The Man Van: A pilot study of using mobile targeted case-finding to address health inequalities in prostate cancer
Data from the project has been presented at the following conferences: American Urology Association Annual Meeting, American Society of Clinical Oncology Annual Meeting, British Association of Urological Surgeons Annual Meeting, Royal Society of Medicine Winter Short Papers Meeting.
Abstract
Early diagnosis remains a major limitation of cancer outcomes with ethnicity and deprivation being determinants of inequalities that impact outcomes. Prostate cancer suffers from lower incidence rates and higher mortality rates in the most deprived versus the least deprived groups. We developed the ‘Man Van’ to enable high-risk male patients' from deprived communities and ethnic minorities increased access to health care to address these health inequalities. Between December 2021 and December 2022 the Man Van project was piloted in eight different locations chosen using geospatial targeting based on ethnic minority populations and deprivation scores. The primary outcome measures were the prevalence of prostate cancer and other health conditions. 810 men were recruited to be seen at our Man Van clinics with 610 men attending. 48% of attendees were non-White including 30% of men who were Black. 420 men had PSA tests performed with a median PSA of 1 μg/L. 15 prostate cancers were diagnosed (3.6%; 95% CI 2.0–5.9) with 10 of these being clinically significant disease. Black men were more likely to be diagnosed compared to white men: 7.1% versus 1.8% (p < .05). The Man Van project is a novel approach to tackling health inequalities combining awareness raising, improved access to healthcare as well as ease of follow-up. Comparatively high levels of prostate cancers were diagnosed at early stages and high levels of other health conditions were found which could improve the economic value of the service.
What's New?
Men from deprived groups are at increased risk of delayed prostate cancer diagnosis. To ease access to PSA blood testing and follow-up for ethnic minority men and men in deprived communities, the Royal Marsden Hospital and Institute of Cancer Research in the United Kingdom initiated Man Van. Here, comparison with health screening in general practice shows that the Man Van model yields higher levels of prostate cancer diagnosis at early stages. Other health conditions, including hypertension and erectile dysfunction, are also readily detected. The findings highlight the utility of the Man Van model in facilitating disease detection in hard-to-reach groups.
1 INTRODUCTION
With increasing research in the advances of medical management, we are continuing to push the boundaries of what is possible for treating cancer. A major determinant of this is early diagnosis, without which improvements in cancer outcomes nationally and internationally may be limited. Ethnicity and deprivation are two key areas of inequality that are determinants of health outcomes. Improving outcomes in these groups is key to resolving health inequalities and improving overall population health.
Public health data from the United Kingdom shows that between 2018 and 2020 the least and most deprived deciles there is a 9.7-year difference in life expectancy for males and 8 years for females, and the trend is that this inequality gap is worsening.1 Deprivation is also linked to ethnicity, with certain ethnic groups being disproportionately affected by deprivation. In England, ethnic minority groups make up 15% of the total population but account for 22% of the population living in the most deprived decile.2 Deprivation is also associated with cancer outcomes, with all cancer mortality rates (per 100,000 people) in England in 2021 of 104.9 in the least deprived decile versus 149.4 in the most deprived decile.3 There is further evidence to suggest that a causal link between increasing levels of deprivation and worse cancer outcomes is affected by a later diagnosis; national data for cancer screening programmes in England for breast, bowel and cervical show decreased uptake associated with deprivation.3, 4 Reasons for poorer outcomes amongst these groups are multi-factorial and complex. Levels of education are often a factor which can impact the understanding of the disease and how to seek assistance.5 Distrust of medical organisations has also been cited as a factor.6
