or radiologically definite osteoarthritis (Kellgren–Lawrence grade ≥2), had a lower Phase 1 volume. Knees with definite radiographic osteoarthritis also showed higher pressures at 45 ml and Phase 2 slopes (171.11 ± 94.35 mmHg and 5.08 ± 3.07 mmHg/ml, respectively) than those without (101.88 ± 58.12 mmHg and 2.84 ± 1.27 mmHg/ml, respectively). The Phase 2 slope was higher for knees with positive provocative tests than in those with negative provocative tests, although not statistically significant. The synovium stretched earlier in knees with effusion or radiologically definite osteoarthritis. Intra-articular pressure and synovial stiffness were significantly higher in patients with radiologically definite osteoarthritis. The synovium's mechanical characteristics are altered by osteoarthritis of the knee joint. Intra-articular pressure characteristics could be utilized for synovial evaluation clinically.
1 INTRODUCTION
Intra-articular fluid dynamics interacting with the viscoelastic tissue inside the knees changes every moment in response to various external stimuli in our daily lives. The viscoelastic properties of synovial membrane and fluid play an important role in shock absorption and lubrication.1 However, the inner structures of the knee that have been used throughout one's life are likely to get damaged someday, and various damages are inevitably accompanied by inflammation and fluid accumulation, which could affect the intra-articular rheology. Moderate to large effusion was previously reported in 56% of elderly patients with painful radiographic knee osteoarthritis (OA), but in only 15.6% of those without pain.2
Knee OA is a major cause of activity limitation, physical disability, excessive medical use, and poor quality of life.3 Formerly, physicians focused on evaluating structural damages such as cartilage, subchondral bone, meniscus, and other mechanical weight-bearing soft tissues. Recently, the inflammation-predominant OA has been recognized as an important clinical type of OA.4-7 Osteoarthritic synovitis found early in OA, and has been suggested as a cause of pain, structural damage,6 and progression7 of OA. Although the histologic changes of the synovium and proinflammatory role of synovitis have been known well,6, 8, 9 the pathogenesis from synovitis to certain disease patterns is still obscure and difficult to investigate. In early synovitis, synovial membrane is not easily detected because the cell layer is extremely thin,10 and even in later phase, it is difficult to quantitatively measure and conclude the roles of synovitis, because of various diagnostic methods. For example, the previous study on contrast-enhanced magnetic resonance imaging (MRI) of OA knees revealed more thickened synovium, which seemed to be a simple effusion on fluid-sensitive MRI sequence.11
Few previous studies have reported changes in the physical properties of synovium. Increased stiffness of the synovial membrane has been reported in patients with RA and in patients with painful stiff shoulder,12, 13 and reduced elasticity was observed in the animal OA knee model.14 The physical change of the synovium could be explored by observing the viscoelastic properties of synovial tissue, such as other biologic soft tissues in the body, for example, tendons and ligaments.15 Viscoelastic properties refer to time-dependent mechanical behavior and show nonlinear elasticity. That is, the stress response to a constant increase in strain is nonlinear. As the strain increases, the increase in stress is initially nonlinear, which is called the toe region. After passing through the toe region, it shows linear increase, and finally, tissue failure occurs beyond physiologic limits, again showing a nonlinear pattern.15-17
To the knowledge of the authors, no studies have reported the physical properties of the synovial membrane of painful knee joints in vivo. In this study, the intra-articular pressure data of patients who underwent intra-articular injection into knee joint using hydraulic distension (HD) device were retrospectively investigated. And the objective of this study was to investigate the difference of synovium's viscoelastic properties within painful knee joints regarding OA and different clinical situations.
2 METHODS
This study is a retrospective cohort study with Level 3 evidence.
2.1 Patients
We reviewed outpatient records from January 2016 to December 2018 and included the patients who underwent intra-articular corticosteroid injection in a large-volume injectate with pressure monitoring under constant volume infusion, and whose pressure–time (PT) data were recorded in the storage of the HD machine. A large-volume corticosteroid injection in the knee was administered in cases of diffuse knee joint pain continuing > 6 weeks despite noninvasive conservative treatments. Patients who diagnosed with inflammatory arthritis (rheumatoid arthritis, psoriatic arthritis, reactive arthritis, and crystal-induced arthritis) and recent trauma were excluded. Patients were also excluded if their PT curves were impossible to analyze (e.g., considerable noise due to needle manipulation, joint motion, muscle contraction, or any other technical errors from HD machines or physicians). Finally, 60 painful knee joints from 58 subjects (69.57 ± 8.97 years old) were included. This study was approved by the Institutional Review Board of Seoul National University Hospital and was performed in accordance with the guidelines of the Helsinki Declaration. Informed consent was waived because the data were deidentified, and the study design was retrospective.
