Approaching a patient with poststernal pain after eating: A case report
Yanjun Feng and Yayan Niu have contributed equally.
Key Clinical Message
This article reports a case of mediastinal lymph node tuberculosis with no obvious symptoms and a concealed focus. This patient, a 33-year-old male, suffered from pain behind the sternum after eating. He underwent three gastroscopic examinations and two fine needle punctures guided by ultrasound gastroscopy but was not diagnosed. Chest-enhanced CT revealed a mediastinal mass compressing the adjacent esophagus, suggesting the possibility of enlarged lymph nodes. Furthermore, T cells from patients infected with tuberculosis tested positive. Ultrasound bronchoscopy revealed enlarged lymph nodes in area 7, and then EBUS-TBNA was performed in that region. Only a few scattered lymphocytes and necrotic tissue were found under the biopsy microscope. The EBUS-TBNA biopsy Xpert MTB/RIF showed low positive results, and the EBUS-TBNA puncture fluid Xpert MTB/RIF was positive. Therefore, he was diagnosed with mediastinal lymph node tuberculosis. After antituberculosis treatment with the 2HREZ/10HRE regimen, the patient's pain behind the sternum gradually alleviated, and the enlarged mediastinal lymph nodes gradually narrowed.
1 INTRODUCTION
Tuberculosis of the mediastinal lymph nodes is a chronic disease caused by Mycobacterium tuberculosis (MTB) invading multiple groups of lymph nodes in the mediastinum. Previous reports have focused primarily on children, but current data show that the incidence of adult primary mediastinal lymph node tuberculosis is still 25.0%–35.7%.1, 2 The onset of mediastinal lymph node tuberculosis is insidious, and it is often misdiagnosed as another disease in the early stage due to the absence of clinical symptoms specific to tuberculosis. Moreover, there were no specific characteristics on imaging examination. Therefore, it is easy to misdiagnose, leading to treatment delays. This patient underwent three gastroscopic examinations and two ultrasonic gastroscopic punctures due to poststernal pain after eating, but the diagnosis remained unclear. Chest-enhanced CT revealed the possibility of enlarged lymph nodes in the mediastinum. Finally, EBUS-TBNA was used to obtain samples for tuberculosis-related molecular biological detection.
2 CASE HISTORY
A 33-year-old male patient was admitted to the hospital on September 5, 2020, due to “intermittent poststernal pain persisting for more than one month.” More than a month ago, the patient developed poststernal pain after eating and acid-belching after eating, accompanied by dysphagia and poor feeding; however, the patient did not experience nausea, hiccups, vomiting, fever, or chest tightness. The patient went to the gastroenterology department of Suzhou Kowloon Hospital. Gastroscopic examination revealed chronic superficial gastritis and esophageal protrusion. Without a clear diagnosis, the patient was referred to the First Affiliated Hospital of Soochow University. On August 11, 2020, he underwent fine needle puncture guided by ultrasound gastroscopy. Biopsy pathology indicated chronic inflammation with squamous epithelial hyperplasia and mild atypical hyperplasia of the focal epithelium. The patient was referred to the Second Affiliated Hospital of Soochow University. On August 27, 2020, the patient underwent neck + chest enhanced CT. The results were as follows: ① the middle mediastinum occupied space, compressed the adjacent esophagus, and possibly enlarged lymph nodes; ② scattered small solid nodules with partial calcification in both lungs; ③ a few old foci in the upper lobes of both lungs; and ④ no obvious abnormalities in the neck. The patient underwent gastroscopy and ultrasound-guided fine needle puncture again. Pathology revealed scattered lymphocytes and stretched, deformed cell clusters. The pathological results are still not clear. Due to the positive results of the gamma interferon release test, the patient was suspected to have tuberculosis and was referred to our hospital. During the course of the disease, the patient felt tired and unwell and lost approximately 4 kg of weight in a month. The patient did not experience coughing, expectoration, night sweats, fever, or any other discomfort. He had a poor appetite, slept well at night, and had no issues with urination or defecation. His father was once a tuberculosis patient, and the patient had been in close contact with him for 2 months when the father was ill. There were no apparent abnormalities in the subject's allergy history, personal history, or family history.
3 INVESTIGATIONS AND TREATMENT
3.1 Clinical examination
Physical examination on admission revealed the following: body temperature, 36.5°C; pulse, 88 breaths/min; respiration, 18 breaths/min; blood pressure, 111/74 mmHg; clear mind; good spirit; coarse breath sounds in both lungs; no obvious dry or wet rales; arrhythmia; abdominal flatness; no tenderness; rebound pain; no mobile dullness; and no edema in either lower limb.
