Assessment of growth monitoring among children younger than 5 years at early childhood development centres in Nelson Mandela Bay, South Africa
Abstract
Introduction
Early childhood development (ECD) centres are important community hubs in South Africa and act as sites for community detection of childhood nutrition problems. This study aimed to assess the ability of trained ECD practitioners with optimal support to correctly classify the nutritional status of infants and young children at ECD centres in the Nelson Mandela Bay.
Methods
A descriptive, cross-sectional study was used to collect data from 1645 infants and children at 88 ECD centres. Anthropometric measurements were taken by trained fieldworkers and growth monitoring and promotion infrastructure was audited at ECD centres.
Results
Of the sample, 4.4% (n = 72) were underweight by weight for age Z-score (WAZ < −2) and 0.8% (n = 13) were severely underweight (WAZ < −3). Results showed that 13.1% (n = 214) were stunted by height for age Z-score (HAZ < −2) and 4.5% (n = 74) were severely stunted (HAZ < −3). The prevalence of moderate acute malnutrition was 1.2% and severe acute malnutrition was 0.5%, while the prevalence of overweight was 9.2% and the prevalence of obesity was 4%. A significant level of agreement between the correct interpretation and the ECD practitioners' interpretation was observed across all the anthropometric indicators investigated. The true positive wasting cases had a mean mid-upper arm circumference (MUAC) of 14.6 cm, which may explain the high false negative rate found in terms of children identified with wasting, where ECD practitioners fail to use the weight for height Z-score (WHZ) interpretation for screening.
Conclusion
By using ECD centres as hub to screen for malnutrition, it may contribute to the early identification of failure to thrive among young children. Although it was concerning that trained ECD practitioners are missing some children with an unacceptably high false negative rate, it may have been due to the fact that wasting in older children cannot be identified with MUAC alone and that accurate WFH plotting is needed. Onsite mentorship by governmental health workers may provide ECD practitioners with more confidence to screen children for growth failure based on regular WFH measurements. Moreover, ECD practitioners will be more confident to monitor the Road to Health booklets for missed vaccinations, vitamin A and deworming opportunities.
Abbreviations
-
- CHW
-
- community health worker
-
- DSD
-
- Department of Social Development
-
- ECD
-
- early childhood development
-
- FN
-
- false negative
-
- FNR
-
- false negative rate
-
- FP
-
- false positive
-
- FPR
-
- false positive rate
-
- GMP
-
- growth monitoring and promotion
-
- HAZ
-
- height for age Z-score
-
- IMCI
-
- integrated management of childhood illness
-
- MAM
-
- moderate acute malnutrition
-
- MUAC
-
- mid-upper arm circumference
-
- NGO
-
- nongovernmental organisation
-
- RtHB
-
- road to health booklet
-
- SAM
-
- severe acute malnutrition
-
- SD
-
- standard deviation
-
- SPSS
-
- statistical package for the social sciences
-
- TN
-
- true negative
-
- TP
-
- true positive
-
- WAZ
-
- weight for age Z-score
-
- WFH
-
- weight for height
-
- WHO
-
- World Health Organisation
-
- WHZ
-
- weight for height Z-score
1 INTRODUCTION
Childhood malnutrition continues to be a public health threat in sub-Saharan Africa, where approximately 27.4% of children younger than 5 years are stunted, 25% are underweight and 10% are wasted [1]. Although the prevalence of stunting in southern Africa decreased from 31.8% in 1990 to 23.3% in 2020, there are still an estimated 1.6 million stunted children in this region. Apart from underweight, wasting and stunting, childhood overweight and obesity, associated with chronic diseases of lifestyle later in life, increased to 13.5% among schoolchildren aged 6–14 years, and should be seen as a public health concern [2]. Any form of malnutrition, especially stunting, can have a substantial negative impact on a child's cognitive development before the age of five, depriving them of the ability to reach their full potential and thrive in school [3].