2.2 Clinical parameters
Demographic data, including age, sex, height, weight, and the results of McMurray's test and pain complaints at end-range flexion, were obtained from electronic medical records. All patients live in Korea. The patients were assigned a Kellgren–Lawrence (KL) grade using the results of standing anteroposterior radiographs by a physiatrist with more than 5 years of musculoskeletal practice who was blinded to the patients' intra-articular pressure characteristics and clinical information. To divide the OA severity into definite or indefinite, KL Grade 2 and higher was defined as definite OA. The existence of suprapatellar effusion was determined during ultrasound-guided needle placement for HD, as described in the following section (Table 1).
| Age | 69.57 ± 8.97 |
| Sex (%) | |
| Female | 57 (95.00) |
| Male | 3 (5.00) |
| Height | 155.23 ± 6.28 |
| Weight | 60.08 ± 7.41 |
| End-range flexion pain (%) | |
| Negative | 33 (55.00) |
| Positive | 27 (45.00) |
| Mcmurray's test (%) | |
| Negative | 44 (73.33) |
| Positive | 16 (26.67) |
| Existence of suprapatellar effusion (%) | |
| Absent | 16 (26.67) |
| Present | 44 (73.33) |
| Kellgren–Lawrence grade (%) | |
| <2 | 16 (27.12) |
| ≥2 | 43 (72.88) |
| Pressure parametersa | |
| Vph1 (ml) | 5.57 [2.93, 12.20] |
| P45 (mmHg) | 131.81 [87.56, 206.02] |
| Sph2 (mmHg/ml) | 3.77 [2.69, 5.71] |
- Note: Normally distributed continuous variables are summarized with mean ± SD, nonnormally distributed continuous variables are summarized with median [interquartile range], and categorical variables are summarized as percentages.
- a The volume of phase 1 (Vph1), the volume of potential synovial space; pressure at 45 ml infusion (P45), intra-articular pressure at a standardized volume; and the slope of phase 2 (Sph2), synovial stiffness.
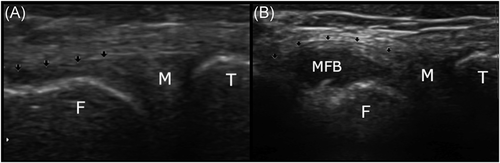
2.3 Ultrasound-guided intra-articular placement of the needle
The patient's knee HD position was supine with the popliteal fossa resting on the pillow with an angle of 75° at the top edge. While the patient was asked to relax the lower extremity as much as possible, a 13 MHz linear ultrasound probe (Accuvix V20; Medison) was spread with coupling gel and placed on the upper lateral part of the patella in the axial orientation to the femur (Figure 1A). We identified the suprapatellar synovial recess as a hypoechoic space by sliding the probe in the cephalic direction, which lies deep to the quadriceps tendon and suprapatellar fat pad and superficial to the prefemoral fat pad (Figure 1C). We determined that effusion was present if the longest anteroposterior diameter of the hypoechoic space in the mid-sagittal plane of the suprapatellar recess was longer than 4 mm.18 With the probe positioned over the suprapatellar recess, the redundant coupling gel around the probe was wiped off, and the skin area lateral to the probe was thoroughly disinfected with betadine balls. Without moving the probe, the needle was introduced into the synovial space by piercing the skin at a point that was at least 5 mm from the lateral edge of the probe to maintain a strict aseptic condition. The direction of needle advancement was in a plane with the sonographic view so that the whole needle tip and shaft could be visualized at any time during the procedure. After confirming that the needle's tip was in the recess without touching the deep or superficial fat pad, the infusion was started with a provider experienced in musculoskeletal ultrasound over 20 years.