3.2 Supplementary examination
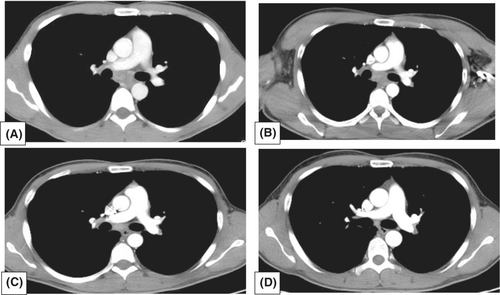
Neck and chest enhanced CT (Second Affiliated Hospital of Suzhou University, August 27, 2020) revealed no obvious abnormalities in the neck. A few solid micronodules were scattered in both lungs, some of which showed calcification. Additionally, a few strip shadows were found in the upper lobes of both lungs, and a mass of lamellar soft tissue density shadow was detected in the middle mediastinum. The soft tissue was irregular, and the boundary between the local and surrounding tissues was unclear. The size of the soft tissue was approximately 33 × 21 × 32 mm. An enhanced scan revealed uneven moderate enhancement (Figure 1). Ultrasound gastroscopic puncture pathology (Second Affiliated Hospital of Suzhou University, September 1, 2020) revealed scattered lymphocytes and stretch deformed cell clusters. Ultrasound gastroscopic puncture pathology conducted at the Second Affiliated Hospital of Suzhou University on September 1, 2020, revealed the presence of scattered lymphocytes and elongated, deformed cell clusters. A T-cell test for tuberculosis (TB) infection (Second Affiliated Hospital of Suzhou University, September 1, 2020) was positive.

3.3 Further examination after admission
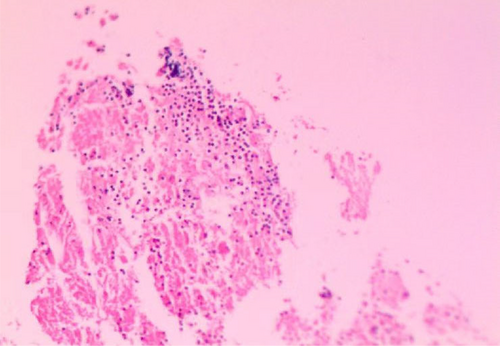
White blood cell count, 5.96 × 109/L; red blood cell count, 4.49 × 1012/L; hemoglobin, 142 g/L; platelet count, 195 × 109/L; neutrophil count, 3.21 × 109/L; and high-sensitivity C-reactive protein concentration, <0.5 mg/L. The biochemical parameters were as follows: total bilirubin: 6.4 μmol/L, direct bilirubin: 2.5 μmol/L, albumin: 41.1 g/L, glutamic oxaloacetic transaminase: 22 U/L, glutamic pyruvic transaminase: 12 U/L, glucose: 4.55 mmol/L, total cholesterol: 3.99 mmol/L, triglyceride: 0.43 mmol/L, creatinine: 68.9 μmol/L, uric acid: 605.0 μmol/L, and potassium: 4.51 mmol/L. sodium: 142.1 mmol/L; erythrocyte sedimentation rate: 2 mm/h. Hepatitis C antibody, hepatitis B surface antigen, syphilis antibody and human immunodeficiency virus antibody were all negative. The Cryptococcu antigen test was negative. Coagulation function tests were normal. Neither alpha-fetoprotein nor carcinoembryonic antigen showed abnormalities. Ultrasound bronchoscopy revealed enlarged lymph nodes in area 7, and then EBUS-TBNA was performed in that region (Figure 2). The EBUS-TBNA biopsy utilized Xpert Mycobacterium Tuberculosis/Rifampicin (Xpert MTB/RIF) real-time fluorescence quantitative nucleic acid amplification detection technology. The results showed low positive detection of MTB nucleic acid and undetectable for rifampicin resistance. Subsequent testing with Xpert MTB/RIF on the EBUS-TBNA puncture solution confirmed positive MTB nucleic acid and undetectable for rifampicin resistance. Pathology revealed that only a few scattered lymphocytes and necrotic tissues were observed under the microscope in Region 7 lymph nodes (Figure 3).

3.4 Diagnosis and treatment
The patient had a history of close contact with pulmonary tuberculosis patients. Tuberculosis-infected T cells tested positive. Ultrasound bronchoscopy revealed lymph node enlargement in area 7. The EBUS-TBA biopsy Xpert MTB/RIF test indicated a weakly positive MTB nucleic acid result that was undetectable or below the lowest detection limit for rifampicin resistance. Testing with Xpert MTB/RIF on the EBUS-TBNA puncture solution confirmed positive MTB nucleic acid and undetectable or below the lowest detection limit for rifampicin resistance. Therefore, the diagnosis was mediastinal lymph node tuberculosis.