Growth monitoring and promotion (GMP) is a nutrition surveillance strategy which is carried out in communities for early detection of childhood growth faltering [4]. Malnourished children are usually identified in the community by trained community health workers (CHWs), used in developing countries to address the shortage of skilled health workers [5]. The full assessment should include mid-upperarm circumference (MUAC) measurement, plotting and interpreting weight for height, an examination of oedema, a clinical examination for Integrated Management of Childhood Illnesses (IMCI) danger signs and an appetite test [6]. However, CHWs lack adequate training, require better supervision and essential resources, and are sometimes inhibited from performing stabilisation care before referral due to restrictive policies [7]. As a result, in most areas in South Africa, screening by CHWs only include measurement and interpretation of MUAC and to assess for the presence of oedema, followed by referral to the nearest primary health care centre.
The space where children are cared for, often while their parents are at work or looking for work, are in early childhood development (ECD) centres, sometimes referred to as creches/preschools. In South Africa, approximately 1.6 million children are enroled in more than 42,000 ECD programmes [8]. It therefore makes sense for CHWs to include these centres in the outreach work to screen for malnutrition. Eliminating all malnutrition in children is an ambitious goal and should be a priority to multiple stakeholders including those working in education, health- and social development fields [9].
This study aimed to assess the ability of a nutrition-trained ECD practitioner with optimal support to correctly classify the nutritional status of infants and young children at ECD centres in the Nelson Mandela Bay. A sub-objective was to assess the growth monitoring practices performed at the ECD centres in the sample.
2 METHODS
2.1 Study design
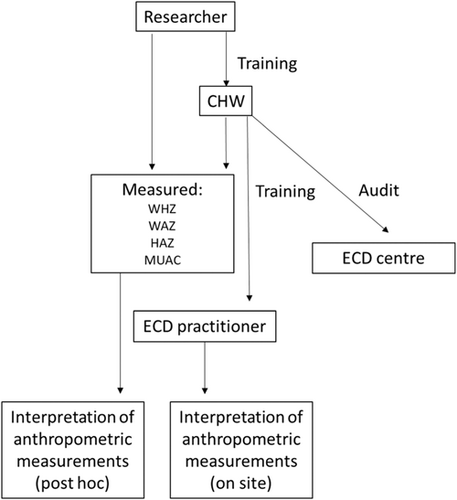
This study used a descriptive, cross-sectional design. Data were collected from 93 ECD centres in Motherwell, Nelson Mandela Bay between May 2017 and May 2018. ECD practitioners received nutrition mentorship from an NGO nutrition-trained CHW (Figure 1). The CHW conducted site visits over a 9-month period which started in May 2018 to screen children for malnutrition, as well as train, assess and support ECD practitioners with regard to growth monitoring at ECD centres. The average number of children per centre was 47.3, with an average of 3.5 teachers. This resulted in a teacher-to-child ratio of 1:13.5.
2.2 Data collection
CHWs were trained to take anthropometric measurements by an experienced, registered dietitian. Children were weighed by the field worker using a Seca electronic scale (Model 813) according to standardised procedures [6]. Weight was measured in kilograms (kg) to the nearest 0.1 kg. The fieldworkers also measured the height of children using a portable stadiometer (Seca model 213) using standardised procedures. Height was measured in centimetres (cm) to the nearest 0.1 cm. Mid-upper arm circumference was measured according to standardised procedures [6], measured in centimetres (cm) to the nearest 0.1 cm.
Weight and height were physically plotted onto the road to health booklet (RtHB) clinic cards and growth charts on site by the ECD practitioner. Weight for age Z-score (WAZ), height for age Z-score (HAZ) and weight for height Z-score (WHZ) were plotted.
Data were collected using a Google form on tablets. The forms were extracted to a Microsoft Excel spreadsheet and saved to a password protected Google Drive folder. Height, weight, MUAC, WAZ, HAZ and WHZ were captured using the form, in addition to the ECD practitioners' interpretation of the anthropometric measurements. The age of the children was calculated as the difference in months between the date of visit and child's date of birth as recorded from the clinic card. The gender of the child was captured to ensure use of the correct growth chart.