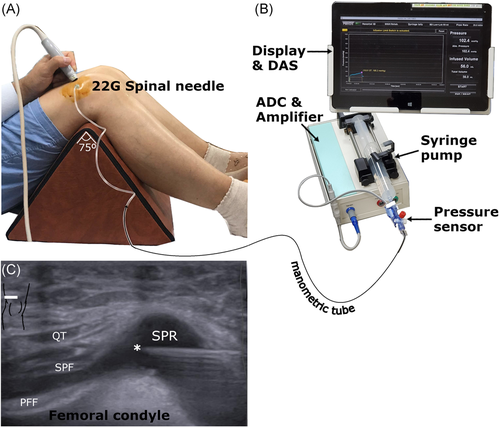
2.4 HD procedure
Since the knee joint has a larger synovial cavity than the other major joints in our body, we injected a larger corticosteroid mixture volume into the knee joint with synovial inflammation. To inject a large volume without imposing excessive strain on the administrators hands, we adopted a HD device that was originally developed to distend painful stiff shoulder joints.12, 19-23 The device provided not only convenience during the injection procedure but also recorded pressure and volume data, which could be processed afterward.
A disposable flow-through pressure sensor (AMK 150; Acemedical) with two tube ends was installed between a needle and syringe. The caudal end was attached to a 50-ml disposable syringe mounted on a syringe pump (NE-500; New Era Pump Systems), which was controlled at a preset constant volume speed of 20 ml/min. The cephalic end was connected to a 22-gauge spinal needle via manometric tubes with a 1.5 mm inner diameter. All connections were secured with Luer locks. The analog pressure signals were amplified using an amplifier (STT-200S-01; CAS), digitalized by an analog-to-digital converter with a sampling rate of 10 Hz, and stored in a local memory disc with a data acquisition system (DAQ, NI USB-6259, NI) (Figure 1B).
A fluid mixture with a total volume of 57 ml, comprising 10 ml of 1% lidocaine, 1 ml of 40 mg triamcinolone, and normal saline, was prepared in a 50-ml disposable syringe. Approximately 5 ml of the injectate filled both the tubes and the sensor of the HD device by manually flushing out immediately before the needle was attached. Fluid infusion was initiated immediately after the successful placement of the needle's tip into the suprapatellar synovial space and continued until all the prepared injectate was infused. Two premature termination criteria were set up for safety purposes: (i) if a sign of impending rupture was noted in the PT curve or a cessation of pressure increase,23 and (ii) if the patient wanted to stop due to pain, discomfort, or other reasons.
2.5 Postprocessing of pressure-volume data
The intra-articular PT data were converted into pressure–volume (PV) curves by multiplying the time by constant volume speed (20 ml/min). The PV curves were divided into two phases: the initial flat phase and continuous pressure increase. To decompose the graph, we identified three pressure points—the initial point at the beginning of the infusion representing baseline intra-articular pressure, the second point between the first and second phases, and third at the end of the second phase. The volume of Phase 1 (Vph1), which reflects the onset volume of synovial strain, was measured between the first and second pressure points (Supporting Information Figure). To compare intra-articular pressure at a standardized volume, the pressure at the 45 ml infusion (P45) was sampled. P45 was chosen to sample the intra-articular pressure at the largest volume for all the tested knees. As this study's PV profiles were analogous to the stress–strain curve for viscoelastic biologic tissues,15-17 the Phase 2 slope (Sph2), reflecting synovial stiffness, was approximated using linear regression from all data points on Phase 2 of the curve after eliminating noise (A-2, B-2, and C-2 in Supporting Information Figure). Finally, Vph1, P45, and Sph2 were determined as the pressure parameters representing physical properties of knee synovium.
2.6 Statistical analysis
To evaluate the physical properties of knee synovium, pressure parameters (Vph1, P45, and Sph2) according to clinical parameters (McMurray's test, pain complaints at end range flexion, KL grade, predisposing suprapatellar effusion) were analyzed with the Wilcoxon signed-rank test with a significance of p < 0.05. To adjust for baseline imbalance between groups, we proceeded with a multivariable analysis using generalized linear (GLM) model with gamma identity link function. The demographic and clinical parameters were used as covariates and magnitude of effects were reported with the effect size based on estimate of GLM. All statistical analyses were performed using R Statistical software version 3.5.3 (Foundation for Statistical Computing).
