Traumatic spinal cord injury caused by a dagger in the spine: A case report
Hong-Su Zhou and Yu Pi contributed equally to this study.
Abstract
Acute traumatic spinal cord injury (SCI) combined with foreign matter retention is rare in the clinic, which causes less literature reported, browsed, and analyzed. A 36-year-old male was rushed to our institution due to an attack on the back. His superficial sensation below the nipple had disappeared (mainly in the left breast), the proprioception of both lower limbs was obviously decreased, and the muscle strength of the left lower limb was level 0 and that of the right lower limb was level 3. Computed tomography of the thoracic vertebrae showed that the dagger had completely pierced into the T9 vertebral body and the spinal canal. Prehospital transport: the spinal cord may be injured again due to the movement of the remaining foreign matter and the posture of the patients while they are being transported. Pathophysiology: the incidence of incomplete SCI is higher than that of other types of SCI. Imaging examination: magnetic resonance imaging might cause unexpected secondary injuries. Treatments: surgical intervention including removal of foreign matter and decompression is an essential and important measure for recovery of neurological function. Patients could benefit from administration of methylprednisolone.
1 INTRODUCTION
Spinal cord injury (SCI) is defined as a disease that causes changes in spinal cord function, whether temporary or permanent, which is classified as traumatic or nontraumatic.1 Traumatic SCI exerts drastic effects on the body due to external physical factors (such as motor vehicle accidents, falling, exercise-related injury, or violence). So far, traumatic SCI events caused by violence have rarely been reported, and have been reviewed mainly in retrospective analysis or case reports.2 Thus, acute SCI combined with foreign matter retention is much rarer in the clinic, occurring in young males.3 Besides, nerve injury can be observed in and around the injured area, which has adverse effects on the physical health, social and professional life of patients. However, the pathological changes, clinical manifestations, imaging signs, and prognosis differ from the characteristics of other types of SCI.4 Therefore, the aim of this study was to report the characteristics, treatment methods, and prognosis of this type of SCI.
2 CASE REPORT
2.1 History
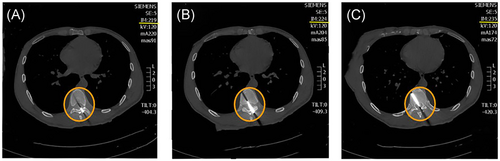
A 36-year-old male was rushed to our hospital due to an attack on his back. The wound was bleeding and the limbs were adynamic. However, there were no symptoms of coma, vomiting, and urination. Vital signs were stable, and the chest and abdomen were complete. On physical examination, the patient was found to be conscious, pale, and in a prone position on a stretcher. It was clearly visible that a dagger was stuck in the middle of the thoracic vertebra to the left (T9). The dagger was about 6 cm in length. The superficial sensation below the nipple had disappeared (mainly in the left breast), the proprioception of both lower limbs was obviously decreased, and the muscle strength of the left lower limb was level 0 and that of the right lower limb was level 3. There were no other pathological changes. Computed tomography (CT) of the thoracic vertebrae showed that the dagger had completely pierced into the T9 vertebral body and the spinal canal (Figure 1).
2.2 Surgical procedures
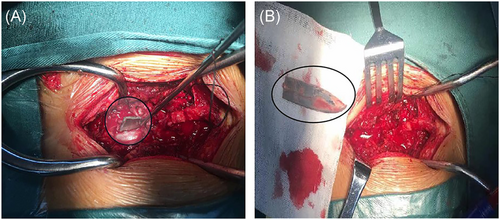
The patient was immediately sent to the emergency operating room and surgery was performed. The operation, “Debridement and Exploration for the Stabbing Wound on Back,” went on for a long time. During the operation, we found that the body pierced from the local muscles to the lamina and intervertebral ligamentum flavum of from T9 to the T10 on the near left, resulting in a gap of about 4 cm in the dura mater, and then the tip arrived at the T9 vertebral body (Figure 2A). Laminectomy and decompression were required, which included hematoma removal, hemostasis, and filling the dural incision with a human-made dural patch. Meanwhile, the dagger was removed completely (Figure 2B). Finally, the drainage tube was placed and the cut was sutured layer by layer, and the debridement was completed.
