Diagnostic yield of utilizing 24–72-hour video electroencephalographic monitoring in the diagnosis of seizures presenting as paroxysmal events in resource-limited settings
Abstract
Objective
Long-term video electroencephalogram monitoring (LTVEM) is a standard practice in epilepsy centers to diagnose and characterize paroxysmal events. With the lack of data on LTVEM in Africa, we aimed to determine the clinical yield of LTVEM performed for 24–72 h to diagnose seizures in an epilepsy center in Nigeria.
Methods
This was a retrospective review of all patients admitted to our Epilepsy Monitoring Unit (EMU) from September 2018 to September 2021, with monitoring lasting between 24 and 72 h. We reviewed the patients' seizure semiology, time to the first event, and final diagnosis. The frequency of seizures was classified as “daily” in patients with one or more seizures per day, “persistent” in patients with less than one seizure per day but at least once in 6 months, and “rare” in patients with less than one seizure in 6 months. Patients with unclear duration due to recent onset were classified as “undefined”.
Results
Seventy patients (34 males, 36 females) were included in our study. The mean age was 22.86 ± 18.00 years. The average duration of monitoring was 44.23 ± 16.16 h. Fifty-seven patients (81.4%) were confirmed to have seizures. Thirteen patients experienced non-epileptic events. Of these 13 patients, nine were diagnosed with psychogenic non-epileptic spells (PNES). Two patients were diagnosed with essential myoclonus and two patients were diagnosed with syncope. The time to the first interictal epileptiform discharge was within 8 h. In the first 24 h, 56 of 57 patients had ictal and interictal discharge (98.2%). These included 100% daily seizures, 100% persistent seizures, and 100% undefined events. One rare seizure was observed within 48 h.
Significance
The diagnostic yield of the LTVEM in well-selected patients for seizures in this study is 81.4%. Most patients received a diagnosis within 48 h of monitoring, and we found that extending the study beyond 72 h may not offer significant additional benefits in diagnosing seizures in patients presenting with paroxysmal events.
Plain Language Summary
There is limited information about the usefulness of long-term video electroencephalogram (EEG) monitoring in diagnosing seizures in Africa. Several conditions that resemble seizures (paroxysmal events) could be misdiagnosed, leading to inappropriate treatment. This study evaluated the effectiveness of 24- to 72-h video EEG monitoring in diagnosing seizures at an epilepsy center in Nigeria. Among 70 patients, 81.4% were diagnosed with seizures, with most diagnoses made within 48 h. The findings suggest that video EEG performed within 48 h can significantly help distinguish seizures from other paroxysmal events, thereby contributing to better management and outcomes.
Key points
- High diagnostic yield: LTVEM achieved an 81.4% diagnostic yield in identifying seizures in low-resource settings.
- Effective in 48 H: A total of 98.2% of epileptic events were detected within the first 24 h; all were captured by 48 h.
- Shorter monitoring feasible: Extending LTVEM beyond 72 h offers minimal additional diagnostic benefit in low-resource settings.
- Cost-effective in low resources: LTVEM's time frame is practical and cost-efficient for accurate diagnoses in resource-limited settings.
1 INTRODUCTION
Long-term Video Electrographic Monitoring (LTVEM) has been commonly used in neurology and epilepsy for over three decades.1-3 The indications and importance include but are not limited to, making a diagnosis of epilepsy and non-epileptic spells, correctly identifying seizure type in those diagnosed with epilepsy, localization of identified seizures, and treatment optimization.2, 3 Due to the brief and intermittent manifestation of seizures, a standard 30–60-min electroencephalogram often fails to show epileptiform activities, as such LTVEM is the gold standard to provide a definitive diagnosis.4-8 Its use in clinical practice has become increasingly important as clinical history is reliant on the patient and observer.9, 11
The duration of LTVEM varies widely among epilepsy centers around the world12 and depends on clinical indication.13 Some studies required an average of 5–7 days,15, 16 while others required 48 and 72 h for epileptic and non-epileptic events, respectively.17-19
LTVEM is a high-cost, time-consuming, and personnel-consuming procedure.7, 14 A comprehensive unit requires a highly trained multidisciplinary team including neurologists, epileptologists, neurosurgeons, psychiatrists, nursing staff, well-trained EEG technologists, and expensive equipment.8, 9 Daily monitoring comes at a significant cost to the patient. Therefore, it is important to ensure the judicious use and diagnostic value of this expensive procedure, particularly in resource-limited settings.
