Hepatology Highlights
Potential conflict of interest: Nothing to report.
Keeping It in the (NAFLD) Family
Shirley Cohen-Mekelburg1* and Robert E. Schwartz1
Twin studies suggest a 50% heritability of nonalcoholic fatty liver disease (NAFLD) that could potentially be explained, in part, by mutations in lamin-coding genes, which have been associated with lipodystrophy. Brady et al. examined a cohort of siblings with NAFLD to identify variants in lamina-related genes. A majority of NAFLD patients had at least one variant in either ZMPSTE24, TMPO, SREBF1, or SREBF2, compared to a low frequency of mutations identified among non-NAFLD patients (P < 0.001). This study also describes the first association between TMPO/LAP2 variants and liver disease. Nuclear lamina-related gene variants have a potential impact in NAFLD, and further studies are needed to understand their role in NAFLD pathogenesis and development. (Hepatology 2018;67:1710-1725)
A Spoonful of Sugar Will Make Length of Life Go Down
Russell Rosenblatt1 and Robert S. Brown, Jr.1
NAFLD has mirrored the rise of obesity and metabolic syndrome. Allen et al. examined the impact of NAFLD on metabolic comorbidities and outcomes in a single community. NAFLD prevalence increased 5-fold from 1997 to 2014, most notably in those under 40. Those with NAFLD were at increased risk of mortality and had reduced life expectancy by 4 years. NAFLD was an independent risk factor for metabolic comorbidities, which increase the risk of mortality, but nullify the impact of NAFLD on cardiovascular disease. Thus, NAFLD remains a looming epidemic with significant impact on overall mortality and metabolic comorbidities. (Hepatology 2018;67:1726-1736)
CASPer11/4—Not the Friendly Ghost of Alcoholic Hepatitis
Russell Rosenblatt1* and Robert E. Schwartz1
While alcoholic hepatitis (AH) presents as acute on chronic liver failure and is associated with high mortality, what causes alcoholic steatohepatitis (ASH) to progress to AH remains unclear. Khanova et al. investigated this transition by using unbiased RNA sequencing and proteomic analyses on livers of recently developed AH mice to mimic this evolution in humans. Gene expression profiling identified that both Casp11 (CASP4 in humans), involved in a noncanonical inflammasome pathway, and Gasdermin-D (GSDMD), which induces pyroptosis (lytic cell death from bacterial infection) downstream of CASP11/4, were up-regulated in AH, but not ASH, mice or healthy human livers. CASP11/4 deficiency reduced GSDMD activation, bacterial load in the liver, and severity of AH in mice. Furthermore, interleukin-18, an important antimicrobial cytokine, aggravates hepatic bacterial load, GSDMD activation, and AH. Overall, pyroptosis induced by the CASP11/4-GSDMD pathway appears to be important in AH pathogenesis and may represent a new target in AH treatment. (Hepatology 2018;67:1737-1753)
Healing the Scars of the Past in NASH
Zaid H. Tafesh1* and Robert S. Brown, Jr.1
More advanced liver disease and death is more frequent in NAFLD in the presence of steatohepatitis (SH) and liver fibrosis (LF). In a phase 2b, randomized, double-blinded, placebo-controlled trial, Friedman et al. studied the efficacy and safety of cenicriviroc (CVC), a chemokine receptor antagonist targeting both inflammatory and fibrotic pathways, in 289 patients with nonalcoholic steatohepatitis (NASH) with fibrosis. Although the numbers meeting the primary endpoint (defined by histological improvement without worsening of fibrosis) at 1 year did not differ between the treatment and placebo groups, important secondary outcomes signifying improvement in fibrosis stage without progression of SH were higher in those receiving CVC (odds ratio, 2.20). Patients with more histologically advanced disease (NAFLD Activity Score ≥5 and increased hepatocellular ballooning) tended to benefit the most, and treatment was overall well tolerated. Thus, without directly modifying metabolic risk factors, targeting inflammatory pathways with CVC may alter the natural history of LF in SH, and provide a promising step forward for more advanced NAFLD. (Hepatology 2018;67:1754-1767)
The Italian Job: Personalizing HCC Care
Clara Tow2** and Robert S. Brown, Jr.1
The Barcelona Clinical Liver Cancer (BCLC) staging classification stratifies hepatocellular carcinoma (HCC) into four stages based on prognosis and responsiveness to surgical, locoregional, and systemic therapies. BCLC stage C is comprised of patients with mild-to-moderately limited performance status (PS1 and PS2, respectively), macrovascular invasion (MVI), and/or extrahepatic spread (EHS) of tumor. Sorafenib is the only currently recommended treatment for this heterogenous group of patients. Using the Italian Liver Center database, Giannini et al. subdivided BCLC stage C patients into five groups based on performance status (PS1, PS2) and tumor characteristics (MVI, EHS, and MVI + EHS) to determine prognosis and responsiveness to different treatments based on the Italian clinical practice from 2008 to 2014. Overall survival was significantly better for those with PS1 (38.6 months), and curative treatments could be successfully performed. Supportive therapy was most common for PS2 patients whereas sorafenib was the treatment of choice in MVI and EHS. Patients with the worst disease burden, MVI + EHS, received best supportive care and had a median survival of 3.1 months. These data suggest that real-world clinical practice does not follow the treatment recommendations for BCLC stage C and that because of the heterogeneity in outcome may need more personalized therapeutic considerations as well as stratified designs for clinical trials. (Hepatology 2018;67:1784-1796)