2.3 Postoperative treatments and recovery postoperative treatment
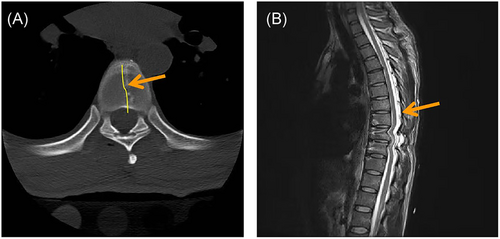
Anti-infection, nourishing nerves, and improving metabolism were important concerns in postoperative care. In addition, rehabilitation training and hyperbaric oxygen therapy for 10 days after the operation contributed to the recovery of the patient. Subsequently, the patient's physical condition and neural function were observed to gradually improve as observed from routine CT and magnetic resonance imaging (MRI) (Figure 3 and Table 1).
| Item | Preoperation | Post operation | 20 days | 60 days |
|---|---|---|---|---|
| after surgery | after surgery | |||
| SS | Disappeared | Weakened | Mild recovery | Recovery |
| TF | Weakened | Weakened | Mild recovery | Recovery |
| MS | 0 | 2 | 3 | 4 |
| Left lower limb | ||||
| MS | 3 | 4 | 4 | 4 |
| Right lower limb | ||||
| MT | / | / | Normal | Normal |
| ASIA sports score | / | / | ||
| ASIA sensory score | / | / |
- Note: SS below the nipple level; the TF in lower limbs; the GMP; MT; ASIA motor score, which grades muscle power from each myotome (i.e., a group of muscles innervated by one spinal nerve root) and the ASIA sensory score, which assesses light touch and pinprick sensation in 28 dermatomes (i.e., an area of skin innervated by one spinal nerve root), from C2 to S4 or S5.
- Abbreviations: ASIA American Spinal Injury Association; GMP, grades of muscle power; MT, muscular tone; MS, muscle strength; SS, superficial sensation; TF, the proprioception.
3 DISCUSSION
SCI caused by violent events is uncommon and can bring a heavy economic and spiritual burden for individuals, families, and societies. To our knowledge, acute SCI combined with foreign matter retention is rare in the clinic, and less literature reported, browsed, and analyzed.2 Therefore, we can treat primary and secondary injuries by reviewing and discussing the patient's prehospital transport, pathophysiology, imaging studies, and treatment. In this article, we also focus on practical, evidence-based methods that clinicians can use.
3.1 Prehospital transport
Maintaining respiratory and circulatory stability is the most urgent of all emergencies in the pre-hospital management of spinal cord injuries with foreign bodies. If improper transport causes movement of foreign bodies in the body, the injured spinal cord nerves and tissues may be secondarily damaged. Furthermore, tremors can aggravate spinal cord injury or even turn an incomplete injury into a complete injury during on-site emergency or transportation. Hence, flexion and torsion should be avoided when transporting the patient, especially foreign matter embedded deep in spine. During the process of transport, the patient's supine position should be perpendicular to the direction of the path of the foreign matter as far as possible, because the sharp part pierces from the back or side of the spine.5
3.2 Pathophysiology
The type of acute SCI often occurs in the thoracic vertebra, and only a few in the cervical, which is related to the number of thoracic vertebra and its easily exposed position. Reportedly, cervical SCI is associated with higher mortality than lumbar SCI (i.e., the risk of mortality increases with more severe injuries and higher injury levels).2 The places punctured mostly gather at the posterior median line or beside the spinous process, and are often accompanied by an outflow of bloody cerebrospinal fluid.5 The incidence of incomplete SCI is higher than that of other types of SCI, believed that the mechanism of injury is inextricably linked. The spinous process overlaps with the posterior median line, and the transverse process protrudes sideways; therefore, the sharp instrument cannot cross the midline before entering the ligamentum flavum, which affects the semilateral spinal cord in most cases. As a result, penetrating traumatic SCI secondary to gunshot and knife wounds can cause the Brown–Sequard syndrome (loss of motor function, light touch, proprioception, and vibration sensation ipsilateral to the injury, and loss of pain and temperature sensation contralateral to the injury are observed in patients with the Brown–Séquard syndrome). It is associated with destruction of the thin and wedge bundles of the ipsilateral side and the lateral corticospinal and thalamus tract of the spinal cord.
When the depth of the wound reaches the anterior spinal cord and exceeds the midline, the portion of the anterior cord may be affected. Usually, these patients are usually in the forward-flexed position, and the sharp instrument is likely to be inserted into the area between the spinous process and the lamina, which causes damage to the dural sac and bleeding, and even compression of the spinal cord. Finally, complete or incomplete lateral injury of the spinal cord may result if treatment is delayed. Fortunately, it mainly leads to nontransverse injury. The wound is smooth and neat, with little bleeding and minimal secondary injury. The severity of paralysis symptoms depends on primary SCI. Kulkarni divided SCI into three types: Type I is hematomyelia, which represents the most serious injury and has the worst prognosis; Type II is spinal edema, with faster recovery and better prognosis; and Type III is contusion, for which the time required for recovery is positively correlated with the amount of blood loss (That is, the less bleeding, the faster the recovery of major functions).6 The CT of this case showed that the fracture fragment did not occupy the vertebral canal, there was no intramedullary hemorrhage, and there was no spinal cord edema, which was the same as type II. The superficial sensation of the patient below the nipple plane disappeared, the proprioception of both lower limbs obviously decreased, the left lower limb was not completely paralyzed. We believe that this is a result of damage to the thin spinal cord bundle, wedge bundle, lateral thalamus bundle, and corticospinal tract, and the impaired neurofunctional symptoms gradually disappeared with regression of edema.