Starting on September 10, 2020, antituberculosis treatment with 2HREZ/10HRE was administered. Rifampicin: 0.45 g, isoniazid: 0.3 g, ethambutol: 0.75 g, once a day; pyrazinamide: 0.5 g, three times a day.
4 OUTCOME AND FOLLOW-UP
After antituberculosis treatment, the patient's pain behind the sternum gradually alleviated, and the number of enlarged lymph nodes in the mediastinum gradually decreased and the patient returned to normal (Figure 4).
5 DISCUSSION
The mediastinum, anatomically, refers to the area below the thoracic inlet, above the diaphragm, and between the left and right lungs. Tuberculosis of the mediastinal lymph nodes can affect all groups of mediastinal lymph nodes, but it predominantly affects those around the trachea, particularly on the right side and under the carina. The incidence of mediastinal lymph node tuberculosis is similar to that of other forms of extrapulmonary tuberculosis. MTB can enter the human body through the respiratory system, digestive system, or skin mucosa and survive for an extended period by developing strong resistance to the human immune system. Then, they remain dormant for a long period of time (inactive or latent MTB) and reactivate when the immune system weakens or when other favorable environments exist. Activated MTB causes extensive damage by entering the blood and attacking other organs, including the lymphatic system. Blood infiltration often manifests as miliary tuberculosis and tuberculous meningoencephalitis, and lymph infiltration manifests as hilar and mediastinal lymph node enlargement.1, 2 The hilum of the lungs is the location where the main bronchus, pulmonary artery, pulmonary vein, bronchial artery, vein, lymphatic vessel, and nerve enter and exit. It is an elliptical depression in the center of the medial surface of the lungs. If only the hilar lymph nodes in the mediastinum are enlarged, it is classified as primary tuberculosis. Primary tuberculosis is typically diagnosed in children, especially those under 5 years old, but it is rare in adults. Due to its rarity, the diagnosis of adult primary tuberculosis is often overlooked.3 The typical manifestation of uncomplicated primary tuberculosis is enlarged lymph nodes located only in the mediastinum of the lung hilum.4
The clinical manifestations of mediastinal lymph node tuberculosis are primarily associated with compression symptoms of the affected lymph nodes and related complications. Additionally, there may be symptoms of tuberculosis poisoning, such as low-grade fever in the afternoon, night sweats, and weight loss. When enlarged lymph nodes compress the respiratory tract, they can cause partial or complete airway obstruction, leading to air retention or atelectasis, which can result in complex primary tuberculosis infections. When lymph nodes produce pus and rupture, the pus can penetrate the respiratory tract, facilitating the transmission of tuberculosis through the respiratory tract via a humoral mechanism, leading to more severe complications.5 Enlarged lymph nodes located next to the trachea and the main bronchus can compress these airways, leading to breathing difficulties, particularly in children. This compression manifests as difficulty breathing in, known as inspiratory dyspnea, and bluish discoloration of the skin, known as cyanosis. Long-term pressure on the trachea and bronchus results in local mucosal congestion and edema, ischemia, softening, necrosis of the tracheal wall, or a lymph node abscess directly penetrating the tracheal wall to cause tracheal and bronchial lymphatic impotence. The enlargement of paraesophageal lymph nodes may cause dysphagia by compressing the esophagus. Esophageal swallowing examination reveals external pressure stenosis, and prolonged compression could result in esophageal perforation. Compression of the recurrent laryngeal nerve by swollen lymph nodes can lead to ipsilateral vocal cord paralysis and hoarseness. Obstinate hiccups can result from compression of the phrenic nerve; Homer syndrome occurs when the sympathetic nerve is compressed; compression syndrome of the superior vena cava may occur due to compression of large vessels; aortic compression can lead to the formation of a pseudoaneurysm; and in severe cases, aortic perforation may occur. Sometimes, mediastinal lymph node tuberculosis can spread upward to cause cervical lymph node tuberculosis. Abscesses can lead to empyema by penetrating the mediastinal pleura, while chronic sinus can form by penetrating the sternum or the skin under the xiphoid process, which may not heal for an extended period.5 When lymph nodes produce pus and rupture, the pus infiltrates the respiratory tract, promoting the transmission of tuberculosis through the respiratory tract via a humoral mechanism, leading to more severe complications.6 This patient had an insidious onset and no symptoms of tuberculosis infection but only experienced pain after intermittent meals. After being transferred to three major general hospitals for the evaluation of digestive tract diseases, an enhanced chest CT examination revealed a soft tissue density mass in the middle mediastinum. After being transferred to our hospital, ultrasound bronchoscopy revealed swollen lymph nodes in area 7. Therefore, the symptoms of the digestive tract should be related to compression of the esophagus by the enlarged mediastinal lymph nodes.
