Abnormal Breast Temperature and Cortical Enlargement of the Axillary Lymph Nodes Through the Thermography
Funding: The authors received no specific funding for this work.
ABSTRACT
Breast thermography may be used for the early detection of breast diseases in women younger than 50 years. Performed breast thermography on a woman in her 20s, revealing an average temperature difference of about 1°C. Ultrasound imaging further identified a simple cyst and enlarged, vascularized lymph nodes in both axillae.
1 Introduction
In all over the world, it was reported that in the 2020, the number of deaths and new cases for breast cancer were 684,996 and 2,262,419, respectively. According to the age, the deaths were 131,322 of women younger than 50 years, and 553,674 of older than 50 years. For the year 2040, it is expected that the number of deaths increase to above 50%, while for the new cases 40% [1].
However, not all breast diseases are cancerous, which means that healthcare professionals must be vigilant in distinguishing breast lesions that may be mistaken for benign conditions [2-5]. Therefore, making an accurate differential diagnosis is crucial at various stages of a patient's consultation with a healthcare provider. Depending on the signs and symptoms, the physician may require imaging studies or even a biopsy of the suspicious tissue. The choice of imaging study depends on several factors, including the patient's age, the region of interest, and the type of information needed from the study [6, 7].
On the other hand, the primary goal of healthcare professionals is to improve and extend quality of life. Achieving this requires the early identification of signs and symptoms that may compromise a patient's health [8, 9]. In the context of breast cancer, particularly for women under 50, for whom mammography is typically not recommended, increasing the likelihood of early detection of breast abnormalities is critical [10-12]. To reach a broader segment of this population, there is a growing need for noninvasive qualitative and quantitative technologies [13-15].
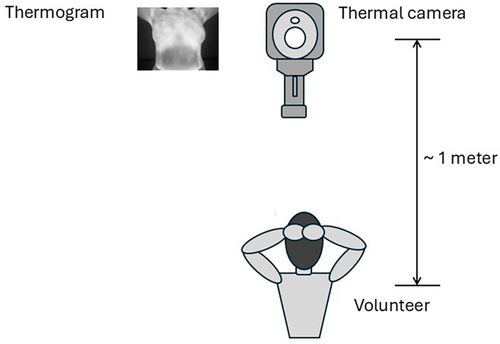
In the case reported here, the abnormality was detected using breast thermography [Appendix A]. This noninvasive technology aims to identify early signs of abnormal heat retention or dissipation in the studied tissue by quantitatively comparing physiologically equivalent regions of interest.
A woman in her 20s had a breast thermogram showing an average temperature difference of more than 1°C, with the right breast exhibiting the higher temperature. Due to her age, a second thermogram was performed 7 weeks later, yielding results similar to the initial one. An ultrasound of the left breast revealed a simple cyst with a diameter of 2.4 mm, predominantly located in the upper outer quadrant. Abnormal lymph nodes with diffuse cortical enlargement were observed in both axillae, measuring 8 mm on the right and 3 mm on the left. Additionally, rim blood vessels were noted in both lymph nodes. The patient was referred to her healthcare provider for further evaluation.
Since breast thermography provided crucial information regarding her breast health, regardless of age, it could be considered as a complementary tool in breast health protocols. Additionally, thermography appears to offer valuable insights into the status of the sentinel lymph node.
2 Case History
A woman in her 20s signed an informed consent to participate in a breast thermography campaign. She was fully informed about her participation, and all her questions were answered. The thermography was performed following the protocol of the American Academy of Thermology [16]. Figure 1 illustrates the process of acquiring the thermogram. The volunteer is positioned approximately 1 m in front of the thermal camera. The operator activates the camera, allowing the thermal sensors to capture the radiation emitted by the volunteer. Her thermogram revealed an average temperature difference of more than 1°C between the right and left breasts, which is considered abnormal [16].
3 Method
A second thermogram was acquired 7 weeks later, with results like the previous one. In both thermograms, the right breast was warmer than the left. Based on these findings, a breast ultrasound was ordered. The ultrasound revealed a simple cyst, 2.4 mm in diameter, located predominantly in the upper outer quadrant of the left breast. Abnormal lymph nodes were also observed in both axillae, with diffuse cortical enlargement measuring 8 mm on the right and 3 mm on the left. Additionally, rim blood vessels were detected in both lymph nodes.
4 Conclusions and Results
The thermography study is designed to compare heat conservation and dissipation between the right and left breasts by calculating the average temperature in specific regions of interest (ROIs). In this study, the average temperatures were measured across seven ROIs, covering all areas of the breast: the four quadrants, the axilla, and the nipple along with the areola.
The results are summarized in Table 1. The first column lists the names of the ROIs, while the second and third columns show the average temperature for each ROI. The average temperature difference (ATD) between the right and left ROIs is presented in the fourth column. The data indicate that the ATD across the entire breast was 0.8°C, which is not statistically significant. However, the ATD for the quadrants Q1, Q3, Q4, and the nipple and areola were 1.0°C or greater, which is considered abnormal [16].
| Skin tissue | AT right (°C) | AT left (°C) | AT difference ATD (°C) |
|---|---|---|---|
| Overall | 32.9 | 32.1 | 0.8 |
| Q1 upper-outer | 32.7 | 31.7 | 1.0 |
| Q2 upper-inner | 32.3 | 31.8 | 0.5 |
| Q3 lower-inner | 33.1 | 32.0 | 1.1 |
| Q4 lower-outer | 33.2 | 32.0 | 1.2 |
| Armpit | 34.4 | 34.0 | 0.4 |
| Nipple+aureole | 32.8 | 31.6 | 1.2 |
- Note: The table lists the seven regions of interest (ROIs) where the average temperature (AT) was calculated. The fourth column shows the average temperature difference (ATD) between the right and left breasts for each ROI.