Prostate cancer remains the most common male cancer in United Kingdom7 and the second most common male cancer in the world.8 Survival is linked to stage at diagnosis, with five-year survival from a stage 4 diagnosis of 53% and 10-year survival only 19%, this is compared with close to 100% for stage 1 survival at 10 years.9 Approximately 24% of cases in the United Kingdom are diagnosed at stage 4.9 The scale of challenges affecting prostate cancer is not to be underestimated. The recent Lancet Commission report predicts a surge in cases world-wide from 1.4 million in 2020 to 2.9 million by 2040, with one of the key recommendation of the report being the use outreach programmes to support early diagnosis.10
Prostate cancer has both issues of lower incidence rates and higher mortality rates in the most deprived versus the least deprived groups.7, 11 The National Prostate Cancer Audit showed that the most deprived groups have a 29% higher risk of presenting with metastatic disease (when adjusted for age, ethnicity, co-morbidity score and region).12 As urinary symptoms poorly correlate with prostate cancer13 prostate cancer incidence is a representation of biological differences, health seeking behaviour and access to testing.14
These phenomena are mirrored across the world with some of the highest incidence rates found in developed countries but mortality rates are highest in the Caribbean and sub-Saharan Africa.8
Although screening has shown a persistent 20% reduction in prostate cancer mortality and a number needed to screen lower than breast cancer15, 16 two criticisms of screening are overdiagnosis and overtreatment of clinically insignificant disease. However there have been significant developments in the diagnostic pathway for prostate cancer; with pre-biopsy MRI reducing the detection of clinically insignificant disease and reducing the rates of unnecessary biopsies.17, 18 The evolution of biopsy techniques with trans-perineal biopsies has also reduced rates of sepsis and made biopsies safer for patients.19
The Royal Marsden Hospital and Institute of Cancer Research developed the ‘Man Van’ to provide improved access for health checks for high risk male patients' from deprived communities and ethnic minorities; focusing on general health and a PSA blood test for those eligible. The service is nurse-led and patients with raised PSA levels being referred directly into the standard rapid referral cancer pathways as opposed to referring back to primary care in order to reduce administrative burden and referral times. As well as improving access to healthcare and raising awareness the van may help to break barriers and reduce stigmas that affect men from having PSA checks including: fear, lack of knowledge, embarrassment.20-22 Black men and other ethnic minorities are also more likely to have co-morbid conditions such as diabetes23-25 and cardiovascular disease26, 27 and these will also be evaluated within the Man Van project.
2 METHODS
Between December 2021 and December 2022 the Man Van pilot project was conducted in eight different locations chosen using geospatial targeting based on ethnic minority populations and deprivation scores; using the index of multiple deprivation (IMD). A single van visited the following locations: community centre (Morden), construction site (Croydon), recycling centre (Croydon), primary care (GP) health centre (Croydon), Church (Croydon), Housing Association (Mitcham), Hospital (Croydon), Royal Marsden Hospital (Sutton).
Community stakeholders were approached to assist with identifying locations and the targeting of potential men. Awareness raising events were held with local charities and local churches. Information was also provided to employees through a construction company and recycling centre. The housing association informed their residents of the service as did GP practices via text messaging to their patients. GP text messages highlighted increased risk of prostate cancer in Black men and those with a family history. Initial inclusion criteria included all men over 18 to facilitate uptake of the service before this was adjusted to men over 40 after August 2022.
Patients registered their interest by either filling out paper forms with contact details or emailing the service. The patient assessment was nurse-led with a clinic co-ordinator for support.
- International prostate symptom score (IPSS) to assess urinary symptoms.
- International Index of Erectile Function (IIEF-5) to assess erectile function.
- General Anxiety Disorder-7 (GAD-7) to assess anxiety.
- Patient Health Questionnaire-9 (PHQ-9) to assess depression.
- Alcohol Use Disorders Identification Test (AUDIT-C) to assess alcohol intake.
- General practice physical activity questionnaire (GPPAQ) to assess physical activity.