The field workers were trained to collect audit data from the ECD centres. This data included immunisation, deworming and vitamin A supplementation history from children's clinic card, as well as the availability of a height chart in the centre, whether the ECD practitioners were measuring and interpreting the height of children, whether ECD practitioners were able to measure and interpret MUAC and whether children were checked for oedema. ECD centre practitioners were interviewed about their referral to local clinic behaviour when malnutrition was detected.
2.3 Data analysis
The researchers then proceeded to recalculate the WAZ, HAZ and WHZ from the actual measurements using Anthro software [10]. These data were cleaned according to the World Health Organisation (WHO) [11] criteria. Participants with WAZ, HAZ or WHZ more than five standard deviations from the median were excluded from the analysis as these measurements are physiologically implausible and are more likely to be the result of measurement or data capture errors. Children with missing Z-scores were removed from the data set.
WAZ, HAZ and WHZ were classified according to WHO criteria. For the purposes of comparison between the ECD practitioners' classification and measured anthropometric classification, WAZ < −2 was classified as underweight, HAZ < −2 was classified as stunted, WHZ < −2 was classified as wasted and WHZ > +2 was classified as overweight.
The ECD practitioners' interpretations of participant nutritional status were analysed and also used to generate classifications of underweight, stunted, wasted and overweight. Children described as ‘growing well’ were not classified as either underweight, stunted, wasted or overweight.
Data were analysed using SPSS v28 [12]. Data were described using means and standard deviations (SD) for continuous data, and frequencies and relative frequencies for categorical data. χ2 tests were used to determine the level of agreement between the correct interpretation of anthropometry and ECD practitioner interpretations. Cohen's kappa statistic (k) was used to determine the strength of the agreement with significance set to p < 0.05. True positive (TP), false positive (FP), false negative (FN) and true negative (TN) values were calculated for the interpretations of weight for age, height for age and WHZ. The false positive rate (FPR) was calculated as FPR = FP/(FP+TN) and the false negative rate (FNR) was calculated as FNR = FN/(TP+FN). Sensitivity was calculated as sensitivity = TP/(TP+FN) and specificity was calculated as specificity = TN/(TN+FP). Figures were generated using RStudio [13].
2.4 Ethics
Ethical approval was obtained from the Nelson Mandela University Human Research Committee. Gatekeepers' permission was obtained from the Eastern Cape Department of Health. The study followed the ethical principles laid out in the Declaration of Helsinki [14]. Informed consent forms were signed by parents of participating children in advance of the study visit. Where cases of malnutrition were identified by fieldworkers, children were referred to the nearest clinic using a clinical referral form. Referral forms were given to the child's parents and follow-up visits were conducted by fieldworkers.
3 RESULTS
The total sample included data for 2396 infants and young children. For the purpose of this paper, 690 participants were removed as they had missing data. A further 53 participants were removed as they had implausible Z-scores. Finally, six records were removed as duplicate data. The final sample contained data for 1645 infants and young children.
The mean age (SD) of the participants was 42.05 months (12.06). The median age was 43.9 months. Approximately half of the sample was male (51.2%, n = 842). The mean (SD) WAZ −0.12 (1.2), the mean HAZ was −0.96 (1.26) and mean WHZ was 0.62 (1.28). Of the sample, 4.4% (n = 72) were underweight (WAZ < −2) and 0.8% (n = 13) were severely underweight (WAZ < −3). Results showed that 13.1% (n = 214) were stunted (HAZ < −2) and 4.5% (n = 74) were severely stunted (HAZ < −3). Moderate acute malnutrition (MAM) was prevalent among 1.2% (n = 19) of the children, while severe acute malnutrition (SAM) was prevalent among 0.5% (n = 8) of the participants. Of the total sample, 9.2% (n = 151) of the children were classified as overweight and 4.0% (n = 66) were in the obese category according to their WHZ.