3 RESULTS
The mean age of 58 patients were 69.57 ± 8.97 and 55 patients among them were women. Forty-three patients have radiographic definite OA (Table 1).
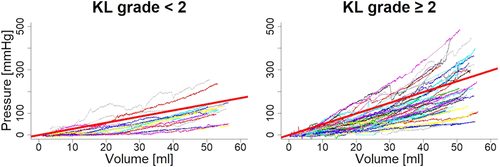
3.1 PV profiles
All procedures were terminated after injecting the total prepared volume; none were prematurely terminated due to emerging pending rupture signs or patient requests. The graphs created from the variables from all the knee joints were biphasic; initial flat and second steep phases. When the initial flat phase was terminated; the second appeared at an infusion volume of 8.38 ± 7.75 ml. The second phase's slope steepness was 4.45 ± 2.85 mmHg/ml, which was maintained until the end of the volume infusion with an average ending pressure of 195.82 ± 109.48 mmHg and an average ending volume of 51.88 ± 3.44 ml.
3.2 PV parameters versus predisposing effusion on ultrasonography
Among the PV parameters, only Vph1 was significantly less with suprapatellar effusion. Vph1 was 6.83 ± 6.45 ml in effused knees, while it was 12.61 ± 9.53 ml when effusion was absent (effect size = −5.97 ± 2.20, p = 0.009) (Table 2). P45 was higher in effused knees (164.34 ± 95.23 mmHg), compared with that of noneffused knees (113.87 ± 65.26 mmHg), but the difference was not statistically significant (Table 2). Sph2 was also higher in knees with effusion (4.66 ± 3.10 mmHg/ml) than in knees without effusion (3.87 ± 2.00 mmHg/ml), with no statistical significance (Table 2).
| Vph1 (ml) | P45 (mmHg) | Sph2 (mmHg/ml) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Parameters | Est | SE | p | Est | SE | p | Est | SE | p |
| Demographic covariates | |||||||||
| Age | 0.000 | 0.060 | 0.998 | −2.888 | 1.192 | 0.020* | −0.066 | 0.032 | 0.045* |
| Sex | −2.371 | 5.236 | 0.653 | −47.813 | 26.944 | 0.083 | −0.962 | 0.812 | 0.242 |
| BMI | −0.096 | 0.209 | 0.649 | −0.814 | 4.376 | 0.853 | −0.016 | 0.118 | 0.893 |
| Clinical parameters | |||||||||
| Mcmurray's test | 0.730 | 1.538 | 0.637 | 17.196 | 26.766 | 0.524 | 0.760 | 0.815 | 0.356 |
| End-range flexion pain | 1.124 | 1.187 | 0.349 | 11.586 | 21.067 | 0.585 | 1.182 | 0.617 | 0.061 |
| KL grade | −8.332 | 2.608 | 0.003* | 52.847 | 22.961 | 0.026* | 1.603 | 0.577 | 0.008* |
| USG effusion | −5.972 | 2.198 | 0.009* | 40.159 | 19.987 | 0.051 | 0.530 | 0.595 | 0.378 |
- Abbreviations: Est, estimate; KL, Kellgren–Lawrence; p, p value; P45, pressure at 45 ml infusion; SE, standard error; Sph2, the slope of Phase 2; USG, ultrasonographic; Vph1, the volume of Phase 1.
- * p < 0.05.
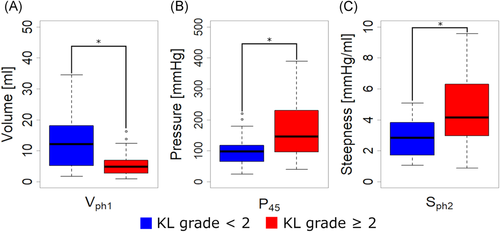
3.3 PV parameters versus radiographic OA severity
Vph1 was 6.15 ± 5.46 and 13.50 ± 10.09 ml in knees classified as KL grade ≥2 and <2, respectively (effect size = −8.33 ± 2.61, p = 0.003) (Table 2). Sph2 was significantly higher in knees classified as KL grade ≥2, which was 5.08 ± 3.07 mmHg/ml, compared with 2.84 ± 1.27 mmHg/ml in knees with a KL grade <2 (effect size = 1.6 ± 0.6, p = 0.008) (Table 2, and Figures 2 and 3). P45 was also significantly higher in knees with a KL grade ≥2, which was 171.11 ± 94.35 mmHg, compared with 101.88 ± 58.12 mmHg in knees with a KL grade <2 (effect size = 52.85 ± 22.96, p = 0.026) (Table 2, and Figures 2 and 3).
