Uncommon extrahepatic metastases from hepatocellular carcinoma
Potential conflict of interest: Dr. Iavarone is on the speakers' bureau for and received grants from Bayer Spa. He is on the speakers' bureau for Gilead, Biocompatibles, and AbbVie.
Abbreviations
-
- HBV
-
- hepatitis B virus
-
- HCC
-
- hepatocellular carcinoma
-
- LT
-
- liver transplantation
-
- RFA
-
- radiofrequency ablation
-
- FDG PET/CT
-
- 18F-fluorodeoxyglucose positron emission tomography/computed tomography
-
- MRI
-
- magnetic resonance imaging
-
- mTOR
-
- mammalian target of rapamycin
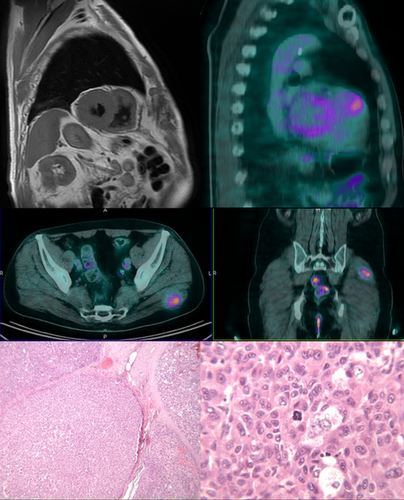
Early diagnosis of metastatic/recurrent hepatocellular carcinoma (HCC) is crucial to identify adequate therapeutic strategy. We report on the case of a patient with hepatitis B virus (HBV)-related compensated cirrhosis (Child-Pugh A5) and alphafetoprotein-negative HCC, who developed unusual HCC metastases after liver transplantation (LT) in the right ventricle and gluteus both detected with 18F-fluorodeoxyglucose positron emission tomography/computed tomography (FDG PET/CT).
Case Report
In July 2013, a 56-year-old male with multifocal HCC underwent LT after downstaging of disease with radiofrequency ablation (RFA) of a major lesion in segment 8 (28 mm) and two smaller lesions in segments 5 (10 mm) and 2 (23 mm), respectively. One month before LT, a complete response was observed at CT scan, whereas the histology of explanted liver demonstrated residual disease in segment 8 (80%-90% of necrosis), vascular infiltration, and six Edmondson grade II satellite nodules (2-5 mm) close to the primary lesion (nodules in segments 5 and 2 were necrotic). Post-LT patient continued tenofovir (started in 2011) and anti-HBV-specific immunoglobulins were added to prevent HBV relapse. Immunosuppressive therapy consisted of steroids, withdrawn after 4 months without rejection evidence, and tacrolimus (average levels, 12 ng/mL in the first 6 weeks, 10 ng/mL from week 7 to 16, and 6-8 ng/mL as maintenance). Fifteen months post-LT, the patient presented progressive exertional dyspnea. Echocardiography showed a mass at the outflow tract of the right ventricle, diagnosed as HCC metastasis at biopsy. A few months before the detection of this lesion, hepatitis B surface antigen turned positive whereas the HBV DNA remained undetectable. A palliative resection/crioablation of cardiac lesion was performed1 and sorafenib was started. One month after treatment, cardiac magnetic resonance imaging (MRI) and chest/abdomen CT scan demonstrated a persistent tissue enhancement surrounding the pulmonary valve. FDG PET/CT was then performed to restage the patient, revealing FDG focal uptake in the cardiac lesion and in the left gluteus (Fig. 1). After gluteal excisional biopsy, a second HCC metastasis with involved margins at histology was diagnosed. Eighteen months post-LT, tacrolimus was switched to everolimus (mammalian target of rapamycin [mTOR] inhibitor) and a transient stable disease at further PET/CT and CT scan was observed during follow-up. However, 34 months post-LT, metastatic mediastinal nodes and enlarged ventricular mass and residual gluteal lesion were observed at last CT scan and PET/CT, suggesting that a further different adjuvant treatment was mandatory.
Discussion
This case shows the usefulness of PET/CT in selected patients post-LT at high risk of distance recurrences. Our protocol for low-risk patients is based on repeat chest/abdomen CT scan every 6 months, whereas a CT scan for high-risk patients is usually performed every 3 months. In our patient, defined as high risk because of microvascular invasion and satellite nodules in explanted liver, frequent CT scans failed to detect extrahepatic metastases, unusually localized in the right ventricle and gluteal muscle. These lesions could be missed respectively because of contrast medium contained in the right ventricle and standard extent of the scan limited to chest and abdomen. The decision to use PET/CT to restage our patient was based on the ability of aggressive tumors to concentrate FDG, exposed in a whole-body map. Moreover, the correlations among the increase of FDG uptake and microvascular invasion and tumor growth rate of poorly differentiated HCC suggested PET/CT use.2 Focal tracer uptake in gluteal metastasis confirmed the role in surveillance of high-risk patients. FDG uptake is also an independent prognostic factor in advanced HCC patients, and it is significantly related to the overall survival under sorafenib treatment.3 After recurrence, mTOR inhibitor was early on associated with sorafenib to combine their antiangiogenic and antiproliferative effects, given that an improved survival post-LT could be expected.4 Otherwise, more recent articles seem to mitigate this enthusiasm. PET/CT scans performed during follow-up allowed the detection of a transient stable disease and a subsequent disease progression. Thus, PET/CT could be also used in planning therapy, avoiding ineffective treatments and their non-negligible side effects.
REFERENCES
Author names in bold designate shared co-first authorship.