Despite the cost of LTVEM, an accurate diagnosis with efficient use of time and resources can minimize net expenditure on healthcare. Many studies have evaluated the diagnostic value in different ways, with varying end points including the percentage of patients in whom the diagnosis was changed, in whom non-epileptic events were recorded, those whose diagnoses were left uncertain, and the time to first interictal epileptiform discharge.7, 8, 10-12
This study aimed to evaluate the diagnostic utility of 24–72-h video electroencephalography in the diagnosis of seizures in paroxysmal events by comparing the frequency of seizures and the time taken to capture the first interictal epileptiform discharge in our population.
2 METHODS
2.1 Study design
We retrospectively reviewed 70 patients admitted to the Regions Stroke and Neuroscience Hospital, Imo State, a large epilepsy center in Southeastern Nigeria. This facility is located approximately 5 km from the center of the capital city of Owerri, Imo State. This advanced high-volume center receives patients from the entire southeast and other regions of the country.
2.2 Study setting
The Epilepsy Monitoring Unit (EMU) at Regions Hospital is a specialized facility with a 1-bed unit and an outpatient EEG room, equipped with three Caldwell Easy III EEG machines. The workflow begins with the careful selection of patients based on clinical criteria, followed by continuous video EEG monitoring over several days. EEG Tech provides 24-h coverage and manages the equipment, ensuring high-quality recordings. The Nurses provide bedside clinical care to the patients such as checking their vitals and informing the doctors of any clinical change. The doctors, typically medical officers, round on the patients daily and report to the epileptologist, a U.S. board-certified neurologist with a fellowship in epilepsy, who provides clinical supervision, interprets the EEG, and formulates a management plan for the patients based on the EEG results. Each study is divided into 8-h segments that are downloaded over a shared drive, reviewed, and interpreted by the Epileptologist to guide diagnosis, treatment, and follow-up care.
2.3 Sample
All patients who had LTVEM in the EMU between September 2018 and September 2021 were included in this study. Patients who were monitored for seizures in the ward, emergency, or intensive care unit were excluded. All patients signed a consent form for teaching and research purposes on admission to the EMU.
2.4 Measures
All patients in this study were carefully selected from a specialized epilepsy clinic. Long-term video EEG was offered to those with appropriate indications. When finance was prohibitive to obtain the study, we prioritized the patients most likely to benefit from the study, focusing on the nuances of their clinical presentations and the semiology of their spells. For instance, in cases where patients were clinically suspected of having psychogenic non-epileptic seizures (PNES) on multiple antiseizure medications without control, and who cannot afford the study, we opted not to proceed with long-term video EEG. Instead, we offered alternative approaches, such as psychotherapy, discontinuation of antiseizure medications, and continued follow-up at the epilepsy clinic.
Based on the history and review of clinical notes, the frequency of seizures was noted and classified into daily, persistent, rare, and undefined. Patients with one or more seizures per day were classified as “daily;” those with less than one seizure per day but at least once in 6 months were classified as “persistent,” while those with a frequency of seizures less than once in 6 months were classified as “rare.” “Undefined” was reserved for patients with unclear durations, see Table 1. This was adapted from the study by Lee et al.10
The demographic and clinical characteristics of the participants were also recorded (Table 1). The patients underwent detailed physical examination on admission and comorbidities were noted. Baseline tests of complete blood counts and electrolytes were conducted to exclude any metabolic or hematologic conditions.