3.4 PV parameters versus provocative physical examination
Vph1 was lower and P45 and Sph2 were higher at patients who complaint end-range flexion pain (9.41 ± 8.69 ml 169.05 ± 97.95 mmHg, and 5.19 ± 3.10 mmHg/ml, respectively) than in those without pain (7.49 ± 6.85 ml, 133.34 ± 80.74 mmHg, and 3.85 ± 2.53 mmHg/ml, respectively), but this difference was not statistically significant according to the results of GLM analysis (Table 2). Patients who obtained positive McMurray's test results (4.97 ± 3.50 mmHg/ml) had higher Sph2 values than those with negative results (4.26 ± 2.60 mmHg/ml), however, the difference was not statistically significant (Table 2).
4 DISCUSSION
The PV data of the 60 painful knees using the HD device were explored to determine whether the PV parameters changed in different clinical conditions. All PV graphs were biphasic, and the initial filling phase was shorter when predisposing suprapatellar effusion or radiologically definite OA was present. Radiologically definite OA showed statistically significant differences in other pressure parameters, namely higher intra-articular pressures and steeper slopes of the second elastic phases. Patients reporting pain at end range flexion showed similar intra-articular pressure characteristics to those with radiologically definite OA; however, this difference was not statistically significant.
4.1 Biomechanical considerations of PV profiles
Typical parameters describing the biomechanical properties of soft tissue are strain, stress, and stiffness, and the quality of the tissue substance are represented by a stress–strain curve.15 Viscoelastic soft tissue has typical triphasic stress–strain curve, which phases are toe region, linear region, and failure region, and we previously observed the typical triphasic PV curve patterns at the painful stiff shoulder joints.12, 19-23 The toe region represents the uncrimping of the synovium, and failure region represent an impending rupture before tissue failure. These phases are nonlinear fashion. In shoulder joints, the typical third phase of PV curve are observed before tissue failure, which mean capsule-rupturing HD.20, 21 In contrast to typical triphasic curves, all PV curves from the painful knees included in this study had biphasic profiles and none were monophasic or triphasic. The authors speculated that the infused volume, 51.88 ± 3.44 ml, was enough to fill up the entire potential space of the knee joint and uncrimped the synovium, because all the profiles passed through the toe region and reached the second phase, but it was not enough to distend the joint further and thereby cause tissue failure because none of the PV curves proceeded into the third phase.
The knee joint is the largest synovial joint in the human body, with the volume reportedly averaging 99 ml at a pressure of 50 mmHg during the arthroscopic procedure.25 Another study reported an average volume of 130 ml at 200 mmHg in advanced OA.26 In this study, we initially decided to stop the procedure if pending rupture signs or pain complaints emerged, but the average injected volume was much less (approximately 52 ml) than normal joint volume, and the knee was in its resting state without muscle contraction, so the synovium could be preserved without rupture. We observed bulging of the meniscofemoral recess at the medial knee under the deep medial collateral ligament, which are normally closed as potential spaces, so we presumed that the various bursae and recesses in the knee joint27 were stretched at the same time (Figure 4).
4.2 Early strain in the presence of supra-patellar effusion
Vph1, the end volume of Phase 1 of the PV curves, represents the point at which the potential space of a joint is filled up until the toe region appears and significant pressure develops. Steer et al. previously reported the slope changing section, which is toe region, where the elasticity changes during knee joint distension using a dextrose/sodium chloride solution in experimental setup.28 In our study, Vph1, was significantly reduced in knees with effusion (6.15 ± 5.46 ml) compared to those without (13.50 ± 10.09 ml). In Figure S2A, raw data from two contrasting knees demonstrated that knee #27 (with suprapatellar effusion) had a much shorter initial flat phase than that of knee #4 (without suprapatellar effusion) (Figure S2B,C). These findings suggest that there should be more than 13 ml of effusion to develop tension in the knee joint synovial cavity.