A significant level of agreement between the correct interpretation and ECD practitioners interpretation was observed across all the anthropometric indicators investigated (Table 1). The level of agreement for wasting was lower than other indicators (k = 0.463), with the highest level of agreement observed for overweight (k = 0.769).
| Anthropometric classification | Measurer | N (male/female) | % | X2 d.f. p | k |
|---|---|---|---|---|---|
| Underweight | Researcher | 81 (40/41) | 5.7 | 663.285 | 0.687 |
| ECD practitioner | 89 (33/56) | 6.3 | 1 | ||
| <0.001 | |||||
| Stunted | Researcher | 246 (128/118) | 17.5 | 631.648 | 0.669 |
| ECD practitioner | 277 (126/151) | 19.7 | 1 | ||
| <0.001 | |||||
| Wasted | Researcher | 27 (14/13) | 1.9 | 303.747 | 0.463 |
| ECD practitioner | 32 (11/21) | 2.2 | 1 | ||
| <0.001 | |||||
| Overweight | Researcher | 199 (109/90) | 14.2 | 836.615 | 0.769 |
| ECD practitioner | 231 (127/104) | 16.5 | 1 | ||
| <0.001 |
FP rates and FNRs are presented in Table 2. The FP rate for wasting was 1.3%, but the FNR for wasting was 52%. The FP rate is low across all anthropometric measurement interpretations, however, the FNR is high for underweight for age, stunting, wasting and overweight. The FNR is higher in younger children for underweight and stunting and appears to be more consistent across age groups for wasting and overweight.
| Indicator | Interpretation | Age (years) | True positive | False positive | False negative | True negative | False positive rate | False negative rate | Sensitivity | Specificity |
|---|---|---|---|---|---|---|---|---|---|---|
| Weight for age | Underweight | ALL | 60 | 21 | 29 | 1292 | 0.016 | 0.32 | 67.42 | 98.40 |
| 0–6 | 0 | 0 | 0 | 5 | 0 | - | - | 100.00 | ||
| 6–12 | 1 | 0 | 1 | 15 | 0 | 0.5 | 50.00 | 100.00 | ||
| 12–23 | 4 | 0 | 0 | 122 | 0 | 0 | 100.00 | 100.00 | ||
| 24–35 | 16 | 11 | 5 | 295 | 0.036 | 0.238 | 76.19 | 96.41 | ||
| 36–48 | 18 | 10 | 9 | 513 | 0.019 | 0.333 | 66.67 | 98.09 | ||
| >48 | 19 | 8 | 7 | 539 | 0.0146 | 0.269 | 73.08 | 98.54 | ||
| Height for age | Stunted | ALL | 191 | 86 | 55 | 1072 | 0.074 | 0.22 | 77.64 | 92.57 |
| 0–6 | 1 | 0 | 1 | 3 | 0 | 0.5 | 50.00 | 100.00 | ||
| 6–12 | 3 | 1 | 2 | 11 | 0.083 | 0.4 | 60.00 | 91.67 | ||
| 12–23 | 16 | 4 | 13 | 93 | 0.041 | 0.448 | 55.17 | 95.88 | ||
| 24–35 | 52 | 19 | 22 | 234 | 0.075 | 0.29 | 70.27 | 92.49 | ||
| 36–48 | 55 | 28 | 31 | 436 | 0.06 | 0.36 | 63.95 | 93.97 | ||
| >48 | 59 | 34 | 20 | 460 | 0.06 | 0.25 | 74.68 | 93.12 | ||
| Weight for height Z-score | Wasted | ALL | 13 | 18 | 14 | 1359 | 0.013 | 0.52 | 48.15 | 98.69 |
| 0–6 | 0 | 0 | 0 | 5 | 0 | - | - | 100.00 | ||
| 6–12 | 1 | 0 | 0 | 16 | 0 | 0 | 100.00 | 100.00 | ||