| Frequency (n) | Percentage (%) | |
|---|---|---|
| Gender | ||
| Male | 34 | 48.6 |
| Female | 36 | 51.4 |
| Presenting complaints | ||
| Focal jerking | 11 | 15.7 |
| Generalized jerking only | 22 | 31.4 |
| Generalized stiffening only | 6 | 8.6 |
| Generalized jerking and stiffening | 9 | 12.9 |
| Loss of speech | 2 | 2.9 |
| Starring spells | 4 | 5.7 |
| Fainting spells | 6 | 8.6 |
| Eye deviation and twitching | 1 | 1.4 |
| Abnormal neck movement | 3 | 4.3 |
| Abnormal body movement | 6 | 8.6 |
| Frequency of seizures | ||
| Daily | 25 | 35.7 |
| Persistent | 39 | 55.7 |
| Rare | 3 | 4.3 |
| Undefined | 3 | 4.3 |
| Duration of EEG | ||
| 24 h | 22 | 31.4 |
| 48 h | 37 | 52.9 |
| 72 h | 11 | 15.7 |
- Note: This table shows gender distribution, clinical presentation, seizure frequency, and EEG monitoring duration of patients.
All antiseizure medications were discontinued at the start of the study for those on the medications before the study. For some patients, we reduced the medication to 50% of the dose on day one and discontinued it the next morning. Following confirmation of diagnosis based on the clinical presentation and EEG result, appropriate antiseizure medication was restarted, mostly on the second day of the study. For patients whose paroxysmal events were determined to be non-epileptic, and on antiseizure drugs, the medication was permanently discontinued, and appropriate alternative therapy was recommended.
All patients underwent a combination of sleep deprivation, photic stimulation, and hyperventilation. A neurophysiologist and a nurse monitored the patients during the admission.
The diagnosis after the monitoring period was classified as an epileptic event, non-epileptic event, or no event. Non-epileptic events were further specified and classified.
The data were entered into Google Sheets and transferred to the Statistical Package for Social Sciences (SPSS) version 26. Descriptive statistics for sociodemographic characteristics and frequency of seizures were calculated. The occurrence of interictal events during each 8 h was noted and compared with the frequency of seizures reported during history taking. The frequency, percentage, and cumulative percentage of interictal events captured within each 8-, 24-, 48-, and 72-h sessions were cross-tabulated with the frequency of seizures. The chi-square test and confidence interval were used to determine the level of significance.
3 RESULTS
Seventy patients (34 males, 36 females) were included in our study. The mean age was 22.86 ± 18.00 years (Median:18.55 years, Range: 6 months to 80 years). The clinical presentations were various seizure-like activities with and without electrographic correlation. LTVEM was performed for 24 h in 22 patients (31.4%), 48 h in 37 patients (52.9%), and 72 h in 11 patients (15.7%). The average duration of monitoring was 44.23 ± 16.16 h.
3.1 Diagnostic yield of LTVEM
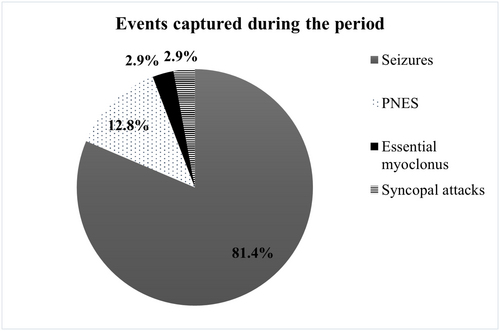
A total of 57 patients (81.4%) were confirmed to have seizures based on the clinical semiology and video electrographic findings. Of the 57 patients with ictal and interictal discharges, 31 had confirmed ictal discharges while 26 had interictal discharges. Thirteen patients (18.6%) experienced non-epileptic events. Patients who had non-epileptic events were further categorized as having psychogenic non-epileptic spells (12.8%), essential myoclonus (2.9%), and syncope (2.9%) (Figure 1).
3.2 Patients with seizures
From the admission history, of the 57 patients who were confirmed to have seizures based on electroclinical signs, 19 (33.3%) had daily events, 33 (57.9%) had persistent events, 3 (5.3%) had rare events, and 2 (3.5%) had undefined or unspecified events.