4.3 High stiffness of synovium in radiologic definite knee OA
To the best of our knowledge, direct measurement of synovial stiffness of the knee joint has never been performed in clinical settings. Here, it was clearly shown that HD pressure monitoring would provide a novel method to quantify the stiffness of the synovial membranes of the knee joint. The joint capsule is composed of an inner synovial membrane and an outer fibrous membrane, but since the supra-patellar recess of the knee joint consists only of the synovial membrane, the initial expansion would mostly reflect the stiffness of the synovium. The slope of the second phase in the PV curve, Sph2, is the surrogate marker of synovial stiffness because it is an analog of the slope of the linear elastic region in the stress–strain curve of the viscoelastic biological tissue.15-17 In this study, the Sph2 was higher in knees with radiologically definite OA, which was 5.08 mmHg/ml compared with 2.84 mmHg/ml of the non- or possible radiological OA, and it was significant even after considering demographic and clinical covariates. This is similar to the results of previous studies which showed increased synovial stiffness in patients with painful stiff shoulders19 and RA of the knee.13, 29
Measuring the stiffness of knee synovial membranes could have vital implications for the diagnosis of painful knees. In shoulder joints, which aim to perform daily life tasks in a wide range in various directions, early observable range of motion (ROM) disturbances are relatively sensitive tests to detect capsular pathology, especially the dominant limitation of external rotation due to pathologic changes in the coracohumeral ligament. However, the knee joint, which mainly plays a role in weight-bearing and limb stabilization has a simple axis and a narrower ROM than the shoulder. Therefore, knee joint ROM limitation due to stiffened synovium cannot readily be seen until certain pathologies evolve into very advanced stages. Abreu et al. reported adhesive capsulitis of the knee with ROM limitation without definite injury of the intra-articular structures. Although they presented MRI and positron emission tomography/computed tomography images to show extensive inflammation of the synovium,29 complementary use of real-time pressure monitoring HD could have helped to make earlier and more functional diagnoses rather than solely relying on imaging studies because the synovial membrane is extremely thin cell layer.10
4.4 High intra-articular pressure and early strain in radiologic definite knee OA
Tissue material strength with viscoelastic properties can be shown as the maximum load achieved, but since this means the synovial rupture, it is ethically inappropriate. Instead, the maximum infusion volume observed in all subjects was 45 ml, so the intra-articular pressure in that volume, P45, was compared. The P45 value was notably higher in patients with radiologically defined knee OA in the resting state. These results indicate that a knee joint with more degeneration may have increased stiffness in the synovial membrane (higher slope of Phase 2), predisposing effusions (shorter length of Phase 1), and/or less volumetric capacity. Because high Sph2 and reduced Vph1 were observed in radiologically definite OA.
4.5 Significance of exploring synovial physical properties
Recently, attempts have been made to classify both the heterogeneous pathology and multifactorial nature of OA into phenotypes based on underlying causes and mechanisms driving joint damage, which were frequently classified into bone and cartilage metabolism, metabolic syndrome, malaligned biomechanical, chronic pain, and inflammatory predominant types.5, 30 Synovitis, accompanied by synovial proliferation, angiogenesis, and neurogenesis, is suggested as the cause of pain and structural damage in OA.6, 7, 31-33 Sarmanova et al. reported that ultrasound detection of effusion and synovial hypertrophy is more common in painful knee OA, and it is related to OA structural changes rather than pain.31 Burke et al. reported that higher 18F-fluorodeoxyglucose uptake within the suprapatellar region in symptomatic knees compared with asymptomatic knees and higher fluorodeoxyglucose avidity are associated with cartilage loss and a higher degree of synovitis on MRI but not with bone marrow edema lesion.32 Another ultrasound study found that meniscal protrusion was present in most asymptomatic patients; however, a hypertrophied synovium and suprapatellar effusion are associated with knee pain, even in patients with bilateral equal KL grades.33 The pathologic changes of the structures around the synovial recess of OA knees have also been reported. Atrophy and dysfunction of the articularis genu muscle, which holds and pulls the suprapatellar recess, have been reported,34 along with the formation of a synovial pannus, which covers and restricts the meniscus, have also been reported in OA patients.35-37
Although many reports revealed synovial inflammation in knee OA, the joint capsule and synovium's physical properties have been reported to a lesser extent. Lower elasticity and less compliance were observed in animal study and small case-reports.14, 29, 38 These synovial physical changes, mainly increased stiffness, could be precisely detected by the current technique utilizing pressure monitoring with constant volume infusion. Therefore, controlling the inflamed synovial membrane could be one of the main strategies not only in reducing inflammatory pain but in treating the rigid and thickened synovium. Presently, treatment options for knee OA have shown limited effects, and many patients eventually require replacement surgery. Conversely, physicians have evaluated the OA knee by observing structural damages and biomechanical approaches such as compressive overload, malalignment, and instability. However, we have not yet paid close attention to the intra-articular rheological profiles, but it could have some value in improving the understanding of the ambiguous pathophysiology of painful OA. In addition to adjusting patients' physical activity levels and modifying their lifestyle choices, meticulously treating pathologic synovium may be a more effective treatment option.