| 12–23 | 0 | 0 | 1 | 125 | 0 | 1.0 | 0.00 | 100.00 | ||
| 24–35 | 2 | 4 | 5 | 316 | 0.0125 | 0.714 | 28.57 | 98.75 | ||
| 36–48 | 6 | 5 | 6 | 533 | 0.009 | 0.5 | 50.00 | 99.07 | ||
| >48 | 4 | 9 | 1 | 559 | 0.015 | 0.2 | 80.00 | 98.42 | ||
| Weight for height Z-score | Overweight | ALL | 177 | 54 | 27 | 1144 | 0.045 | 0.13 | 86.76 | 95.49 |
| 0–6 | 1 | 0 | 0 | 4 | 0 | 0 | 100.00 | 100.00 | ||
| 6–12 | 5 | 0 | 1 | 11 | 0 | 0.166 | 83.33 | 100.00 | ||
| 12–23 | 31 | 3 | 6 | 86 | 0.033 | 0.162 | 83.78 | 96.63 | ||
| 24–35 | 30 | 15 | 7 | 275 | 0.052 | 0.189 | 81.08 | 94.83 | ||
| 36–48 | 48 | 17 | 13 | 472 | 0.035 | 0.213 | 78.69 | 96.52 | ||
| >48 | 55 | 20 | 12 | 486 | 0.039 | 0.179 | 82.09 | 96.05 |
- - indicates undefined.
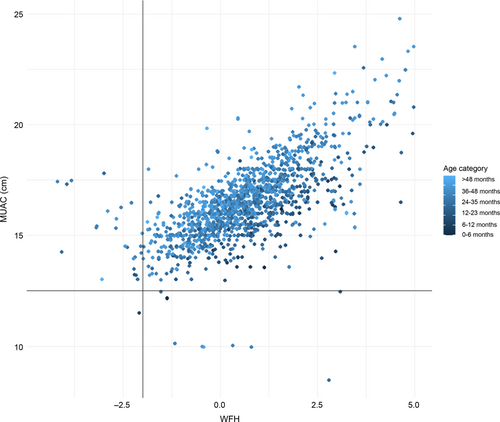
Figure 2 displays MUAC (cm) plotted against WHZ for the children in the sample, disaggregated by age group. The mean MUAC among children identified as TP wasting cases by WHZ was 14.6 cm (n = 14), while the mean MUAC for FP cases was 15.35 cm (n = 11) and for FN cases was 15.51 cm (n = 9). The mean MUAC for TP cases of wasting identified by WHZ was 18.0 cm (n = 1573). More cases of MAM and SAM were identified by WHZ than MUAC, and only one child in this sample was positive for both indicators. An age bias for MUAC is apparent in the figure, with darker plots representing younger infants and children towards the lower part of the cluster, and lighter plots representing older children towards the top.
Three out of 88 ECD centres monitored the deworming and vitamin A supplementation of children, and clinic cards were available at 17 of 73 ECD centres, as shown in Table 3. Half of nutrition-trained ECD practitioners were capable of carrying out a MUAC measurement. It was found that 54 of 88 ECD centres had a height chart available, but that height was measured by a trained ECD practitioner in only 17 of 88 ECD centres, as shown in Table 3.
| RtHB available | Deworming checked | Vitamin A checked | Height chart available | Height measured by practitioner | Check for oedema | Practitioner able to do MUAC | |
|---|---|---|---|---|---|---|---|
| No | 73 | 85 | 85 | 35 | 67 | 68 | 45 |
| Yes | 17 | 3 | 3 | 54 | 17 | 22 | 45 |
| Partially | 0 | 2 | 2 | 1 | 1 | 0 | 0 |
| Total | 90 | 90 | 90 | 90 | 85 | 90 | 90 |
4 DISCUSSION
The results of this study suggest that trained ECD practitioners are capable of classifying the nutritional status of children at ECD centres in Nelson Mandela Bay when optimal support is available. Agreement between anthropometric interpretations of the researcher and ECD practitioner was statistically significant, however, there was a range in the level of agreement across the anthropometric indicators.
