Using area and volume measurement via weightbearing CT to detect Lisfranc instability
LEVEL OF EVIDENCE:
Level III, comparative diagnostic study
Abstract
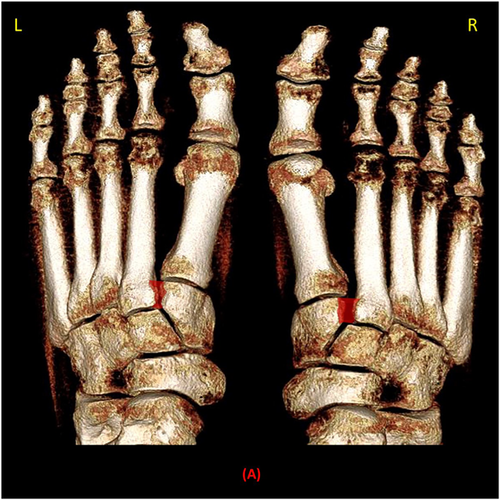
Weightbearing CT (WBCT) allows evaluation of the Lisfranc joint under physiologic load. We compared the diagnostic sensitivities of one-dimensional (1D) distance, two-dimensional (2D) area, and three-dimensional (3D) volumetric measurement of the injured Lisfranc joint complex (tarsometatarsal, intertarsal, and intermetatarsal) on WBCT among patients with surgically-confirmed Lisfranc instability. The experimental group comprised of 14 patients having unilateral Lisfranc instability requiring operative fixation who underwent preoperative bilateral foot and ankle WBCT. The control group included 36 patients without foot injury who underwent similar imaging. Measurements performed on WBCT images included: (1) Lisfranc joint (medial cuneiform-base of second metatarsal) area, (2) C1-C2 intercuneiform area, (3) C1-M2 distance, (4) C1-C2 distance, (5) M1-M2 distance, (6) first tarsometatarsal (TMT1) angular alignment, (7) second tarsometatarsal (TMT2) angular alignment, (8) TMT1 dorsal step off distance, and (9) TMT2 dorsal step-off distance. In addition, the volume of the Lisfranc joint in the coronal and axial plane were calculated. Among patients with unilateral Lisfranc instability, all WBCT measurements were increased on the injured side as compared to the contralateral uninjured side (p values: <.001–.008). Volumetric measurements in the coronal and axial plane had a higher sensitivity (92.3%; 91.6%, respectively) and specificity (97.7%; 96.5%, respectively) than 2D and 1D Lisfranc joint measurements, suggesting them to be the most accurate in diagnosing Lisfranc instability. The control group showed no difference in any of the measurements between the two sides. WBCT scan can effectively differentiate between stable and unstable Lisfranc injuries. Lisfranc joint volume measurements demonstrate high sensitivity and specificity, suggesting that this new assessment has high clinical implications for diagnosing subtle Lisfranc instability.
1 INTRODUCTION
Lisfranc joint instability can result in high morbidity and long-term disability if inadequately treated.1, 2 Displaced injuries are readily diagnosed, but injuries that result in only subtle instability may be more difficult to identify, even with weight bearing radiographs.3 Subtle Lisfranc instabilities usually have clinical signs and symptoms with equivocal initial non-weightbearing radiographs.4 Clinical findings are pain over the Lisfranc joint, which can be reproduced by passive movement of individual metatarsal heads and the presence of plantar ecchymosis.4 When diagnosis remains in question, therefore, clinicians have increasingly employed cross sectional imaging modalities such as magnetic resonance imaging (MRI) and computed tomography (CT)—but each has unique limitations.2, 5 MRI readily identifies Lisfranc ligamentous injury but does not distinguish between injury and instability by virtue of its unstressed views and suboptimal bony detail. Similarly, conventional CT scanning is able to demonstrate midfoot alignment with excellent anatomic detail, but does so without a physiologic load and may therefore miss subtle instability.