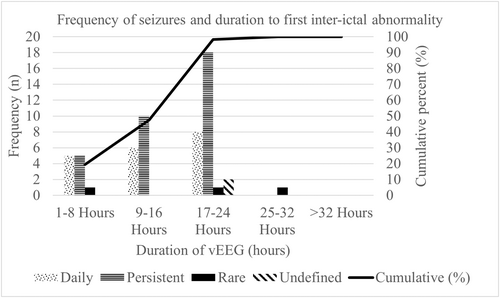
All electroclinical evidence of seizures was captured within 48 h of LTVEM. In addition, 56 of 57 patients with ictal and interictal discharge (98.2%) were captured within 24 h. This included 100% daily seizures, 100% persistent seizures, and 100% undefined events. One rare seizure was captured beyond the 24-h mark but within 48 h (Table 2). On further analyses, 19.3% had their first interictal epileptiform discharge within 8 h. There was an association between the frequency of seizures and the time to first interictal epileptiform discharge (p = 0.007, 95% CI: 1.60–1.94).
| 1–8 h | 9–16 h | 17–24 h | 25–32 h | Total | |
|---|---|---|---|---|---|
| Daily | 5 | 6 | 8 | 0 | 19 |
| Persistent | 5 | 10 | 18 | 0 | 33 |
| Rare | 1 | 0 | 1 | 1 | 3 |
| Undefined | 0 | 0 | 2 | 0 | 2 |
| Total | 11 | 16 | 29 | 1 | 57 |
| Percent (%) | 19.3 | 28.1 | 50.9 | 1.8 | 100 |
| Cumulative yield (%) | 19.3 | 47.4 | 98.2 | 100 |
- Note: This table shows the frequency of seizures and time to first interictal epileptiform discharge in hours.
The detection of ictal and interictal discharges increased with monitoring time, peaked at the 24 h, and declined (Figure 2). The majority (>50%) of the first ictal and interictal discharges were captured within 17–24 h.
3.3 Patients with non-epileptic events
Thirteen patients had non-epileptic spells. Of these 13 patients, nine were diagnosed with psychogenic non-epileptic spells (PNES). Two patients were diagnosed with essential myoclonus and two patients were diagnosed with syncope see Figure 3.
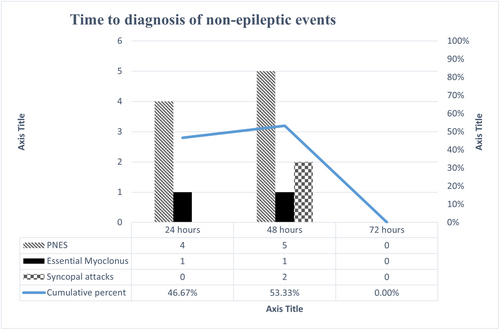
All non-epileptic spells were diagnosed before the 72-h mark, with an equal number diagnosed at 24 and 48 h. The nine patients with psychogenic non-epileptic spells were diagnosed within 48 h of the study, with four diagnosed within the first 24 h, revealing a diagnostic yield of 44.4% in the first 24 h and 100% in the first 48 h.
4 DISCUSSION
The utility and diagnostic efficacy of LTVEM has been firmly established within the field.1, 3 Nonetheless, the application of LTVEM in low-resource countries remains underexplored, with only a limited number of studies conducted. The utilization of LTVEM is impeded by notable financial constraints attributed to its substantial cost, the labor-intensive nature of its implementation, and its restricted availability.14 Therefore, there exists a compelling necessity to ascertain the diagnostic utility of LTVEM specifically within limited-resource countries. This imperative stems from the realization that the daily financial implications of LTVEM can be substantial, potentially dissuading prospective patients from seeking the benefits offered by this investigative procedure.
There exists a wide variability in the literature regarding the duration of LTVEM.12 A Taiwanese retrospective study revealed in 247 patients undergoing inpatient LTVEM, 21.2% had their clinical event at 3 h, the second wave at 33–36 h, and only 3.5% diagnosed after 57 h of monitoring.10 In contrast, a retrospective study in Qatar comprising 439 cases of LTVEM revealed that a monitoring duration of 72 h successfully recorded at least one seizure in 90% of patients diagnosed with epilepsy, as opposed to the 48 h duration required for patients with Psychogenic Non-epileptic Seizures (PNES).5 Additionally, a retrospective Australian study reported that 98% of events were captured by the 5th day.