IPSS and IIEF-5 questionnaires form a fundamental part of urological assessments providing crucial information related to urological symptoms, which can be related to prostate cancer or other urological aetiologies. They are also a relatively quick and inexpensive means to whether which possible symptoms may have contributed to men attending the van. Urine dipsticks were also performed to assess for urinary tract infections and haematuria. Smoking history and a family history of cancer was also sought. GAD-7, PHQ-9, AUDIT-C and GPPAQ questionnaires were not performed from November to December 2022 to reflect an increased focus of the consultations on urinary symptoms and prostate cancer.
Patients with the following risk factors were offered HbA1c blood tests: overweight BMI, elevated blood pressure, family history, South-Asian or Black ethnicity. Normal blood results were communicated to patients using text messages and a follow-up letter. Patients with abnormal results received a telephone call.
Abnormally high PSA levels or haematuria (as per NICE criteria28) were referred via two-week wait pathways directly to hospital. Visible haematuria was specifically asked as part of the assessment process as well as non-visible haematuria that was detected on urine dipstick. The referral process had agreement from other trusts at cancer alliance level with regular discussions with individual hospitals to ensure pathways were robust. All hospitals in the cancer alliance operate a pathway with a pre-biopsy multiparametric MRI scan followed by targeted and/or systematic transperineal prostate biopsies. Other abnormal results (including any red flags for other malignancies) were referred back to the patients GP. Patients with a family history of prostate cancer or high-risk due to ethnicity were also offered participation in genetic research studies.
Patients were described with respect to age (years), ethnicity, BMI, IMD rank/score, smoking status, alcohol status, PSA level (ng/ml) and HbA1c level (mmol/mol). Associations between age, PSA, cancer diagnoses, diabetes status, BMI status, ethnicity, deprivation score, smoking status and questionnaire scores were explored both descriptively and using two-sided statistical tests at the 5% significance level; 95% confidence intervals (CIs) were calculated. No adjustments for multiple testing were made given the exploratory nature of the study.
3 RESULTS
3.1 Demographics
Between December 2021 and December 2022, 810 were recruited to be seen at our Man Van clinics at a range of community settings. 610 men attended (non-attendance rate 25%). The median age of attendees was 56 years (range 26–88). 30% of men who attended were Black (full ethnicity breakdown is shown in Table 1). The median IMD score was 23.0 (range 1.5–63.8). The median IMD rank was 12,084 which is within the 4th most deprived centile.
| Age range | N | Number of PSA tests (n and %) | Average PSA (median and IQR) | White ethnicity (n and %) | Black ethnicity (n and %) | Asian ethnicity (n and %) | Other ethnicity (n and %) | Prostate cancer referrals (n and %) | Prostate cancers (n and %) |
|---|---|---|---|---|---|---|---|---|---|
| <40 | 52 | 0 (0) | N/A | 28 (54) | 10 (19) | 6 (12) | 8 (15) | 0 (0) | 0 (0) |
| 40–44 | 62 | 4 (6) | 0.6 (0.5–0.8) | 25 (40) | 22 (35) | 11 (18) | 4 (6) | 0 (0) | 0 (0) |
| 45–49 | 83 | 47 (57) | 0.9 (0.5–1.2) | 37 (45) | 33 (40) | 8 (10) | 5 (6) | 5 (6) | 4 (5) |
| 50–59 | 184 | 172 (93) | 0.9 (0.5–1.4) | 94 (51) | 66 (36) | 20 (11) | 4 (2) | 14 (8) | 4 (2) |
| 60–69 | 167 | 151 (90) | 1.2 (0.8–2.7) | 98 (59) | 48 (29) | 15 (9) | 6 (4) | 28 (17) | 2 (12) |
| 70–79 | 55 | 45 (82) | 1.5 (1.0–3.0) | 37 (67) | 3 (5) | 13 (24) | 2 (4) | 8 (15) | 5 (9) |
| 80+ | 7 | 1 (14) | 5.3 (5.3–5.3) | 2 (29) | 2 (29) | 2 (29) | 1 (14) | 1 (14) | 0 (0) |
| Total | 610 | 420 (69) | 1 (0–2) | 321 (53) | 184 (30) | 75 (12) | 30 (5) | 56 (9) | 15 (2) |
The median BMI was 27.7 kg/m2 (range 16.2–50.5); 33% were obese or severely obese. There was a suggested negative correlation between BMI and deprivation rank, where lower ranks represent increasing deprivation (Spearman's co-efficient = −0.13, p = .001).