Bilateral weightbearing CT (WBCT) offers several potential advantages over these other imaging modalities. It not only visualizes the Lisfranc joint complex while under physiological load, but also affords a direct comparison between the injured and uninjured sides.6, 7 Moreover, this newer technology comes with additional software capabilities that enable multidimensional analytic assessments heretofore unutilized. The primary aim of this study was thus to evaluate the ability of bilateral foot WBCT to diagnose Lisfranc instability utilizing one-dimensional (1D), two-dimensional (2D) and three-dimensional (3D) measurement amongst patients with operatively-confirmed Lisfranc instability, while using their contralateral, uninjured sides as internal controls. The secondary aim was to evaluate a separate control cohort of patients devoid of foot injury who had also undergone bilateral ankle WBCT, to validate the use of the contralateral side as an internal control. Last, our study aimed to compare the sensitivities of these various measurements—including volumetric 3D measurement of the Lisfranc joint—vis a vis an optimized ability to diagnose even subtle Lisfranc instability.
2 MATERIALS AND METHODS
2.1 Study population and design
After Institutional Review Board approval, 227 bilateral foot and ankle WBCT scans performed between 2015 and 2019 at an academic medical center using the PedCAT (CurveBeam) were retrospectively reviewed. The images encompassed bilateral ankles as well as the entire foot. The patient group included individuals diagnosed with Lisfranc instability that was confirmed intraoperatively and who had undergone preoperative WBCT scans. Patients were intraoperatively determined to have had an unstable Lisfranc joint if the dorsal ligament(s) were ruptured and any diastases or subluxation was seen after gently inserting a small freer elevator into the joint.8, 9 Furthermore, the intercuneiform joint (C1-C2) was deemed unstable if the dorsal intercuneiform ligament was ruptured with any diastasis or subluxation.8, 10 These patients received surgical fixation of the Lisfranc joint complex as part of their clinical course. The control group included individuals who underwent bilateral WBCT imaging to evaluate the ankle in the setting of acute trauma or posttraumatic changes but without associated foot injury. Exclusion criteria were patients with Lisfranc injuries who had additional foot or ankle injuries on either side, patients younger than 18 years of age, and patients diagnosed with midfoot arthritis.
Fourteen patients (28 feet) with unilateral Lisfranc instability confirmed intraoperatively and requiring operative fixation were included in the patient group, and 36 individuals (72 feet) with bilateral, uninjured Lisfranc joints were included in the control group. Collected demographic data included age, gender, and body mass index (BMI).
2.2 WBCT 1D and 2D measurements
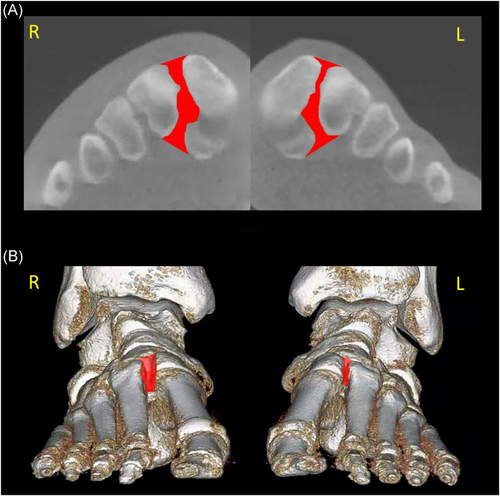
Prior studies have demonstrated that the average height of the medial cuneiform is 30 mm on CT scan.11-13 Axial plane measurements were, therefore, assessed at the junction of the upper and middle third of the medial cuneiform defined as 10 mm below its dorsal surface. The Lisfranc joint area in our study was defined as the space between the medial cuneiform and the base of the second metatarsal delineated by two lines adjoining the articulated portions of the base of the second metatarsal and the medial cuneiform (Figure 1).13 The intercunieform area was defined as the space between the medial and intermediate cuneiform outlined by two lines along the proximal and distal articulating cortex of the intermediate cuneiform extending to the medial cuneiform on the axial plane (Figure 1).14 Other axial plane 1D and 2D measurements included the distance between the medial cuneiform (C1) and the base of second metatarsal (M2) (C1-M2); the intercuneiform distance (C1-C2); the distance between first and second metatarsal (M1-M2); the first tarsometatarsal (TMT1) alignment relative to C1; and the second tarsometatarsal (TMT 2) alignment relative to C2.9 Axial plane alignment was measured 10 mm plantar from the dorsal extent of C2 at both the first (TMT 1) and second (TMT 2) tarsometatarsal joints. Dorsal step offs were measured in the sagittal plane at the midportion of the respective joints (Figures 1 and 2).9 All measurements were performed using Visage Software (version 7.1.14; Visage Imaging Inc.).