3.3 Imaging examination
In fact, the diagnosis of acute SCI caused by foreign matter is not difficult. The tips of sharp objects (such as various knives) can reach the deepest place around the injured tissue, while the injuries associated with remaining foreign matters must be highly vigilant. Therefore, assessment of the detailed history and the identification of the imaging location of foreign matter by plain X-ray or CT in the body are very important.7 Nevertheless, CT can show and pinpoint accurate localization characterization of foreign matter, its proximity, and related complications, all of which help to set the operation plan and time.8, 9 Theoretically, MRI can provide more detailed pictures (including the track and location of foreign matter, signs of intramedullary hemorrhage, metal artifacts, herniation of damaged spinal cord, dura and arachnoid formation, identification of spinal cord transection, and can assess the presence of edema and/or hemorrhage) than CT, but if the metal part of the object is pulled in a strong magnetic field, it may cause unimaginable secondary damage. To make matters worse, the patient has difficulty moving and is anxious, which can take up time and may miss the best chance of resuscitation. On the basis of the above, imaging techniques can play a significant role in treatments, assessment of the condition and prognosis, and postoperative follow-up.3, 10
3.4 Treatments
Primary injuries occur at the time of the initial injury and may include disc herniation, vertebral fractures or dislocations, penetrating injuries, and vascular abnormalities. Secondary injuries occur after the primary injury, are multifactorial, and include many pathological changes that lead to further progression of the injury.11 The Brown–Séquard syndrome is more common in patients with penetrating traumatic SCI secondary to gunshot and stab wounds. Patients with the Brown–Séquard syndrome have loss of motor function, light touch, proprioception and vibrosensory sensations on the injured side, and loss of pain and temperature sensation on the injured side. Therefore, for each open injury, especially SCI, it is very important to perform debridement and explore and remove damaged tissue and hematoma to prevent compression, infection, and other adverse effects. Spinal reduction, internal fixation, and other treatment measures that rely mainly on the imaging signs are considered. Among, there is no doubt that surgical intervene to explore foreign matters.3 In addition, the absence of foreign bodies should be determined according to the damage to adjacent tissues such as the spinal cord, intervertebral disc, and ligamentum flavum, as well as paraplegia, bleeding after hematoma formation, and fracture, and then the corresponding surgery should be performed.4 Procedures such as spinal canal exploration and hematoma removal prevent infection and also prevent foreign bodies from wandering in the body cavity or bleeding in the spinal canal, thus reducing the risk of tissue damage. In other words, the purpose of the operation is to prevent infection and discover conditions that arise from foreign matter and increase the risk of tissue damage (e.g., Bleeding of free material through the body cavity or spinal canal). In cases of violence, SCI with thoracic and abdominal injuries are mostly severe trauma; the incidence of shock is higher. Therefore, it is clear that patients with SCI with cervical or thoracic injuries and paraplegia, along with chest and abdominal injury, should be regularly examined physically to avoid misdiagnosis and missed diagnosis. Hematoma removal, foreign body removal, and release of compression on the spinal cord and its nerves, and improvement of microcirculation in the damaged tissues all significantly contribute to the recovery of spinal cord function. In brief, to solve all problems of neurological impairment, improved microcirculation of the damaged tissues is essential, which can effectively decrease the incidence of secondary injury, and contribute to overall recovery.7 More importantly, lesions that can be life-threatening, such as hemopneumothorax and massive hemorrhage owing to damage to abdominal organs, must be treated on a preferential basis; however, this may inevitably delay the treatment of spinal surgery. In general, on the basis of stable vital signs, surgical intervention of the spinal cord should be performed as soon as possible; this is very critical for the patient's prognosis. A retrospective analysis of 43 patients with neurologic spinal injuries who underwent surgical intervention within 72 h; the result indicated that early surgery may improve neurologic recovery and decrease hospitalization time.12
When dealing with foreign matter stuck in the cone plate and the vertebral body, the exposed parts need to be carefully cleaned and gently pulled out following the path of entry; sometimes, it may be necessary to break the cone to loosen it. More importantly, we should definitely avoid shaking them, which can cause unnecessary and new trauma. When there is a high suspicion for chest and abdominal cavity organ injuries, we should consider thoracotomy or exploratory laparotomy. While it is important to remove the foreign body under direct vision, it is of equal importance to repair organs damaged, relieve nervus oppressed, and repair dura upon cerebrospinal fluid being detected, clear anywhere hematoma, finish the ligation of active hemorrhage, flush the contaminated lacuna repeatedly, and then place the drainage tube. These measures can lead to a decrease in the incidence of associated complications (such as infections).7, 13, 14 Although epidural hematoma is rare for typical SCI, the possibility of epidural hematoma should be taken into account for SCI.