The results, from the second thermogram, are displayed in Table 2. The fourth column shows ATD, between the right and left ROI. The ATD from all-over breast was still of about 0.8°C. At this time, the ATD from the quadrants Q1, Q2, and the N + A were equal-greater than 1.0°C, which is considered abnormal [16].
| Skin tissue | AT right (°C) | AT left (°C) | AT difference ATD (°C) |
|---|---|---|---|
| Overall | 35.3 | 34.5 | 0.8 |
| Q1 upper-outer | 35.3 | 34.3 | 1.0 |
| Q2 upper-inner | 34.8 | 33.5 | 1.3 |
| Q3 lower-inner | 35.7 | 34.8 | 0.9 |
| Q4 lower-outer | 35.7 | 35.1 | 0.5 |
| Armpit | 35.9 | 36.6 | −0.7 |
| Nipple+aureole | 35.6 | 34.4 | 1.2 |
- Note: The table lists the seven regions of interest (ROIs) where the average temperature (AT) was calculated. The fourth column shows the average temperature difference (ATD) between the right and left breasts for each ROI.
The volunteer underwent a breast ultrasound, which revealed a simple cyst measuring 2.4 mm in diameter, predominantly located in the upper outer quadrant of the left breast (Q1). Abnormal lymph nodes in both axillae were noted, with diffuse cortical enlargement measuring 8 mm on the right and 3 mm on the left. Additionally, rim blood vessels were observed in both lymph nodes. As of the time this report was submitted, the woman is under the care of a healthcare professional team and receiving all necessary attention.
The volunteer who participated in the breast thermography campaign reported that the information she received significantly improved her quality of life. She stated, ‘Thanks to the thermography, I now know that I have health issues with my breasts that I need to address with the medical team.’ The volunteer also noted that she was aware of the enlargement of both lymph nodes but had not paid much attention to it. It was the thermography that provided critical insights into her breast health and prompted her to take appropriate action.
More detailed data and analysis are needed to understand why the warmer breast does not correspond to the breast with the cyst. Additionally, studying the average axillary temperature over time may require a specific protocol. However, breast thermography could be incorporated as a complementary study within standard protocols.
5 Discussion
In terms of heat conservation and dissipation, which are autonomous physiological processes, thermography is useful for objectively comparing the average temperature across different ROIs that are physiologically equivalent. In breast thermography, an abnormal ATD should not be assumed to be exclusively indicative of cancer. It may also result from factors such as inflammation, infection, trauma, physical issues, or other conditions.
In the case presented, the location of the cyst does not align with the hotter region identified by thermography. According to the ultrasound, the cyst is predominantly in quadrant Q1 of the left breast, while the thermograms show hotter regions in quadrants Q1, Q2, Q3, and Q4 of the right breast. Additionally, although both lymph nodes in the axillae were identified as abnormal on the ultrasound, the ATD in the axillae from the thermograms was considered normal [16]. From Table 2, it is observed that both breasts showed an increase in temperature compared to the first thermogram (Table 1). By analyzing the gradient between different ROIs on both thermograms and comparing physiologically equivalent ROIs, it is noted that the left breast, particularly the left axilla, was hotter than the right breast.
It is widely accepted that the axillary lymph node can serve as the sentinel lymph node for breast cancer. Once detected, this lymph node is biopsied to identify the type of cancer [17-20]. However, there appear to be no established techniques or protocols for its early detection. Therefore, thermography could potentially provide information on its presence. To achieve this, a specific protocol for a series of thermograms needs to be developed to monitor this lymph node.
Many young women are often unaware of their breast health, and certain signs or symptoms may go unnoticed by both themselves, and healthcare professionals. Thus, breast thermography could serve as an alternative for obtaining objective information about breast health. Additionally, thermography could be incorporated into existing protocols. For example, a Papanikolaou test for cervical cancer could be complemented with breast thermography. This is not due to any direct correlation between cervical cancer and breast diseases, but rather to provide a more comprehensive approach to women's health. Furthermore, breast thermography may provide information to help differentiate between benign conditions and breast cancer [2].
Author Contributions
Francisco-J Renero-C: conceptualization, data curation, formal analysis, investigation, methodology, project administration, writing – original draft, writing – review and editing. Tania-Cristell Martínez-Azmitia: conceptualization, supervision, validation.
Ethics Statement
Ethical approval was not required, because of, that this case report was captured by a breast thermography campaign. Furthermore, the thermography is totally not-invasive; the acquisition protocols guarantee the confidentiality of the participant volunteers.
Consent
The volunteer signed the printed consent statement in accordance with the journal's patient consent policy.
Conflicts of Interest
The authors declare no conflicts of interests.
Appendix A
Thermography is a technique used to record thermal radiation from the study area. This technology does not emit any signals; instead, it relies on a grid of thermal radiation sensors. The device's electronics convert the thermal radiation detected by each sensor into temperature values, which are then stored in a digital file. These temperature values are presented as a thermal map in false colors, known as a thermogram.
Open Research
Data Availability Statement
The data are available upon request to the authors.