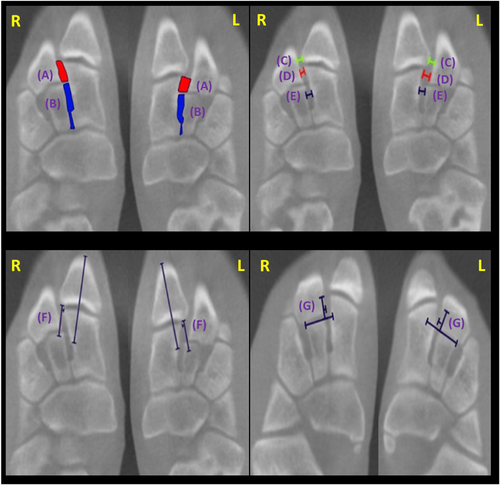

2.3 WBCT 3D volumetric measurement
The volume of the Lisfranc joint (medial cuneiform—base of second metatarsal) on WBCT was measured using Visage Software (version 7.1.14; Visage Imaging Inc.). This imaging software has the ability to calculate 3D volume amounts on cross sectional imaging. First, the axial plane slices (0.3 mm standard thickness) were used to measure the Lisfranc joint area on each slice, starting from the appearance of the first tarsometatarsal joint until the disappearance of the second tarsometatarsal joint. Thereafter, the Lisfranc joint area in the coronal plane was measured on each CT slice (0.3 mm standard thickness), starting from the base of the second metatarsal until the anterior surface of the medial cuneiform. This measurement was defined as the space between the medial cuneiform and second metatarsal delineated by two tangential lines adjoining the dorsal cortex and the plantar cortex of the medial cuneiform and the second metatarsal (Figure 4).13 Thereafter, the volume of the Lisfranc joint in mm3 was created and measured in both the axial and coronal orientation utilizing following the formula:  , wherein A is the area in each slice and T is the slice thickness (in the current study 0.3 mm; Figures 3 and 4).
, wherein A is the area in each slice and T is the slice thickness (in the current study 0.3 mm; Figures 3 and 4).
Two orthopaedic surgeons independently performed the measurements as well as the volume calculations in four randomly selected patients to assess interobserver agreement using the intraclass correlation coefficient (ICC) through a two-way mixed effects model with absolute agreement. The absolute agreement determines how much a measurement that is done by one observer varies from that of the other observer. The ICCs were interpreted according to the guidelines provided by Shrout and Fleiss where values between 0 and 0.10 were considered as virtually none; 0.11 and 0.40 as slight; 0.41 and 0.60 as fair; 0.61 and 0.80 as moderate; and values 0.81 and 1.0 considered as substantial.15
2.4 Statistical analysis
The baseline characteristics, namely age, gender, and BMI were analyzed and summarized using percentage and frequency for categorical variables and mean ± SD for continuous data. To determine differences in demographics between the patient and the control group a χ 2 test was used for dichotomous and categorical explanatory variables. A paired t test (a parametric test used when comparing two dependent samples) was applied to test the primary hypothesis that 1D, 2D, and 3D WBCT measurements of the Lisfranc joint complex were increased on the injured side as compared to the contralateral, uninjured side among patients with Lisfranc instability. To test our secondary hypothesis that 3D volumetric measurement was more sensitive for distinguishing stable and unstable Lisfranc injuries than the other WBCT measurements, absolute value difference were compared between the injured and injured side. Secondarily, the relative ratios between injured and uninjured sides were also calculated and then a comparison was performed using a Wilcoxon signed-rank test (a nonparametric test used when comparing two dependent samples). Finally, the data from the left and right feet in the control group (n = 72), as well as the uninjured feet in the patient group (n = 14) was pooled, and the stable/unstable cut-off values for each 1D, 2D, and 3D WBCT measurement was calculated by the mean of the measurement + 2 SD. Subsequently, the sensitivity, specificity, negative, and positive predictive value for each of the 2D and 3D measurements of the Lisfranc joint was determined. In this study, a p value of less than .05 was considered as statistically significant. Data analyses were performed using Stata 13.0 (StataCorp LP).
