Metastatic hepatocellular carcinoma presenting as a lytic calvarial mass
Key Clinical Message
Hepatocellular carcinoma (HCC) is one of the most common types of cancer. More focus is being placed on clinical presentations of distant metastasis from HCC. Head masses should be investigated even when no concerning symptoms are found in patients with prior history of alcohol abuse and liver comorbidities.
1 INTRODUCTION
Hepatocellular carcinoma (HCC) is one of the most common types of cancer with a predominately higher prevalence in East Asia and Africa.1 This incidence rate is attributed to an increased prevalence of co-morbid chronic hepatitis B in patients within these geographic regions.2-4 HCC metastases are reported to occur at a rate less than 5% with spread occurring within regional lymph nodes and the lungs.3, 4 This typically occurs for patients undergoing late-stage metastasis. The current literature indicates that HCC has preferential metastasis to the vertebral column, pelvis, and ribs. In addition, HCC metastatic manifestations in the skull or skeleton are classified medically as rare.2 Previously, clinical providers focused primarily on management of the primary cancer due to a lack of treatment options. However, recent progress in the treatment of HCC has allowed long-term survival rates to increase significantly. We present the case of a 74-year-old male patient with an unusual presentation of metastatic hepatocellular carcinoma. The data presented may help enhance clinical knowledge of HCC manifestations, which may help guide early detection of skull metastasis and improve the patient's prognosis and quality of life.
2 CASE HISTORY/EXAMINATION
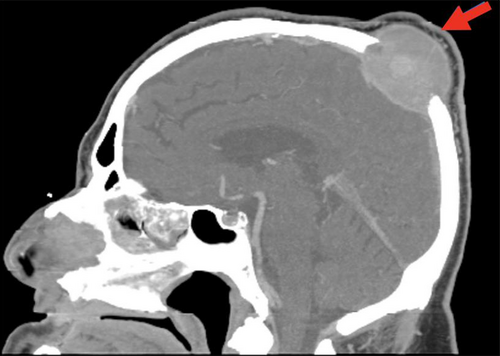
A 74-year-old male with a medical history significant for treated chronic hepatitis C infection, alcohol abuse, and cirrhosis presented to the emergency department with an enlarging area of swelling on the top of his scalp over 1 month. He denied pain at the time of evaluation but reported intermittent episodes of headache in the swollen area associated with blurry vision, especially in the morning. No imaging was obtained, and a lipoma was suspected. He was discharged to follow up with plastic surgery. Six weeks later, an outpatient head and neck CT was obtained, which showed a lytic destructive lesion centered in the left parietal bone with an associated 4 × 4.7 × 4 cm soft tissue density mass (Figure 1). He was referred to neurosurgery for scheduling of a brain MRI, however, this was not obtained due to bullet fragments in his chest.
3 METHODS (DIFFERENTIAL DIAGNOSIS, INVESTIGATIONS, AND TREATMENT)
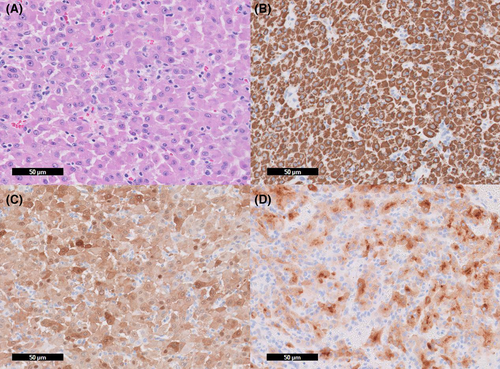
Five days after the second head CT, the patient presented to the Emergency Department due to the mass rapidly increasing in size, gait imbalance with leftward inclination while walking, intermittent confusion, and blurred vision of the left eye. Another CT of the head was repeated which showed a lytic calvarial mass at the vertex with both intracranial and extracranial extension, having a mass effect on the superior sagittal sinus without definite occlusion/thrombosis or intravascular invasion. CT chest, abdomen, and pelvis were done to rule out metastatic malignancy and it showed a mildly cirrhotic liver and a 4.1 cm mass in segment 6 which is hypovascular on portal venous phase. There was no evidence of extrahepatic malignancy in the abdomen and pelvis. Neurosurgery was consulted and performed a biopsy, which was sent for pathological diagnosis (Figure 2). In suspicion of hepatocellular primary, alpha-fetoprotein level was checked but it returned normal.
4 CONCLUSION AND RESULTS (OUTCOME AND FOLLOW-UP)
The patient was discharged with a scheduled follow-up with neurosurgery. Surgical pathology showed morphologic and immunohistochemical findings consistent with well-differentiated metastatic hepatocellular carcinoma (Figure 2). The decision to perform Y90 radioembolization for the hepatic primary neoplasm and stereotactic body radiotherapy (SBRT) for the skull mass was made following discussion of the case at a multi-disciplinary oncology conference. An immunotherapy regime of atezolizumab plus bevacizumab would later follow. The calvarial lesion was treated with 800 cGy × 5 frac-tions for 4000 cGy of CyberKnife SBRT. The liver lesion was treated with Y90 radio-embolization through the right hepatic artery. Both radiation treatments were completed 6 weeks post-diagnosis.