Since mediastinal lymph node tuberculosis can be symptomatic or asymptomatic, chest CT abnormalities may be the most prominent indicator of this condition. Due to its hidden location, diagnosing and evaluating enlarged lymph nodes in the mediastinum is typically very challenging.7 Mediastinoscopy is a challenging and invasive procedure with numerous complications, hence its infrequent utilization.8, 9 Transbronchial needle aspiration biopsy can sample pathological changes in the trachea, parabronchus, and lung hilum. The scope of the examination is broad, offering a method for diagnosing tuberculosis in mediastinal and hilar lymph nodes. However, because it is considered a “blind” technology, the technical requirements and risk allocation are relatively high, which is not conducive to development. Endoscopic ultrasound-guided transbronchial needle aspiration is a new technology that combines ultrasound, bronchoscopy, and needle aspiration biopsy. It can be used to explore the enlarged lymph nodes and space-occupying lesions around the mediastinum, hilum of the lung, tracheobronchial area, and ultrasound-guided puncture. Its operational technology offers the advantages of accurate positioning, minimally invasive procedures, high sensitivity, specificity, and repeatability, and it is increasingly being utilized in developing countries.10, 11 Since the initial symptoms at this clinic were related to the digestive tract, we performed two ultrasonic gastroscopic punctures at the general hospital, but a definitive diagnosis could not be made. According to the location of the patient's lesion, we performed endoscopic ultrasound-guided transbronchial needle aspiration to obtain samples for diagnosing tuberculosis.
As an infectious disease, tuberculosis is diagnosed based on etiology and pathology findings.12 Etiological examination includes finding acid-fast bacilli by smears, cultivating mycobacteria, and detecting the molecular biology of tuberculosis. The positivity rate of traditional acid-fast bacilli smears is low, and nontuberculous mycobacteria can interfere with the results. In addition, culturing mycobacteria takes a long time, and the process is complex. In contrast, Xpert MTB/RIF can rapidly detect MTB and rifampicin resistance. It was recommended by the World Health Organization (WHO) as one of the diagnostic criteria for adult tuberculosis in 2010. In 2013, the WHO also recommended it for the diagnosis of children's tuberculosis and extrapulmonary tuberculosis (EPTB).13, 14 Kohli et al.15 used MTB culture as the “gold standard” in a meta-analysis of Xpert MTB/RIF detection for EPTB diagnosis. The sensitivity and specificity of the Xpert MTB/RIF summary of the lymph node aspirates were 81.6% (61.9%–93.3%) and 96.4% (91.3%–98.6%), respectively. The diagnosis of mediastinal lymph node tuberculosis and the sensitivity to ifampicin were confirmed by the weak positive Xpert MTB/RIF test of biopsy specimens from mediastinal lymph nodes and the positive Xpert MTB/RIF test of puncture fluid in this case. After the diagnosis, we provided patients with a standardized antituberculosis treatment program.
Due to the low incidence of mediastinal lymph node tuberculosis, tuberculosis is often overlooked by doctors. Additionally, the location of the mediastinal lymph nodes is hidden, making diagnosis in this region particularly challenging. Fortunately, the patient's clinical symptoms were mild, without airway compression, lymphatic fistula, or other complications. Although the road to diagnosis and treatment is challenging and involves multiple hospitals, specimens can be accurately obtained through EBUS-TBNA. The diagnosis of Xpert MTB/RIF was clear, and there was no rifampicin resistance. After standardized treatment, the treatment response was positive, clinical symptoms disappeared, and imaging revealed a significant reduction in the focus.
6 CONCLUSION
This case highlights that EBUS-TBNA combined with Xpert MTB/RIF is crucial for the precise and prompt diagnosis of mediastinal lymph node tuberculosis.
AUTHOR CONTRIBUTIONS
Yanjun Feng: Conceptualization; methodology; writing – original draft; writing – review and editing. Yayan Niu: Writing – original draft; writing – review and editing. Jinyu Yan: Methodology; resources; writing – original draft. Meiying Wu: Funding acquisition; methodology; resources; writing – review and editing. Peijun Tang: Methodology; resources; writing – original draft; writing – review and editing.
ACKNOWLEDGMENTS
Not applicable.
FUNDING INFORMATION
This research received a grant from the Respiratory Infectious Diseases Clinical Medical Center of Suzhou, China (Szlcyxzx202108).
CONFLICT OF INTEREST STATEMENT
The author reports no conflicts of interest in this work.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
All the findings are presented within the manuscript.