3 RESULTS
No differences were found between the Lisfranc and control populations regarding age, gender, and BMI (Table 1). In the control group, there was no evidence of foot injury in any patient; ankle diagnoses precipitating the WBCT included syndesmotic widening (22; 61.1%), ankle fracture (6; 16.7%), ankle impingement (2; 5.6%), lateral ankle sprain (2; 5.6%), lateral ankle reconstruction (2; 5.6%), or an ankle osteoarthritis (2; 5.6%).
| Control group (n = 36) | Patient group (n = 14) | p Value | |||
|---|---|---|---|---|---|
| Gender | F | 58.3% (n = 21) | F | 42.9% (n = 6) | .19 |
| M | 41.7% (n = 15) | M | 57.1% (n = 8) | ||
| Age (years) mean ± SD | 35.7 ± 16.5 | 32.2 ± 15.5 | .32 | ||
| BMI (kg/m2) mean ± SD | 26.7 ± 4.6 | 26.3 ± 5.3 | .72 | ||
- Abbreviations: BMI, body mass index; F, female; M, male; WBCT, weightbearing computed tomography.
3.1 Weightbearing 1D and 2D measurements
Among patients with Lisfranc instability, all WBCT 1D and 2D measurements were significantly increased on the injured as compared to the contralateral, uninjured side (p values ranging from <.001 to .008; Table 2). In contrast, among the control group, there there was no difference in 1D or 2D measurements between paired uninjured feet (Table 3). The ICCs were 0.96 for C1-M2 distance (95% confidence interval [CI]: 0.94–0.98), 0.92 for C1-C2 distance (95% CI: 0.87–0.95), 0.87 for M1-M2 distance (95% CI: 0.80–0.92), 0.84 for TMT2 alignment (95 CI: 0.75–0.88), 0.83 for TMT1 alignment (95% CI: 0.73–0.89), 0.94 for TMT1 dorsal step off (95% CI: 0.92–0.97), 0.90 for TMT2 dorsal step off (95% CI: 0.88–0.94), 0.97 (95% CI: 0.95–0.98) for the Lisfranc joint area in the axial plane, and 0.91 for the intercuneiform area (95% CI: 0.89–0.94), indicating substantial agreement between the two observers for all measurements.
| Measurement | Patient group | Difference between the injured and uninjured foot | 95% CI | Median ratio (IQR) a | p Value b | |
|---|---|---|---|---|---|---|
| Uninjured foot (mean ± SD) | Injured foot (mean ± SD) | |||||
| Coronal Lisfranc joint volume (mm3) | 396.7 ± 112.5 | 701.4 ± 123.6 | 304.7 | [235.6–373.8] | 1.9 (1.7–2.2) | <.001 |
| Axial Lisfranc joint volume (mm3) | 236.1 ± 86.6 | 418.7 ± 96.1 | 182.7 | [152.9–212.3] | 1.9 (1.6–2.3) | <.001 |
| Axial Lisfranc joint area (mm2) | 15.1 ± 6.9 | 35.7 ± 11.1 | 20.7 | [17.1–24.3] | 2.3 (2.0–3.0) | <.001 |
| Intercuneiform area (mm2) | 24.2 ± 10.8 | 33.5 ± 12.8 | 9.3 | [4.6–13.9] | 1.3 (1.1–1.6) | .001 |
| C1-M2 distance (mm) | 2.1 ± 1.1 | 5.3 ± 0.9 | 3.2 | [2.9–3.6] | 2.3 (2.1–3.9) | <.001 |
| C1-C2 distance (mm) | 1.1 ± 0.4 | 2.5 ± 0.8 | 1.3 | [0.9–1.7] | 2.1 (1.9–2.6) | <.001 |
| M1-M2 distance (mm) | 1.8 ± 0.8 | 3.1 ± 0.8 | 1.3 | [0.5–1.9] | 1.7 (1.5–2.4) | .002 |
| TMT1 alignment (mm) | 1.1 ± 0.4 | 2.1 ± 0.5 | 1.1 | [0.8–1.4] | 1.7 (1.6–2.3) | <.001 |
| TMT2 alignment (mm) | −0.5 ± 0.9 | 1.2 ± 0.9 | 1.8 | [1.2–2.1] | 1.6 (0.7–3.0) | <.001 |
| TMT1 dorsal step-off (mm) | −0.8 ± 1.3 | 0.7 ± 1.6 | 1.5 | [0.4–2.7] | 1.0 (0.7–2.0) | .008 |
| TMT2 dorsal step-off (mm) | −1.2 ± 1.1 | 0.6 ± 1.2 | 1.8 | [0.8–2.7] | 0.7 (0.6–1.5) | .001 |
- Abbreviations: CI, confidence interval; CT, computed tomography; IQR, interquartile range; WBCT, weightbearing computed tomography.