Our study demonstrated that 57 of the 70 patients had electrographic evidence of seizures that were successfully captured within 48 h of LTVEM. Of the 57 patients with ictal and interictal discharges, 31 had confirmed ictal discharges while 26 had interictal discharges. The high burden of the interictal discharges, mainly during sleep, the location of these interictal discharges, and the clinical presentation provide valuable context for epilepsy diagnosis and guide appropriate management of the patient. Furthermore, 56 out of 57 (98.2%), with electrographic events were identified within the initial 24 h of monitoring. This encompassed various seizure types, including daily seizures, persistent seizures, and undefined events. However, it is worth noting that one rare seizure occurrence was recorded beyond the 24-h mark but still within the 48-h window (see Table 2). Further analyses revealed that in 19.3% of the study population, the first interictal epileptiform discharge was captured within 8 h of monitoring. This is similar to the result reported in the study by Lee CH et al. (2013) of 21.2% at 3 h10.
At least 20% of patients referred to comprehensive epilepsy programs do not have epilepsy.3, 15, 16 In prior research, the prevalence of patients experiencing paroxysmal events, who were diagnosed with PNES or events stemming from physiological conditions, ranged from 14% to 42%.17-19 Establishing an accurate diagnosis is vital as it can avert the prescription of unnecessary Antiepileptic Drugs (AEDs) and facilitate the implementation of suitable treatment strategies.3, 5, 9 In the current study, the application of LTVEM identified the target paroxysmal event as non-epileptic in 13 (18.6%) patients. Of these 13 patients, nine (12.8%) were diagnosed with PNES. Two (2.9%) patients were diagnosed with essential myoclonus and two (2.9%) patients were diagnosed with syncope. This is consistent with previous LTVEM studies that showed the prevalence of PNES among patients diagnosed with non-epileptic paroxysmal events.17-20
The diagnostic yield for interictal and ictal events in this study is 81.4%. This is similar to studies by Chen et al. and Hupalo et al21, 22 who reported 72.8% and 82.0%, respectively. However, some studies have demonstrated yields of <50%.23, 24
4.1 Conclusion
Our investigation demonstrates that a 24–72-h long-term video electrocardiogram is effective in diagnosing seizures in well-selected patients presenting with paroxysmal events, particularly in low-resource settings. We observed that most patients were diagnosed within 48 h of monitoring with an overall diagnostic yield of 81.4%. Furthermore, our study suggests that extending the monitoring period beyond 72 h does not yield substantial additional benefits. These results underscore the practicality and efficiency of the 24–72-h time frame for accurate diagnosis of epilepsy in resource-constrained environments.
4.2 Limitations
Not all patients for whom long-term video EEG was indicated ultimately underwent the procedure. Long-term video EEG was offered to those with appropriate indications. When finance was prohibitive to obtain the study, we prioritized the patients most likely to benefit from the study, focusing on the nuances of their clinical presentation and the semiology of their spells. For instance, in cases where patients were clinically suspected of having psychogenic non-epileptic seizures (PNES) on multiple antiseizure medications without control, and who cannot afford the study, we opted not to proceed with long-term video EEG. Instead, we offered alternative approaches, such as psychotherapy, discontinuation of antiseizure medications, and continued follow-up at the epilepsy clinic. Given the significant cost of the investigation and the economic challenges within the country, a substantial portion of the patients fell into this category. This careful selection process undoubtedly played a significant role in enhancing the diagnostic yield of the long-term video EEG.
The quantitative analysis of patient selection is out of scope of this manuscript.
It should also be noted that despite best efforts to obtain an accurate history from the patient, there is still the possibility that the patients and caregivers may have reported untrue information as regards the frequency of the seizure/paroxysmal event.
CONFLICT OF INTEREST STATEMENT
We confirm that the authors have no conflicts of interest or disclosures. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Open Research
DATA AVAILABILITY STATEMENT
Data not currently available publicly but will be made availabe on demand.