Regression of hepatocellular adenomas and systemic inflammatory syndrome after cessation of estrogen therapy
Potential conflict of interest: Nothing to report.
Abstract
We report a case of dramatic systemic inflammatory symptoms and biochemical signs of inflammation related to multiple hepatic adenomas that completely resolved after cessation of the oral contraceptive pill (OCP) and associated adenoma regression. This represents a case of dramatic symptoms that resolved after estrogen withdrawal alone. (Hepatology 2017;66:989–991).
Abbreviation
-
- OCP
-
- oral contraceptive pill
A 43-year-old woman presented with generalized abdominal discomfort, debilitating fatigue, malaise, and intermittent night sweats in conjunction with arthralgia of both small and large joints. She had a past history of obesity and gastric stapling and was prescribed esomeprazole and the oral contraceptive pill (OCP). Clinical examination revealed mild right upper quadrant tenderness and a body mass index of 36 kg/m2. There was no fever, rash, synovitis, or palpable lymphadenopathy.
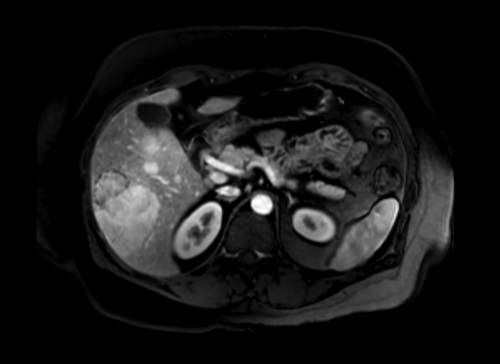
On initial investigations, erythrocyte sedimentation rate was elevated at 100 mm/hour, as was C-reactive protein at 45 mg/L. Serum albumin was low at 30 g/L, and alkaline phosphatase was elevated at 320 U/L. Liver ultrasound showed hepatic steatosis in conjunction with multiple liver lesions, the largest of which was 8.5 cm in diameter. Magnetic resonance imaging demonstrated multiple arterially enhancing liver lesions most consistent with hepatic adenomas (Fig. 1). Biopsy was not performed due to the characteristic imaging appearance.
Given the severity of systemic symptoms and elevated inflammatory markers, concerns were raised about the possibility of connective tissue disease or occult malignancy. Extensive investigations were performed, including serum vasculitic and tumor markers, positron-emission tomography, nuclear medicine bone scan, and serum protein electrophoresis. Other than a mildly positive perinuclear antineutrophil cytoplasmic antibody and microalbuminuria with preserved renal function, the remaining investigations were unremarkable.
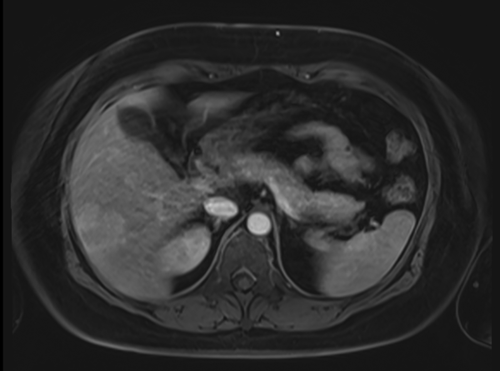
A diagnosis of adenoma-driven systemic inflammation was considered; therefore, the OCP was ceased, and lifestyle interventions were recommended to induce weight loss. Subsequent imaging revealed a steady decrease in size of the hepatic adenomas and a progressive decline of the inflammatory markers. Almost 4 years after ceasing the OCP, systemic symptoms and microalbuminuria resolved, inflammatory markers normalized, and serum albumin rose to 35 g/L. At this time, arterial enhancement of all lesions was markedly reduced and the largest adenoma had shrunk from 8.5 to 4.2 cm in diameter (Fig. 2).
Discussion
This case illustrates a rare but recognized manifestation of hepatic adenoma. The initial symptoms raised concerns about the possibility of significant systemic disease. Although histopathology was not available, the probability that the syndrome was due to estrogen-dependent hepatic adenomas was strongly supported by shrinkage of the tumors, resolution of symptoms, and normalization of inflammatory markers following cessation of the OCP.
Inflammatory hepatocellular adenomas comprise 30%-50% of all hepatic adenomas and are characterized by intralesional inflammatory infiltration and increased amyloid-A and C-reactive protein expression. Hepatocyte nuclear factor 1A–inactivated subtype comprises 35%-40% of adenomas and tends to have intratumor steatosis related to increased lipogenesis. The beta catenin–mutated subtype comprises 15% of adenomas and is associated with progression to hepatocellular carcinoma.1 In our patient, magnetic resonance imaging was strongly suggestive of hepatic adenomas, with characteristic features including arterial-phase enhancement without portal venous washout and reduced signal intensity on hepatobiliary-phase scans. The finding of diffuse hepatic steatosis in the surrounding nontumor liver suggested that the subtype was inflammatory hepatocellular adenoma because such steatosis is rare in association with other adenoma subtypes.2
Systemic symptoms have been described in patients with inflammatory adenomas; however, the syndrome appears to be rare. Previous case studies have reported systemic inflammatory presentations in young women with single large liver lesions that were confirmed to be the inflammatory hepatocellular adenoma subtype after resection.3, 4 The rapid resolution of symptoms postoperatively strongly suggested that the adenoma was solely responsible for their illness. Systemic reactive amyloidosis with associated nephrotic syndrome has also been shown to resolve following resection of an adenoma.5 In our patient, resection was precluded by the presence of multiple liver lesions, all of which had similar magnetic resonance imaging appearance. We report complete resolution of a severe hepatic adenoma–induced systemic inflammatory syndrome after cessation of estrogen therapy.