Localized stomach cancer: Perioperative or postoperative approach? A meta-analysis of phase III studies
Declaration of conflict of interest: None.
Abstract
Background and Aim
Despite the development and standardization of surgical techniques in the treatment of localized gastric adenocarcinoma, the loco-regional and metastatic recurrence rate remains high. A combined radiochemotherapeutic regimen (the MacDonald regimen) as well as perioperative chemotherapy allows a significant improvement in the survival of patients with localized gastric adenocarcinoma with a reduction in the recurrence rate compared to surgery alone. The purpose of this review is to specify the best therapeutic approach in the treatment of localized gastric cancer.
Methods
We performed a systemic search of Medline, Embase, and the Cochrane Central Register of Controlled Trials using PubMed, Google Scholar, and Ovid without language restriction. Hazard ratio (HR) with 95% confidence interval (CI) was reported.
Results
We pooled 727 patients from two phase III randomized controlled trials. There was a benefit of perioperative chemotherapy versus surgery alone on the overall survival (OS) (HR = 0.72, 95% CI: 0.55–0.95) and on disease free survival (DFS) (HR = 0.65, CI: 0.50–0.85). Adjuvant chemotherapy was superior to surgery alone based on OS and disease free survival (CLASSIC study HR = 0.72, CI: 0.52–1 and HR = 0.56, CI: 0.44–0.72, respectively). Adjuvant radiochemotherapy was superior to surgery alone (HR = 1.35, 95% CI: 1.09–1.66; P = 0.005).
Conclusion
A face-to-face comparison of perioperative chemotherapy versus adjuvant chemotherapy versus chemoradiotherapy is necessary.
Introduction
Stomach cancer remains a serious pathology with a poor prognosis. It occupies the second rank in cancers of the digestive system.1 Despite the development and standardization of surgical techniques in the treatment of localized forms, the loco-regional and metastatic recurrence rate remains high. Indeed, the recurrence rate can reach 70% in some series with a 5-year survival of around 20–30% in Western series. The National Cancer Data Base on gastric cancer shows that survival after surgery remains poor (5-year relative survival: 43% for Stage I, 37% for Stage II, 18% for Stage III).2 Radiochemotherapeutic regimen (MacDonald regimen) followed by perioperative chemotherapy results in a significant improvement in the survival of patients with localized gastric adenocarcinoma, with a reduction in the recurrence rate, and has become, therefore, the new therapeutic standard. The purpose of this review is to specify the best therapeutic approach in localized gastric cancer.
Methods
Study selection
We conducted a search of Medline, Embase (January 2001 to January 2018), and the Cochrane Central Register of Controlled Trials using PubMed, Google Scholar, and Ovid, without language restriction. The search was limited to human studies. The following medical subject heading terms were used: “gastric cancer,” “chemotherapy,” “radiotherapies,” “full text,” and “randomized controlled trial.” Boolean operators (“NOT,” “AND,” “OR”) were used.
Inclusion criteria
We included in this study phase III randomized controlled trials (RCTs) comparing surgery alone versus adjuvant treatment or perioperative treatment in case of stage IB–IIIB resectable gastric adenocarcinoma.
Exclusion criteria
- Case reports, letters, editorials, comments, reviews, and abstracts with insufficient details to meet the inclusion criteria;
- Nonrandomized studies;
- Cases without the full text.
Data extraction
The investigator of the extracted data was Wala Ben Kridis. Data were abstracted by three independent reviewers. Each article was scrutinized to determine whether it met the predetermined inclusion and exclusion criteria. Data were abstracted independently by each reviewer using a standardized data collection form to increase the uniformity of data extraction and to reduce reporting bias. In case of any discrepancy, a consensus decision was made with the help of the senior author. Corresponding authors were contacted for any missing data points. Disagreements over values or analyses were resolved by discussion.
Assessment of study quality
Once a study was selected for inclusion, two authors (Wala Ben Kridis, Haitham Rejab) independently rated the quality of each randomized trial using the Jadad et al.3 scale, which is a validated instrument for assessing the quality of randomized studies. This is a five-question scale assessing the following: (i) whether the study is randomized, (ii) whether the study is double-blinded, (iii) whether withdrawals are described, (iv) whether randomization allocation is explained adequately, and (v) whether blindness is described adequately.
Scores range from 1 to 5, with a higher score indicating higher quality. We assigned an arbitrary score of less than 3 to indicate a lower study quality, whereas a rating of 3 or more points were considered of higher quality and were used as part of the sensitivity analysis.