68 men were current smokers (11.3%) smoking a median of 10 cigarettes per day (range 1–40). 228 men drank alcohol (37%), with a median alcohol intake of 12.5 unit per week (range 0.2–140). The median AUDIT-C score was 3 (range 0–12).
3.2 PSA testing and prostate cancer
Of the 413 men that were seen and aged over 50 the uptake of PSA tests was 89.3%. 33 men attended aged between 45 and 50 with Black ethnicity and the PSA uptake in this group was 93.9%. Overall 420 men had PSA tests performed with a median PSA of 1 μg/L (range 0.1–45). 56 patients (13.3% of men who had a PSA test) were referred for an elevated age-specific PSA. 48 of men (85.7% of referrals) had MRI scans of the prostate with 23 (41.1% of referrals) prostate biopsies performed. 13 prostate cancers were diagnosed through this pathway with an additional two prostate cancers diagnosed via alternate pathways (one from the haematuria pathway and one via a research pathway). No patients failed to complete the diagnostic assessment. Of the total of 15 prostate cancers diagnosed till date (3.6%; 95% CI 2.0–5.9). 10 (67%; 95% CI 38–88) of these were cancers with clinically significant disease, being grade group 2 (i.e., Gleason 7) or higher (all with >5% pattern 4 Gleason scores). The prevalence of clinically significant disease was 2.4%. Data showing PSA by age, ethnicity and cancers is shown in Table 1 with a further breakdown of data for men diagnosed with prostate cancer shown in Supplementary Table 1. Figure 1 shows a flow diagram of the prostate cancer diagnostic pathways.
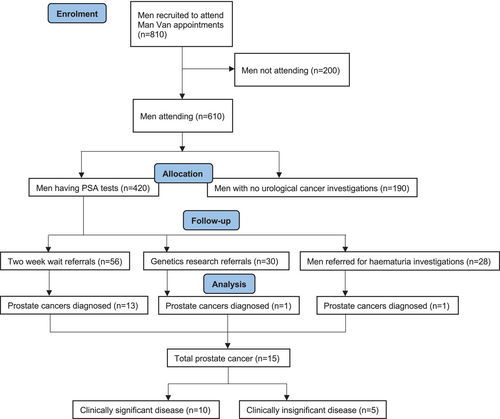
The prevalence rate for different ethnicities was: White 1.8%, Black 7.1% (Chi Squared, p < .05 vs. White), Asian 2.1%. Of patients diagnosed with prostate cancer the median age was 59 years, range 48–77. The median PSA was 6.9 μg/L (range 0.8–45). The PSA was significantly higher (Mann–Whitney U, p < .001) in men diagnosed with prostate cancer however there was no significant difference in IPSS or IIEF-5 scores between men diagnosed and those not diagnosed with prostate cancer.
One bladder (G3pT1b) and one oesophageal cancer (T3N2M1) were found incidentally. Three patients had either high-grade prostatic intraepithelial neoplasia (HGPIN) or atypical small acinar proliferation (ASAP), three patients had renal stones and one urethral stricture was found.
3.3 Haematuria
Twenty-eight patients were referred on 2-week wait pathways for haematuria. No bladder or renal cancers were found as a result of these referrals. One patient was found to have prostate cancer via this referral pathway.