FPRs across all indicators of nutritional status were low, suggesting that few infants and young children will be inappropriately referred to a health centre for treatment. FPs are likely to be discharged back into the community on full assessment, incurring transport and opportunity costs for caregivers and undermining confidence in the health system [15]. However, there was a high FNR for WFH, while half of trained ECD centres were able to measure MUAC and a third of ECD centres were monitoring children for oedema. Therefore, the accuracy of all three acute malnutrition screening practices recommended by the WHO [6] is likely to be compromised in this setting. The MUAC values for children identified as wasted by WHZ were higher than the WHO cut-off value for moderate wasting (12.5 cm). Therefore it is likely that these children would be missed by MUAC in this setting. While there is an inherent age-bias in MUAC, in which infants and younger children have smaller arms and are therefore more likely to be identified as malnourished, the data from this sample suggests that even younger infants and children appear not acutely malnourished by MUAC. It may also be that older children with higher MUAC are more difficult for the ECD practitioners to screen and because their arms are thicker they do not look like children with low Z-scores, making them more difficult to detect.
Despite the good level of agreement between researcher and ECD practitioner interpretation of HAZ, the FNR for stunting was 22%. Laar et al. [16] found that there was a moderate level of agreement in height measurements taken by CHWs and experienced measurers in Ghana. However, these researchers noted that errors were more likely to occur in measurements in crowded GMP sites and when health workers are overburdened [16]. Height charts were available in the majority of ECD centres included in the study, however, height was measured by a trained ECD practitioner in only 16 of the 84 centres. While the accuracy and frequency of height measurements of children in South African health settings is poor, a culture shift is required to address the double burden of malnutrition facing the country. South Africa has agreed to the Sustainable Development Goals, including goal 2.2, to end all forms of malnutrition, including stunting and overweight. While the country is on track to meet its targets for wasting, it is showing no progress or even a worsening situation with regard to stunting [17]. Currently, nutrition surveillance in South African secondary settings classifies children as SAM, MAM or not acutely malnourished, resulting in stunting and overweight lacking priority with the South African Department of Health. In addition, there is a lack of policy in place for treating stunting in children when it is identified. Fink and Rockers [18] have found that stunting during childhood is associated with diminished cognitive development and poorer schooling outcomes in later adolescence. Stunting has been associated with reduced human capital and intergenerational poverty [19]. While prevention of nutritional disorders and malnutrition and the associated developmental delays has been emphasised in the literature, researchers have also begun to suggest that the focus should shift from basic child survival towards thriving [19]. Therefore, Black et al. [20] have identified enabling environments as well as proximal components including safe and nutritious food, health care and learning opportunities as important parts of improving child survival, as well as ensuring that children grow and develop to meet their full potential [20].
In the current study, it was noted that only one ECD centre made referrals to the health service when a child was identified as malnourished. Reasons for the low rate of referrals by the ECD centres included ECD practitioners being too busy with educational activities, sporadic attendance at the ECD centre by children, and ECD practitioners preferring to wait for the CHW or nurses to complete the referral process. ECD practitioners also reported forgetting how to plot the growth charts as a barrier to making referrals. Similar limitations were noted by Blaauw et al. [21], where inadequate training, staff shortages and limited time were factors contributing to suboptimal use of the clinic cards among CHWs and healthcare workers. Based on the findings of Woldie et al. [22], CHWs can deliver high-quality services, but their performance on complex tasks, such as diagnosis and counselling, tends to be actioned in practice at a lower standard and requires intentional support and training to achieve an adequate certain level of competency.