In this study, we observed stiffness of the synovium in painful, radiologically defined knee OA. Whether the high stiffness of synovium is a simple result, or a cause of OA is uncertain. Various degrees of OA could be revealed in the future through longitudinal observation or careful research. Nevertheless, synovitis deserves to be another target for challenging OA treatment.
4.6 Limitations
Because this study is a retrospective review, it has some limitations, but these results are indispensable for future prospective studies. First, the authors did not fill the knee joint enough to observe the tissue failure of the synovium. This is an inevitable limitation because this was not an experimental setup. Second, we did not quantify the actual joint size and the amount of pre-existing effusion except for the supra-patellar recess. Therefore, constant speed volume injection, could not be the exact same strain per time. However, the difference could be minimal, because although Vph1 was smaller about 6 ml in predisposing effusion group, they still show biphasic PV curve. That means they had residual space to fill up and uncrimped synovium, therefore intra-articular space is not in excessively prestretched, such as a joint that acutely expanded due to recent trauma or inflammatory arthritis. So, driving the synovial stiffness from the slope of PV curve and compare it could be appropriate. Furthermore, the results are statistically significant after adjusting demographics. The volume of the knee joint was found to be dependent on height.26 Third, we did not use an electromyographic sensor or goniometer; thus, we could not confirm that the knee joint angles and muscle activation were the same between patients. Still, we observed a graph that shows noise such as an abrupt decrease or increase in the pressure and removed it, so the influence of episodic joint movement or muscular contractions could be eliminated to some extent. Finally, other types of chronic inflammatory arthritis could not be completely excluded. Although radiographically definite OA group in this study satisfy the ACR' clinical and radiographic criteria of idiopathic knee OA,39 and we excluded other inflammatory arthritis, it can be interpreted as a result for all painful knee conditions.
5 CONCLUSION
In conclusion, synovial strain was observed early in knee joints with effusion or definite radiographic OA. Synovial stiffness and intra-articular pressure of the knee joint were significantly higher in patients with radiologically definite OA. Intra-articular pressure volume monitoring could be utilized to sensitively evaluate the physical properties of synovium in a clinical setting, which could not be evaluated using the conventional method. Further prospective studies are warranted.
ACKNOWLEDGMENTS
This study was supported by the Bio and Medical Technology Development Programs (No. 2017M3A9D8048711 and No. 2016M3A9F1941984) of the National Research Foundation (NRF) funded by the Korean government (MSIT).
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
All authors contributed to the conception and design of the study, all were involved in drafting the article critically for important intellectual content, and all approved the content of the manuscript. Sun Gun Chung (E-mail: [email protected]) had full access to all data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Specific roles were as follows. Study conception and design: Jae Hyun Lee, Keewon Kim, and Sun Gun Chung. Acquisition of data: Jae Hyun Lee, Keewon Kim, and Sun Gun Chung. Analysis and interpretation of data: Jae Hyun Lee, Keewon Kim, and Sun Gun Chung. Drafting of the article: Jae Hyun Lee. Final approval of the article: Sun Gun Chung.
Open Research
DATA AVAILABILITY STATEMENT
The data sets for this study are available on request. The raw data supporting the conclusions of this manuscript will be made available by the authors to any qualified researcher. Contact: Jae Hyun Lee (ORCID 0000-0002-4927-9722).