Statistical analyses
The effect measures estimated were the hazard ratio (HR) for dichotomous data, which we report with 95% confidence intervals (CIs). HR indicates the risk of an individual with localized gastric cancer who received systemic treatment developing progression or death compared with the risk of an individual receiving surgery alone. Relative risk reduction (RRR), absolute risk reduction (ARR), and the number needed to treat (NNT) were calculated to assess whether the relative risk was clinically important.
Results
Study characteristics
Our initial search yielded 306 literature citations (Fig. 1). Of these, 44 citations were excluded because full text was not available and 254 because they were non RCTs. Finally, eight RCTs were included (Table 1).

| Study | Number of patients | Study design | 5-year rate survival | HR [95% CI] |
|---|---|---|---|---|
| Classic | 1035 | Adjuvant eight cycles XELOX versus observation | 78 versus 69% | 0.66 [0.51–0.85] |
| ITACA-S | 1100 | Adjuvant folfiri then docetaxel-cisplatine versus adjuvant LV5FU2 | 51.0 versus 50.6% | 0.98 [0.82–1.18] |
| MacDonald | 556 | Adjuvant 5 cycles FUFOL+ radiotherapy versus observation | 40 versus. 28% | 1.35 [1.09–1.66] |
| Magic | 503 | Perioperative chemotherapy (epirubicine-cisplatine-5-fluorouracile: ECF) versus surgery alone | 36 versus. 23% | 0.75 [0.6–0.95] |
| FFCD | 224 | Perioperative chemotherapy (cisplatine-5-fluorouracile: PF) versus surgery alone | 38 versus 24% | 0.69 [0.5–0.95] |
| FLOT | 716 | Perioperative chemotherapy (FLOT) versus perioperative chemotherapy (ECF or ECX) | 45 versus 36% | 0.77 [0.63–0.94] |
| Artist | 458 | Postoperative treatment with capecitabine plus cisplatin (XP) versus XP plus radiotherapy with capecitabine (XP/XRT/XP) |
The secondary end point of overall survival was not analyzed | — |
| Critics | 788 | Perioperative chemotherapy versus perioperative chemotherapy + adjuvant radiotherapy | 41.3 versus 40.9% (P = 0.99) | — |
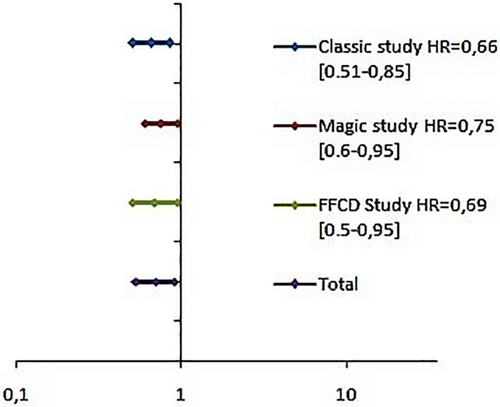
Adjuvant chemotherapy
The CLASSIC study is a phase III RCT undertaken in 37 centers. It included non-metastatic gastric cancer ≥Stage II treated by curative D2 gastrectomy. It compared adjuvant chemotherapy with capecitabine and oxaliplatin (arm 1) versus placebo (arm 2). The 3-year disease-free survival (DFS) was 74% in the arm 1 versus 59% in the arm 2 (HR = 0.56, 95% CI: 0.44–0.72; P < 0.0001). Grade 3 or 4 adverse events were reported in 56% for arm 1 and 6% in arm 2.4 The The ITACA-S study was designed to evaluate a sequential treatment with FOLFIRI (irinotecan plus 5-fluorouracil/folinic acid) followed by docetaxel plus cisplatin versus 5-fluorouracil/folinic acid alone in patients with radically resected gastric cancer. No statistically significant difference was detected for both DFS (HR = 1.00, 95% CI: 0.85–1.17; P = 0.974) and OS (HR = 0.98; 95% CI: 0.82–1.18; P = 0.865).5
Adjuvant radiochemotherapy
The McDONALD is a phase III study that investigated the effect of surgery plus adjuvant chemoradiotherapy on the survival of patients with resectable gastric adenocarcinoma. The median OS in the surgery group was 27 months, compared with 36 months in the surgery and chemoradiotherapy group (P = 0.005). The HR for relapse was 1.52 (95% CI: 1.23–1.86; P < 0.001).6 The main criticism of this study was that nodal dissection was D0 in 54% of cases (suboptimal surgery). Subgroup analysis in the update published in 2012 showed that there was no benefit of concomitant chemoradiotherapy in the case of women or in case of independent cell carcinoma.7
Adjuvant chemotherapy versus concomitant chemoradiotherapy