In addition to early spinal surgery and foreign body removal, intraoperative anesthesia and surgical manipulation are major factors in injury recovery. Important anesthetic implications include maintenance of airway stability and spinal perfusion pressure, which play an important role in the progression of SCI.15 Some cases of SCI during anesthesia are a result of the administration of anesthesia, such as spinal nerve root injury from inaccurate or inconsiderate needling during spinal anesthesia. In many cases, however, SCI during anesthesia is not always caused by the administration of anesthesia, but by improper surgical manipulation. Both direct and indirect factors, such as spinal nerve root injury due to incorrect pedicle screw placement and spinal cord ischemia after aortic surgery, are responsible for a significant proportion of SCI.16 These injuries occur during anesthesia and it cannot be determined whether they are caused by errors during anesthesia, but the effects of anesthesia on SCI cannot be denied. Moreover, it has been demonstrated that temperature can also have an effect on SCI, and subfreezing therapy can slow down the inflammatory response after SCI and also slow down the progression of neurological damage.17 Therefore, we need to pay attention to error-free operation, anesthetic behavior, and appropriate temperature during surgery to avoid secondary injuries and to ensure a healthy prognosis.
In this case, taking into account the patient's condition and what is discussed in this article, the patient was operated on within 8 hours. The results of his treatment were satisfactory. Postoperative treatments focus on the prevention of cerebrospinal fluid leakage and anti-infection measures. It is noteworthy that the patient received a therapy of methylprednisolone shock, which has been shown to benefit patients, as demonstrated by clinical trials,18 and it significantly reduced secondary injury and also yielded better therapeutic outcomes by protecting cell membrane stability, as recommended by the National Acute Spinal Cord Injury Studies Ⅲ. Ganglioside Gg (GM-1) and sodium cytidine triphosphate were used to nourish nerves and improve metabolism. In this case, rehabilitation training and hyperbaric oxygen therapy were started 10 days after surgery. Since SCI does not usually significantly affect the stability of the spine, rehabilitation should be started as soon as the patient's general condition allows. Early hyperbaric oxygen and appropriate local hypothermia therapies and rehabilitation training also play an important role and can profoundly improve activities of daily living (ADL) of patients.
4 CONCLUSIONS
All in all, we removed the contaminated wound within 8 hours and made every effort to minimize the various adverse effects of the dagger removal on the spine. It was found that the dagger had pierced the spinal lamina into the spinal canal and finally reached the spinal cord during exploration. When the tip of the dagger remaining in the vertebral body was taken away, the dura was repaired and the spine was fixed. When post-op plans based on clinical experiences and reported relevant studies were adopted, the neurological function recovered quickly and no adverse events occurred. During the follow-up, we observed that the ADL of the patient had improved significantly. Finally, although this is a rare occurrence, when it does happen it can lead to personal and even family collapse, which is a cause for concern. Therefore, the aim of this article is to emphasize again medical treatments, practice defensive strategies from admission to discharge, and contribute potentially to systematic research in the future.
AUTHOR CONTRIBUTIONS
Hao Yuan and Jun Ao performed the operations and collected the clinical data. Hao Yuan and Hong-Su completed the manuscript. Hao Yuan gave instructions on the whole process. Yu Pi developed charts and reviewed the literature. Chong Wang and Lv Sun participated in the operations. All authors have read and approved the final submitted manuscript.
ACKNOWLEDGMENTS
We thank Liu-Lin Xiong for the guidance. This study was funded by the Guizhou Provincial Department of Science and Technology [Grant number: LC (2021)002] and the Joint Fund of Zunyi Science and Technology Bureau-Affiliated Hospital of Zunyi Medical University (No. HZ2020220).
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
ETHICS STATEMENT
This research was conducted ethically in accordance with the Declaration of Helsinki and approved by the Biomedical Research Ethics Committee of the Affiliated Hospital of Zunyi Medical University (No. KLL-2020-275). The patient provided written consent to publish this case, including the use of computed tomography and magnetic resonance images.
Open Research
DATA AVAILABILITY STATEMENT
The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.