Biersteker et al. [23] identified that the National Department of Social Development (DSD), Basic Education and the Department of Health are the core governance pillars of the ECD sector. Collaboration is required between these departments to address the multidisciplinary nature of malnutrition. Closing the referral system link between the ECD centres which are now governed by the Department of Basic Education and the Department of Health primary health facility. It has been suggested that improved supervision of CHWs may improve their effectiveness [21]. Feroz et al. [24] have recommended the use of mobile phones to improve support and supervision for CHWs. However, these authors noted that problems with network connectivity and technical support can confound this approach [24]. It is important to consider that these forms of supervision and support may be less available to unregistered centres, who receive limited support from state authorities. Also in this study, the ECD practitioner had good support and mentorship which did not result in a better outcome in terms of reducing the FNRs in identifying wasting which warrants further investigation.
CHW have been referred to as a critical component of the South African health care system and are praised for their status within the community for their ability carry both indigenous knowledge and service community health issues at local level [25, 26]. ECD centres play a critical within local communities by providing parents and children with support regarding education and health and social protection [27]. ECD Practitioners may not be CWH, however, there are some similarities in the status they hold embedded within communities as teachers and caregivers trained in messages related to ECD.
The nutrition screening function described in this article could be fulfilled by community-based individuals such as ECD practitioners and this supportive role enhances public health initiatives and can drive screening at a local community level [28]. A case study example of this occurring in practice is South African, Zero2Five Trusts' Mbizana stop stunting campaign 2020 using anthropometric measures of children at ECD centres to demonstrate how ECD practitioners, CHWs and local clinics can work together to improve child nutrition in their communities [29]. To appreciate the nature of this integrated discussion, one acknowledges the multidisciplinary nature of ECD and the ability for child health to fit comfortably under the umbrella of ECD. A shared responsibility for addressing the malnutrition crisis is a practical approach that is appropriate in developing countries where public health issues are complex and multidisciplinary in nature. Acknowledging the diverse scope of ECD and child well-being as a fundamental element of the nurturing care framework necessary for young children that advocates for a collaborative approach, thereby creating partnership pathways for a practical and efficient strategy to tackle the malnutrition crisis in developing nations with complex public health issues.
5 CONCLUSION
This study aimed to assess the ability of trained ECD practitioners to correctly classify the nutritional status of infants and young children at ECD centres in the Nelson Mandela Bay and to quantify the nutrition screening practices at ECD centres in this community. The results of this study suggest that child health services can be promoted and encouraged by ECD centres, but require regular visits and support from local clinic staff. The link to local clinic staff requires active human resourcing and commitment to the community linkages by the Department of Health. Growth monitoring is difficult to implement in the absence of skilled support staff to assist with nutrition screening and referral. ECD centres are useful sites for community detection of malnutrition. In addition, overweight and obesity are prevalent in this community, but the opportunity for intervention is missed as this nutritional state is not captured or prioritised by the Department of Health. Onsite mentorship by the CHW proved valuable support for ensuring that key health messages were correctly understood and implement. However, an NGO cannot provide sustainable support and it is important that the Department of Health provide staff to become mentors to the ECD practitioners.
AUTHOR CONTRIBUTIONS
Shawn W. McLaren: Formal analysis (lead); visualisation (lead); writing—original draft (lead); writing—review and editing (equal). Liana Steenkamp: Conceptualisation (lead); data curation (lead); formal analysis (supporting); funding acquisition (lead); investigation (lead); methodology (lead); project administration (lead); writing—review and editing (equal). Jessica Ronaasen: Formal analysis (supporting); investigation (equal); methodology (supporting); validation (supporting); writing—original draft (supporting); writing—review and editing (equal).
ACKNOWLEDGMENTS
The authors would like to thank Nelson Mandela University, London Metropolitan University and UNICEF.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
Ethical approval was obtained from Nelson Mandela University Human Research Ethics Committee.
INFORMED CONSENT
Informed consent forms were signed by parents of participating children in advance of the study visit.
Open Research
DATA AVAILABILITY STATEMENT
Data are available on request from the authors.