Type 2 Diabetes, the Metabolic Syndrome, and HCC: A Bizarre Love Triangle
Nicholas Russo1 and Robert S. Brown, Jr.1
To investigate the impact of type 2 diabetes (T2D) on risk of HCC, Simon et al. performed a prospective study on 120,826 women enrolled in the Nurses' Health Study and 50,284 men in the Health Professionals Follow-up Study. Over 32 years of follow-up, 112 cases of HCC were documented, and T2D was independently associated with increased risk for HCC (hazard ratio [HR], 4.59; 95% confidence interval [CI], 2.98-7.07). Increasing HCC risk was also associated with T2D duration (HR, 2.96 for 0 to <2 years, 7.52 for ≥10 years), and increasing number of metabolic comorbidities. Those with four metabolic comorbidities had an 8.1-fold increased HCC risk (95% CI, 2.48-26.7) compared to those without. Although it is difficult to analyze the impact of T2D independent of the effect of NASH from these data, it does suggest an important role of insulin resistance and the metabolic syndrome in the pathogenesis of HCC, and potentially implicates T2D in tumorigenesis perhaps through insulin-like growth factor 1 signaling. (Hepatology 2018;67:1797-1806)
Block HMGB1 and Impede the HIPPO Charge in HCC
Yecheskel Schneider3* and Robert E. Schwartz1
The Hippo pathway regulates tissue proliferation and has been suggested to play a role in tumorigenesis of HCC. Chen et al. sought to study the role of a chromosomal protein called high-mobility group box 1 (HMGB1) in the regulation of the Hippo pathway during liver tumorigenesis. The investigators found that HMGB1 depletion in hepatocytes blocks diethylnitrosamine-induced liver cancer in mice. Furthermore, shRNA-mediated gene silencing of HMGB1 inhibits HCC cell proliferation. The role of HMGB1 may be medicated by expression of yes-associated protein inducing hypoxia-inducible factor 1α. This pathway may be targeted for novel HCC therapies. (Hepatology 2018;67:1823-1841)
A Common Pathway to Liver Cancer
Vikas Gupta1* and Robert E. Schwartz1
HCC and hepatoblastoma are the most common types of liver cancers in adults and pediatric patients, respectively. These cancers develop somewhat differently; hepatocytes dedifferentiate and express fetal markers in HCC, whereas hepatic precursors never fully differentiate in hepatoblastoma. To understand the pathway of oncogenesis in these cancers, Cast et al. examined CCAAT-enhancer-binding protein alpha (C/EBPα), a transcription factor with tumor-suppressing properties when phosphorylated. They found that pediatric patients with aggressive hepatoblastoma had decreased levels of phosphorylated C/EBPα. Using a mouse model in which C/EBPα cannot be phosphorylated, the investigators could elicit the development of HCC. A close examination of preneoplastic foci within the liver revealed hepatocytes with increasingly aberrant nuclear morphologies. Those with the greatest atypical appearance were preferentially located near tumor nodules, suggesting them as the origin of cancer cells. Interestingly, they were able to find similar cells in patient samples of hepatoblastoma. This study identifies a shared pathway leading to liver cancer in HCC and hepatoblastoma, a finding sure to spur further molecular dissection of how treatment of one could affect the other in these very different, yet similar, cancers. (Hepatology 2018;67:1857-1871)
Is OCA the One for PBC?
Saurabh Mukewar2** and Robert S. Brown, Jr.1
Obeticholic acid (OCA), a farnesoid X receptor agonist, is effective in primary biliary cholangitis (PBC) patients with inadequate response or intolerance to ursodeoxycholic acid. In a randomized, controlled trial for 1 year with a 6-year open-label extension, Kowdley et al. studied the effect of OCA monotherapy at 10 or 50 mg versus placebo for 3 months in 59 PBC patients. A significant reduction in alkaline phosphatase was observed in both the OCA arms compared to placebo. Furthermore, safety and efficacy of the OCA was demonstrated in the open-label extension for 6 years. Pruritus was the main side effect leading to discontinuation of OCA in 15%-38% patients in the 10- and 50-mg groups, respectively. Monotherapy with OCA appears to be safe and effective in treating patients with PBC. (Hepatology 2018;67:1890-1902)
To Bleed or Not to Bleed in Acute Liver Failure, Will It Lead Us to Die-to Sleep No More?