- a Ratio: Lisfranc 2D and 3D measurements in injured foot/contralateral uninjured foot.
- b p Value of less than .05 was considered as statistically significant.
| Measurement | Control group | Difference between the left and right foot | 95% CI | p Value* | |
|---|---|---|---|---|---|
| Left foot (mean ± SD) | Right foot (mean ± SD) | ||||
| Coronal Lisfranc joint volume (mm3) | 399.3 ± 110.9 | 399.4 ± 115.8 | 0.1 | [−1.7–2.0] | .89 |
| Axial Lisfranc joint volume (mm3) | 232.1 ± 88.9 | 235.6 ± 94.8 | 3.6 | [−2.0–5.1] | .35 |
| Axial Lisfranc joint area (mm2) | 13.5 ± 5.9 | 13.8 ± 6.1 | 0.4 | [−0.1–0.1] | .12 |
| Intercuneiform area (mm2) | 24.5 ± 6.3 | 24.5 ± 6.4 | 0.01 | [−0.1–0.2] | .98 |
| C1-M2 distance (mm) | 2.1 ± 0.8 | 2.1 ± 0.8 | 0.6 | [−0.1–0.2] | .23 |
| C1-C2 distance (mm) | 1.2 ± 0.4 | 1.2 ± 0.3 | 0.1 | [−0.1–0.2] | .18 |
| M1-M2 distance (mm) | 2.3 ± 0.6 | 2.4 ± 0.6 | 0.1 | [−0.2–0.1] | .17 |
| TMT1 alignment (mm) | 0.9 ± 0.7 | 1.1 ± 0.6 | 0.1 | [−0.3–0.1] | .25 |
| TMT2 alignment (mm) | −0.5 ± 0.7 | −0.4 ± 0.8 | 0.1 | [−0.3–0.2] | .48 |
| TMT1 dorsal step-off (mm) | −1.1 ± 0.9 | −1.1 ± 1.1 | 0.0 | [−0.2–0.1] | .72 |
| TMT2 dorsal step-off (mm) | −1.5 ± 0.6 | −1.3 ± 0.7 | 0.2 | [−0.3–0.1] | .11 |
- Abbreviations: CI, confidence interval; CT, computed tomography; WBCT, weightbearing computed tomography.
- * p Value of less than .05 was considered as statistically significant.
3.2 WBCT 3D volume measurement
In the Lisfranc group, the volume measurement of the Lisfranc joint was larger on the injured side compared to the contralateral, uninjured side (p < .001; Table 2). In contrast, within the control group there was no difference in volume measurements between paired uninjured feet (Table 3). The ICC for the Lisfranc joint was 0.97 (95% CI: 0.95–0.98) in the axial plane and 0.96 (95% CI: 0.94–0.98) in the coronal plane, indicating substantial interobserver agreement.
3.3 WBCT 3D versus 1D or 2D measurements
In the Lisfranc group, 3D volumetric measurements of the Lisfranc joint in the coronal plane on average had the largest absolute difference between the injured and uninjured side (mean: 304.7 mm3; 95% CI: 235.6–373.8), followed by volumetric measurements in the axial plane (mean: 182.7 mm3; 95% CI: 152.9–212.3), and Lisfranc joint area (mean: 20.7 mm2, 95% CI: 17.1–24.3; Table 2). Notably, the volumetric measurements in the coronal and axial plane had a higher sensitivity (92.3%, 95% CI: 62.1–99.6; 91.6%, 95% CI: 59.8–99.5) and specificity (97.7%, 95% CI: 91.1–99.6; 96.5%, 95% CI: 89.7–99.1), corresponding to a cut off value of 638.5 and 414.4 mm3, respectively, than the 2D and 1D WBCT Lisfranc measurements (Table 4). This suggest that volumetric measurements are the most accurate measurements for distinguishing stable from unstable Lisfranc injury (Table 4). The relative ratio between measurements on the injured and uninjured sides for the Lisfranc joint 3D volumetric measurements showed no difference when compared to the relative ratios of the 1D or 2D WBCT measurements (p values ranging from .07 to .93; Table 2).