3.4 Diabetes
A total of 331 HbA1c tests were performed, the median HbA1c was 38 mmol/mol (range 24–116). 13 diabetics were diagnosed (3.9% of tests) and 50 pre-diabetics (15.1% of tests). A comparative analysis showed an association of diabetes with ethnicity when assessing the following ethnic groups (Asian [N = 51] vs. both Black and White [N = 268]), based on a Fisher's exact test (p = .036).
Data on other health conditions diagnosed through the Man Van are shown in Supplementary Table 2.
3.5 Symptom scores
The median IPSS score was 6 (range 0–34) with a median quality of life score of 2 (range 0–6). The median IIEF-5 score was 20 (range 0–25). IPSS had a negative correlation with IIEF scores (Spearman's co-efficient = −0.29, p < .001) but a positive correlation with PSA (Spearman's co-efficient = 0.12, p = .019). The median PHQ-9 was 2 (range 0–26). The median GAD-7 score was 1 (range 0–21). Per the GPPAQ 40% were active, 32% moderately active, 14% moderately inactive and 14% inactive.
3.6 GP practice data
A subset of the main data was obtained of patients seen at a GP practice with corresponding baseline data from the background primary care population. A total 3295 SMS were sent from two GP practices (in partnership) with the Man Van based at one of them. 301 patients registered (9.1%) with 218 attending. Due to a communication error one practice sent SMS to men over 25 years old and the second practice as instructed to men over 40. The total population from which the SMS were sent was approximately 4000 men.3 Table 2 shows the GP practice data compared with Man Van data from men seen whilst located at the practice.
| Background GP data (n = 14,105)3 | Man Van sub-group (n = 218) | |
|---|---|---|
| Proportion White ethnicity | 72.3%a | 48% |
| Proportion Black ethnicity | 17.1%a | 33% |
| Proportion Asian ethnicity | 4.2%a | 9% |
| Proportion other ethnicity | 6.4%a | 10% |
| Average IMD score | 35.4a | 34.0 (median), range 3.1–49.6 |
| IMD decile | 2nd worsta | 2nd worst |
| Obesity prevalence | 11.1%b | 33.9% |
| Diabetes prevalence | 7.7%b | 3% (all patients) 4.3% (of HbA1c tests) |
| Non-diabetic hyperglycaemia | 5.3%b | 9.6% (all patients) 17.9% (of HbA1c tests) |
| Hypertension prevalence | 13.1%a | 21% referrals |
| Smoking prevalence | 22.4%c | 14.2% |
| Depression incidence | 2.6%b | 10.3% mental health referrals |
| Prostate cancer incidence, from 2022 (men >45 years) | 0.3% | 3.4% |
- a Data from all ages and both sexes.
- b Data from >20-year-olds, both sexes.
- c Data from >15-year-olds, both sexes.
4 DISCUSSION
In the absence of new screening studies the debate for and against prostate screening continues meanwhile the disease continues to cause morbidity and mortality around the world. In this context alternative methods to support early diagnosis of prostate cancer show relevance. Our prostate cancer prevalence rate of 3.6% (3.1% excluding two patients diagnosed on alternative pathways) compares favourably to previous studies with the first screening phase of the CAP trial having a rate of 3.3% (18-month follow-up), with 40% of these being Gleason 7 or above.29 The PLCO study had a rate of around 1.4% after one screening round30 although with a high-rate of contamination between screened and non-screened groups.
Of particular relevance is our finding of 67% grade group 2 or above disease (of which all were >5% pattern 4). The GÖTEBORG-2 study, using MRI targeted and systematic biopsies, reported 2.3% prostate cancers detected, with almost half of these (1.1%) being clinically significant disease.17
Our finding of no significant difference in urinary and erectile function symptom scores between men diagnosed with and those without prostate cancer is consistent with previous studies13 and further highlights the need to decouple urinary symptoms from prostate cancer. Rates of referral of haematuria were high and did not result in any bladder or renal cancer detections. For a further project this referral process would likely need to be revised.