One-month post radiation, the patient came for a follow-up visit. He presented with complaints of headache. He was also found to be hypotensive and tachycardic, and the scalp mass appeared larger and more cystic than prior. He was admitted to determine if there was an underlying abscess or radiation necrosis. Abdominal CT showed no change in the hepatic lesion (Figure 3) and head CT showed an interval increase in the size of the metastatic lesion with extension along the superior sagittal sinus with progressive mass effect on the underlying brain parenchyma but without evidence of associated cerebral edema. Radiation oncology reviewed the CT scan and determined that the size of the mass was stable from the prior and the exam finding of change in consistency from firm and fixed to soft and cystic was likely indicating a good response to radiation therapy. However, with complaints of headache and radiologic evidence of some mass effect on underlying brain parenchyma, the decision was made to start steroids.

Six weeks post-radiation and 12 weeks post-diagnosis, immune therapy with bevacizumab and atezolizumab was planned to be started, but the patient was found to have low baseline cortisol and TSH levels. Therefore, lenvatinib 12 mg was started in-stead. Ultimately, the low cortisol/ACTH was attributed to prolonged steroid use, but the treatment plan did not change with this discovery. Imaging at this time showed no significant change in the size of the calvarial mass and a slightly contracted in size of the hepatic lesion. Labs showed his AFP levels were trending down, conferring compatibility with treated HCC.
Seventeen weeks after starting Lenvatinib, the patient reported episodes of pre-syncope, dizziness, weight loss and failure to thrive. Therapy was discontinued and a significant improvement in symptoms was seen 3 weeks later. Two months after discontinuation, Lenvatinib was restarted, and the dose was reduced to 8 mg. Six and a half months after restarting Lenvatinib, the dose was decreased to 4 mg daily due to weight and appetite loss. Continued interval scans showed stable to improved disease in the liver and the metastatic calvarial lesion. He had progressive liver failure and cirrhosis with ascites requiring intermittent paracentesis.
5 DISCUSSION
Despite HCC being the fifth most common type of cancer, no adequate screening tools have been identified to date.5 Initial staging work-up should entail viral serologies, liver function studies, and chest CT. Alpha-fetoprotein (AFP) has poor sensitivity and specificity for detecting HCC, which may lead to delay in diagnosis. For example, values above 400 ng/dL are deemed diagnostic for HCC, but this significant elevation only occurs in a minor proportion of patients. HCC is often uncovered later in the clinical picture, possibly attributed to the malignancy having to increase to a significant degree before invasion of nearby organs, only then producing prominent symptoms. In addition, the liver has significant reserves; clinical presentations such as jaundice do not manifest until the tumor has replaced a significant amount of liver parenchyma.5 Advanced HCC typically presents as weight loss, fatigue, right upper quadrant pain, and anorexia.
Incidence of skull metastasis in HCC patients is low. Therefore, due to the rarity of this presentation, radiation therapy is not commonly practiced. In many cases, the detection stage may be too late for radiation therapy.5, 6 In addition, as HCC is known to be resistant to chemotherapy and radiotherapy, the primary treatments for HCC consist of surgical resection, liver transplantation, tyrosine kinase inhibitors (e.g. sorafenib), thermal ablation, or immunotherapy. A phase III trial demonstrated patients with unresectable HCC had increased 1 year survival in those treated with atezolizumab-bevacizumab versus those treated with sorafenib (67.2% vs. 54.6%, respectively). As such, immunotherapy has revolutionized HCC care.
Reported patient outcomes for those affected by skull metastasis are poor.7 Metastasis to cranial areas is often a sign of advanced disease. The patient presented in this report had an incidental discovery of a scalp mass after presenting with associated symptoms. Historically, clinical presentations of skull masses in HCC patients include symptoms of neurological deficits (44%), followed by headache (11%) and seizure (11%).2 Therefore, clinicians should have a high level of suspicion for metastasis in patients presenting with neurological deficits including facial palsy, deafness, visual disturbances, and facial numbness among other manifestations.2 As such, including a neurological workup may be helpful in the initial evaluation of patients with a confirmed diagnosis of HCC.
Skull metastasis from HCC is often discovered incidentally. Patients will usually present with symptoms including increased intracranial pressure, headaches, vision changes, dysphagia, diplopia, trigeminal neuralgia, and occipital neuralgia. Calvarial lesions due to metastasis can occur in any region of the skull. Dural sinus involvement has been correlated with significant changes in intracranial pressure and often indicates disseminated disease progression. Management of calvarial lesions involves an individualized approach depending on the location and presenting symptoms. Historically, surgical resection has been considered in cases where a single lesion is present and is causing neurological deficits. As patients with disseminated metastasis are not considered suitable candidates for resection, radiotherapy with Gamma Knife surgery is an emerging option for patients. Calvarial lesions due to HCC metastasis are a late and rare presentation in patients with HCC. As such, prognosis is usually poor. It is essential for providers to closely monitor patient development and consider a diverse symptom presentation for patients with HCC.
AUTHOR CONTRIBUTIONS
Shirley Parraga: Conceptualization; data curation; investigation; methodology; project administration; resources; visualization; writing – original draft. Melisa Pasli: Conceptualization; data curation; investigation; methodology; project administration; supervision; writing – original draft. Hayley Behm: Conceptualization; methodology; visualization; writing – review and editing. Breann Zeches: Conceptualization; writing – review and editing. Revanth Reddy: Conceptualization; methodology; project administration; writing – original draft.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts to disclose.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.