| Measurements | Cut-off value (n = 86 feet; mean + 2 SD) | Sensitivity (%) | 95% CI | Specificity (%) | 95% CI | PPV (%) | NPV (%) |
|---|---|---|---|---|---|---|---|
| Coronal Lisfranc joint volume | 638.5 mm3 | 92.3 | [62.1–99.6] | 97.7 | [91.1–99.6] | 85.7 | 98.8 |
| Axial Lisfranc joint volume | 414.4 mm3 | 91.6 | [59.8–99.5] | 96.5 | [89.7–99.1] | 78.6 | 98.8 |
| Lisfranc Area | 26.1 mm2 | 78.6 | [48.8–94.3] | 96.5 | [89.4–99.1] | 76.8 | 96.5 |
| C1-M2 distance | 3.8 mm | 78.6 | [48.8–94.3] | 96.5 | [89.4–99.1] | 76.8 | 96.5 |
- Abbreviations: C1-M2, distance between medial cuneiform to base of second metatarsal; CI, confidence interval; NPV, negative predictive value; PPV, positive predictive value.
4 DISCUSSION
Distinguishing Lisfranc injury from instability remains a critical step towards optimizing patient outcome, but diagnosis of subtle instability continues to be a challenge with current imaging modalities.2 The aim of this study was to evaluate the Lisfranc joint complex using 1D, 2D, and 3D measurements on WBCT scan among patients with operatively confirmed Lisfranc instability, as well as among a cohort of control patients without foot injury. Our data suggest that WBCT can effectively identify most patients with Lisfranc instability using either 1D distance, 2D area and alignment, or 3D volumetric measurements, but strongly corroborates 3D volumetric measurement as the best and most sensitive technique—particularly when trying to differentiate more subtle instability patterns. The lack of laterality difference among uninjured patients when using this form of assessment further underscores the reliability of the contralateral extremity as an internal control.
Prior reports that examine Lisfranc instability have employed weightbearing radiographs, conventional, non-WBCT scans, MRI and manual stress radiographs for diagnosis, but each of these modalities comes with inherent limitations.3, 11, 16-18 Weightbearing radiographs readily allow bilateral comparison under physiologic load but have limited sensitivity, especially as the instability becomes increasingly subtle.3 Furthermore, radiographic evaluation of the Lisfranc joint necessitates an average craniocaudal X-ray beam angulation of 28.9°, which may be difficult to optimize in clinical practice or adapt to natural variations in patient anatomy.16 In turn, cross-sectional MRI readily identifies Lisfranc ligament injury but not instability by virtue of being an unstressed modality with particularly poor bony detail in the acute trauma setting due to superimposed edema patterns.17, 19, 20 Furthermore, it does not afford bilateral comparison. Conventional CT scanning allows excellent visualization of Lisfranc alignment, but it does so unilaterally and without physiologic load.16, 20, 21 This may result in subtle cases of instability being overlooked. Bridging many of these concerns, WBCT allows cross-sectional visualization of the Lisfranc region under physiologic load while affording a comparison to the uninjured side as an internal control.7, 22 The latter is critical given the variable anatomy of the Lisfranc joint across individuals.13
The current study highlights the utility of WBCT 1D, 2D, and 3D measurements to evaluate Lisfranc instability. All measurements—be they distance, alignment, area, or volume—effectively diagnosed Lisfranc instability on WBCT when comparing injured and uninjured sides. Highlighting the specificity of such measurements, these differences were uniformly not observed among the control cohort. Most notably, however, as Lisfranc instability becomes increasingly subtle the sensitivities of such measurements become more critical for effectively diagnosing instability.
Among the Lisfranc group, volumetric 3D measurements of the Lisfranc articulation between the base of the second metatarsal and the medial cuneiform clearly afforded the largest absolute difference between injured and uninjured sides. The Lisfranc joint volume increased by an average of 304.7 mm3 in the coronal plane and 182.7 mm3 in the axial plane following destabilization. It is imperative to recognize that this was a full order of magnitude higher than the next highest value, Lisfranc area, which showed an average of 20.7 mm2 increase between the injured and the uninjured side (Table 2).