Nicole T. Shen1* and Robert S. Brown, Jr.1
Using the Acute Liver Failure (ALF) Study Group Registry, Stravitz et al. investigated the relationship of liver function, bleeding events, and transfusions with clinical outcomes. Using international normalized ratio as a marker of liver injury, no relationship of bleeding events or transfusions with severity of liver injury was observed. There was a low incidence of bleeding events (10.6%; 187 of 1,770) overall, of which the majority (89%) were clinically insignificant spontaneous bleeding, most attributed to a self-limited upper gastrointestinal source (94%). Though patients with bleeding more likely had clinical features suggestive of extrahepatic organ system failure, a lower transplant-free survival was only detected in acetaminophen-induced ALF. Interestingly, patients without bleeding commonly received red blood cell transfusions—around 1 in 3 patients—and not only was this associated with the similar signs of acute illness observed in patients with bleeding, but also transfusion regardless of bleeding was associated with a nearly 2-fold higher outcome of liver transplant and/or death. These findings suggest a need for future studies to investigate the role of transfusion and hemoglobin targets in this population. (Hepatology 2018;67:1931-1942)
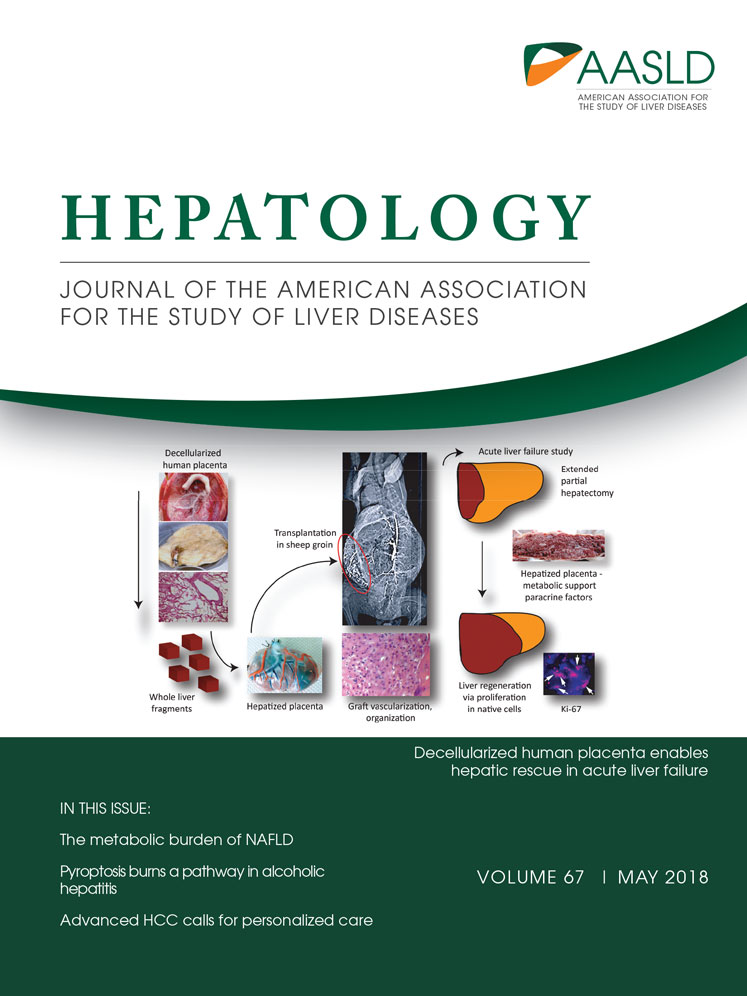
Waste Not, Want Not: Bio-waste as a New Liver
Aleksey Novikov1* and Robert E. Schwartz1
Scaffolding is a fundamental problem in bio-artificial organ development. In this article, Kakabadze et al. have created a working model of a liver by stripping sheep placenta of its cells and reseeding it with homogenized autologous liver cells. These hepatized placentas significantly prolonged sheep survival in a model of ALF, where the animals had 80% of their native livers surgically removed. The hepatized placentas had evidence of sinusoid formation composed of hepatocytes, Kupffer cells, and liver sinusoidal endothelial cells. The graft produced albumin, urea, and bile and had no evidence of cholestasis upon explantation. While imperfect—this model had no identifiable bile ducts—this is a remarkable achievement that may allow future creation of viable implantable bio-artificial livers using banked placentas, which are currently commonly discarded as bio-waste after childbirth. (Hepatology 2018;67:1956-1969)