Overall 30.0% of our population was Black, which shows over-recruitment from a background of 13.5% in London, the 12.2% Asian population was less than the London average of 20.7% although this group was not specifically targeted.31 Our median deprivation score of 23.0 was similar to the Croydon average of 22.5, and higher than both Sutton (14.0) and Merton (14.6).3
The lack of ethnic diversity is a major issue in prostate cancer trials.32 The ERSPC study has no ethnicity data and the PLCO study recruited only 4% of men that were Black.30 Neither has any deprivation data. The ProtecT study, now with 15-year follow-up data,33 has been pivotal in informing the safety of surveillance (or active monitoring) of low and intermediate risk men despite having less than 1% Black men.34 The dangers of extrapolating its results to Black men has been highlighted previously35 with Black men having higher rates of upstaging, biochemical recurrence and positive surgical margins post-radical prostatectomy.36-38 Our work highlights that engagement and recruitment of different ethnic groups is possible and different approaches should be considered in future trials. The addition of diagnostic tests for other cancers could also be a novel approach to targeting similar high-risk groups.
The comparison between GP data and our Man Van patients from the same cohort shows increased participation from Black and Asian ethnic minorities. This is despite the messaging targeting only Black men by ethnicity, suggesting that our approach was able to appeal to groups generally high-risk of health issues. Higher rates of obesity, pre-diabetes and hypertension are also found indicating these men may have some awareness of their health state and may be self-selecting for participation and also highlights how health inequalities affect multiple diseases.
There are several limitations to this study, which should be viewed in the context of the scale and challenges of such a project. Approximately 10% of patients responded to a single text message, compared to 46% recruitment via GPs in the CAP study.39 We did not attempt a repeat text message to non-responders but this could be explored in further studies. Engagement with high-risk groups poses challenges and this study highlights potential solutions, but a complete approach requires further evidence. Despite success in targeting high-risk and difficult to reach groups increased efforts will be required the more barriers are present. A cost-effectiveness balance will be needed to justify the long-term use of such a service. Another limitation is that at present we do not have follow-up data as to whether patients referred to primary care for further follow-up did indeed follow through with guidance and recommendations. Thus drawing conclusions regarding the effect of our intervention from a primary care perspective is limited.
5 CONCLUSIONS
The Man Van project is a novel approach to tackling health inequalities with a combined approach of raising awareness, improving access to healthcare as well as ease of follow-up. Comparatively high levels of prostate cancers were diagnosed at early stages and high levels of other health conditions were found, which could improve the economic value of the service. Further study is needed to optimise the service and better understand how it could overcome other barriers to patients accessing healthcare.
AUTHOR CONTRIBUTIONS
Masood Moghul: Conceptualization; data curation; formal analysis; investigation; methodology; project administration; resources; software; supervision; validation; visualization; writing – original draft. Amina Tran: Data curation; formal analysis; methodology; project administration; software; validation; writing – original draft. Fionnuala Croft: Conceptualization; data curation; investigation; methodology; project administration; resources; supervision. Netty Kinsella: Conceptualization; data curation; investigation; methodology; project administration; resources; supervision. Clare Peckitt: Conceptualization; data curation; formal analysis; investigation; methodology; project administration; resources; software; validation. Declan Cahill: Conceptualization; investigation; methodology; project administration; resources; supervision; validation. Nicholas D. James: Conceptualization; formal analysis; funding acquisition; investigation; methodology; project administration; resources; supervision; validation; visualization.
FUNDING INFORMATION
Funding for this study was obtained from the RM Partners Cancer Alliance.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest.
ETHICS STATEMENT
The Man Van project has ethical approval from Wales Research Ethics Committee (REC) 6.
Study title: The Man Van Project: An evaluation of the effectiveness of a mobile outreach screening clinic model for earlier detection of prostate cancer and other male cancers (REC reference: 22/WA/0113; Protocol number: CCR5573; IRAS project ID: 304320).
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.