Gauging the sensitivity of each measurement strategy—be it distance, area, or volume—becomes increasingly critical as Lisfranc instability becomes increasingly more subtle. Three strategies for doing so focus on either the absolute difference in values between the injured and uninjured sides or diagnostic accuracy for a given cut-off value or on the relative ratios between values. Absolute value difference is most intuitive because measurement values will get smaller with more subtle instability. With higher absolute differences between the injured and uninjured side, it is less likely that a comparison measurement inadvertently results in a Type II statistical error—finding no difference when, in reality, one was present (in this case, finding no Lisfranc instability when instability was indeed present). This is buttressed by the fact that no differences were found in the control group having no injury to either foot. Notably, we also found that the volumetric measurements in the coronal and the axial plane had a higher sensitivity and specificity than the 2D and 1D WBCT Lisfranc measurements, indicating high accuracy of the diagnostic test (Table 4). The relative ratios, on the other hand, were not significantly different among the measurements, largely for geometric reasons. As the distance between the medial cuneiform and the base of the second metatarsal becomes larger, the length of the articulation between the medial cuneiform and second metatarsal base does not change. With displacement, the 2D area measurements increase in width but not length, and thereby increase proportionally to the 1D distance measurements. The same holds true for 3D Lisfranc joint volume measurements, which in this setting incorporated sequential additions of area measurements within individual WBCT slices while bearing in mind slice thickness necessary to create volumetric measurement.
It should also be highlighted that coronal plane volume measurements at the Lisfranc joint were greater in value than axial plane volume measurements. This stems from the fact that the second metatarsal tends to displace not only laterally but also superiorly. The coronal plane axis better captures this translation because the axial plane is preset by the radiologist, and does not necessarily align with the most more oblique translation of the second metatarsal relative to the medial cuneiform (often lateral and superior). The coronal view allows the creation of a 3D parallelogram-like structure that effectively captures this translation, and may better serve towards volumetric measurements of the Lisfranc.
This study has a few limitations that should be considered. First, while all patients included in this study had surgically-confirmed Lisfranc instability, additional studies are necessary to confirm the role of WBCT in diagnosing increasingly subtle cases of instability, especially if the diagnosis is unclear on initial weight bearing radiographs. We recognize that in some cases patients with acute trauma might not be able to fully weight bear due to pain while performing WBCT. However, in the current study, patients were able to fully weight bear during the examination. Furthermore, a previous study has shown that nearly 50% weightbearing is enough to substantially elongate intact dorsal Lisfranc ligament and load beyond 50% weightbearing fails to further increase the dorsal Lisfranc ligament length. Second, we did not include Lisfranc patients with associated tarsal or metatarsal fractures. Superimposed fractures could impact absolute values of the 2D and 3D measurements, though comparison to the contralateral, uninjured side would likely obviate many of these concerns. Third, success of 2D and 3D evaluation of the Lisfranc joint is entirely predicated on having the contralateral, uninjured foot available to serve as an internal control. It is feasible that with larger amounts of data one could develop absolute thresholds values for both 2D and 3D measurements that enable definitive confirmation of Lisfranc instability in isolation—and thereby avoid any need for contralateral comparison. Last, measurement techniques such as area and volume may not be available in most CT imaging viewing systems. Thus, software enhancements are necessary before widespread use of volumetric measurements can be integrated into existing clinical practice.
5 CONCLUSION
WBCT can effectively diagnose Lisfranc instability among patients with surgically-confirmed Lisfranc instability. While 1D distance, 2D area and alignment, and 3D volumetric measurements can all be used to identify such instability, 3D volume measurements are clearly most sensitive towards this end and thus strongly recommended for future application in cases of questionable Lisfranc injury—particularly when injuries are subtle. However, a future prospective study is necessary to better understand the utility of WBCT to diagnose such subtle instabilities. Finally, when performing these 3D volume measurements it appears that coronal plane assessment is best suited to evaluate the often oblique nature of Lisfranc joint displacement. Based on available data, the authors recommend this new technique to supplant earlier methods for optimized identification of Lisfranc instability.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Rohan Bhimani: substantial contributions to design, acquisition of data, and analysis and interpretation of data; involved in drafting and revision of the manuscript. Pongpanot Sornsakrin and Soheil Ashkani-Esfahani: substantial contributions to design, and analysis and interpretation of data; involved in drafting and revision of the manuscript. Bart Lubberts: substantial contributions to acquisition of data, and analysis and interpretation of data; involved in drafting and revision of the manuscript. Cesar De Cesar Netto, Gregory R. Waryasz, and Gino M.M.J. Kerkhoffs: substantial contributions to design; involved in drafting and revision of the manuscript. Daniel Guss and Christopher W. DiGiovanni: substantial contributions to design and interpretation of data; involved in drafting and revision of the manuscript. All authors have read and approved the final submitted manuscript.