The ARTIST trial was the first study, to our knowledge, to investigate the role of postoperative chemoradiotherapy in patients with curatively resected gastric cancer with D2 lymph node dissection. This trial was designed to compare postoperative treatment with capecitabine plus cisplatin (XP) versus XP plus radiotherapy with capecitabine. Overall, the addition of XRT to XP chemotherapy did not significantly prolong the DFS (P = 0.0862).8 With 7 years of follow-up, DFS remained similar between the treatment arms (P = 0.0922). OS also was similar (HR = 1.130; 95% CI: 0.775–1.647; P = 0.5272).9
Perioperative chemotherapy
In the MAGIC phase III study, patients with resectable gastric adenocarcinoma received either perioperative chemotherapy and surgery (250 patients) or surgery alone (253 patients). Chemotherapy consisted of three preoperative and three postoperative cycles of intravenous epirubicin, cisplatin, and fluorouracil. The primary end point was the OS. Compared with the surgery group, the perioperative chemotherapy group had a higher OS (P = 0.00910) (Fig. 2) and of progression-free survival (P < 0.001) (Fig. 3). In the MAGIC trial, mismatch repair deficiency (MMRD) and microsatellite instability (MSI) were associated with a positive prognostic effect in patients treated with surgery alone and with a differentially negative prognostic effect in patients treated with chemotherapy.
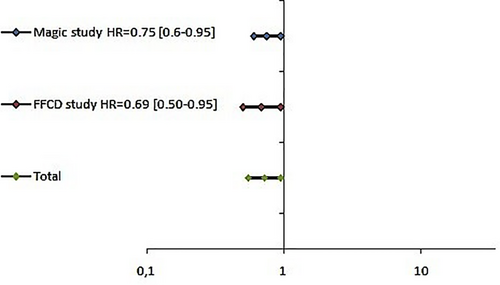

The FFCD trial was designed to evaluate the benefit in OS of perioperative fluorouracil plus cisplatin in resectable gastroesophageal adenocarcinoma. Overall, 224 patients with resectable gastric adenocarcinoma were randomly assigned to either perioperative chemotherapy or surgery. Compared with the surgery group, the perioperative chemotherapy group had a better OS (5-year rate 38 vs 24%; [HR] for death = 0.69; 95% CI: 0.50–0.95; P = 0.02) (Fig. 2) and a better DFS (5-year rate: 34% vs 19%; HR = 0.65; 95% CI: 0.48–0.89; P = 0.003)11 (Figs 3, 4).
FLOT4 (NCT01216644) is a multicenter, randomized, phase III trial that compares the docetaxel-based triplet FLOT with the anthracycline-based triplet ECF/ECX as a perioperative treatment for patients with resectable gastric adenocarcinoma.
FLOT improved the OS (median OS, 35 months with ECX/ECF vs 50 months with FLOT; HR = 0.77 [0.63–0.94]; P = 0.012). FLOT also improved the PFS (P = 0.004). There was more G3/4 nausea and vomiting with ECF/ECX and more G3/4 neutropenia with FLOT.12
Perioperative CT versus CT, then surgery, then RCT
Postoperative chemoradiotherapy (CRT) and perioperative chemotherapy (CT) have demonstrated a survival benefit over surgery alone. The randomized phase III CRITICS study (NCT00407186) investigated whether CRT after neo-adjuvant chemotherapy and adequate (D2) surgery led to improved OS in comparison with postoperative CT. Patients with Stage ≥Ib resectable gastric cancer were randomized after diagnosis. Neo-adjuvant CT was prescribed in both arms and consisted of three courses of epirubicin, cisplatin/oxaliplatin, and capecitabine (ECC/EOC). After gastric cancer resection, patients received another three courses of ECC/EOC or CRT (45 Gy in 25 fractions combined with weekly cisplatin and daily capecitabine). The 5-year survival was 41.3% for CT and 40.9% for CRT (P = 0.99). Toxicity was mainly hematological (Grade III or higher: 44 vs 34%; P = 0.01) and gastrointestinal (Grade III or higher: 37 vs 42%; P = 0.14) for CRT and CT, respectively.13
Comments
We pooled 727 patients from two phase III RCTs. There was a benefit of perioperative CT versus surgery alone on OS (HR = 0.72, 95% CI: 0.55–0.95) and on DFS (HR = 0.65, 95% CI: 0.50–0.85). Adjuvant chemotherapy was superior to surgery alone on OS and SSP (CLASSIC study HR = 0.72; CI: 0.52–1 and HR = 0.56, CI: 0.44–0.72, respectively). Adjuvant radiochemotherapy was superior to surgery alone (HR = 1.35, 95% CI: 1.09–1.66; P = 0.005). Face-to-face comparison of perioperative chemotherapy versus adjuvant chemotherapy versus chemoradiotherapy remains necessary.
Despite the potentially curative resection of stomach cancer, 50–90% patients die of disease relapse. Numerous studies have compared surgery alone with adjuvant chemotherapy, but definitive evidence is lacking. In fact, published randomized studies of adjuvant chemotherapy in gastric cancer were biased: inhomogeneous surgery (D1, D2, D0), sometimes R1 or R2 surgery, and inhomogeneous chemotherapy regimens.
In the meta-analysis by Paouletti et al., individual patient data were available from 17 trials (3838 patients representing 60% of the targeted data) with a median follow-up exceeding 7 years. There were 1000 deaths among 1924 patients assigned to chemotherapy groups and 1067 deaths among 1857 patients assigned to surgery-only groups. Adjuvant chemotherapy was associated with a statistically significant benefit in terms of OS (HR = 0.82; 95% CI: 0.76–0.90; P = 0.001) and disease-free survival (HR = 0.82; 95% CI: 0.75–0.90; P = 0.001). There was no significant heterogeneity for OS across RCTs (P = 0.52) or the four regimen groups (P = 0.13). Five-year OS increased from 49.6 to 55.3% with chemotherapy.
The conclusion of authors was that postoperative adjuvant chemotherapy based on fluorouracil regimens was associated with reduced risk of death in gastric cancer compared with surgery alone.14
To clarify the effect of neo-adjuvant chemotherapy (NAC) on the survival outcomes of operable gastric cancers, Yang et al. searched PubMed, EMBASE, and the Cochrane Library for Randomized Clinical Trials published until June 2014, which compared NAC-containing strategies with NAC-free strategies in patients with adenocarcinoma of the stomach or the esophagogastric junction who had undergone potentially curative resection. The adjusted pooled HR for OS was not significant when comparing the NAC-containing arm with the NAC-free arm. Subgroup analysis showed that the OS of the treatment arm that involved both adjuvant chemotherapy (AC) and NAC was significantly improved over the control arm (AC only) (HR = 0.48, 95% CI: 0.35–0.67; P < 0.001). However, NAC alone plus surgery did not show any survival benefit over surgery alone. Perioperative chemotherapy (PC) also showed a significant increase in PFS and a significant reduction in distant metastasis compared to surgery alone. Therefore, in patients with resectable gastric cancer, NAC alone is not enough and AC alone is not good enough to definitely improve their OS. Collectively, PC combined with surgery could maximize the survival benefit for patients with resectable gastric cancer.15 Perioperative chemotherapy with docetaxel, oxaliplatin, and fluorouracil/leucovorin (FLOT) has become the new standard of care in perioperative treatment of patients with adenocarcinomas of the stomach or gastroesophageal junction the by European Society. However, in the MAGIC trial, MMRD and MSI were associated with a positive prognostic effect in patients treated with surgery alone and a differentially negative prognostic effect in patients treated with chemotherapy. Face-to-face comparison of perioperative chemotherapy versus adjuvant chemoradiotherapy remains necessary by analyzing the microsatellite status. A limitation of this study was that the number of RCTs for each comparison was too small (about 2–3 original studies per comparison). In addition, there is major concern regarding potential and important bias due to the heterogeneity of the interventional protocol used in the different studies. Further RCTs are needed in this field.
In conclusion, perioperative chemotherapy with docetaxel, oxaliplatin, and fluorouracil/leucovorin (FLOT) significantly improved PFS and OS among patients with resectable gastric cancers compared with epirubicin, cisplatin, and fluorouracil or capecitabine (ECF/ECX). FLOT has become the new standard of care in perioperative treatment of patients with adenocarcinomas of the stomach or gastroesophageal junction by the European Society. Face-to-face comparison of perioperative chemotherapy versus adjuvant chemotherapy versus chemoradiotherapy remains necessary.




