X-linked ichthyosis presenting with cryptorchidism for orchidopexy: A rare anesthetic encounter and case report
Abstract
Key Clinical Message
Cutaneous scaling and associated clinical syndrome displayed in X-linked ichthyosis mandates multidisciplinary care. Patient with ichthyosis confronts a numerous challenge to an anesthesiologist and demands a rigorous management. As these patients are very vulnerable perioperatively, meticulous care and support are utmost.
Ichthyosis is a group of genetic conditions distinguished by the appearance of hyperkeratotic scales on the skin's surface. X-linked ichthyosis results from a mutation in the steroid sulfatase (STS) gene, which encodes the steroid sulfatase enzyme. Here we report a case of a 6-year-old child with X-linked ichthyosis. He presented to our operation theater for correction of left-sided undescended testis and underwent surgery uneventfully. To handle X-linked ichthyosis perioperatively, meticulous planning and efficient anesthetic administration are critical.
1 INTRODUCTION
The appellation ichthyosis stems from the Greek word ‘ichthys’ meaning “fish” and alludes to the skin's resemblance to fish scales. Ichthyosis is an assortment of hereditary ailments marked primarily by the emergence of hyperkeratotic scales on the skin surface. Aberrant keratinization and shedding of the horny cell layer are observed in this clinical condition.1, 2
- Ichthyosis vulgaris.
- Lamellar ichthyosis.
- Epidermolytic hyperkeratosis.
- Harlequin Ichthyosis.
- X-linked ichthyosis.2
X-linked ichthyosis is known as steroid sulfatase (STS) deficiency. The disorder arises due to a mutation in the STS gene, which embodies the steroid sulfatase enzyme. Steroid sulfatase deficiency invites cholesterol sulfate buildup and cholesterol depletion, culminating in an erratic skin barrier and corneocyte retention. This condition can manifest at birth or after few weeks following birth. The consequence of STS deficiency emanates as progressive improper shedding of skin which out-turns as dry skin with visible polygonal scales. Corneal opacities, cryptorchidism, and behavioral problems are frequently reported with this circumstance.1
We hereby report a case of a 6-year-old child with X-linked ichthyosis. He presented to our hospital for surgical correction of left-sided undescended testis. Anesthetists do not regularly bump into such clinical scenarios. Management of these patients poses numerous challenges to them which makes this case an invaluable matter to talk about.
2 CASE HISTORY AND PRESENTATION
A 6-year-old child presented to our anesthesia clinic for preanesthetic evaluation. He was posted to undergo elective orchidopexy for left-sided undescended testis. There was a history of consanguineous marriage, prolonged labor and he was delivered vaginally. There was no history of any collodion membrane covering the skin at birth. But he developed abnormal peeling of the skin that started 1 week after delivery. Based on the history of consanguinity and protracted labor, he was diagnosed as case of X-linked ichthyosis. Initially peeling of skin started from bilateral cheeks and over the period years, the abnormal scaling advanced to involve torso, neck, flexor, and extensor surface of extremities and scalp. Palms, soles, and nails were spared. Additionally, child mother reported that the condition gets aggravated during the dry season and the child sometimes complains of pruritus. A family history of similar dermatological disorder was present in relatives from the maternal side of the child.
2.1 Examination
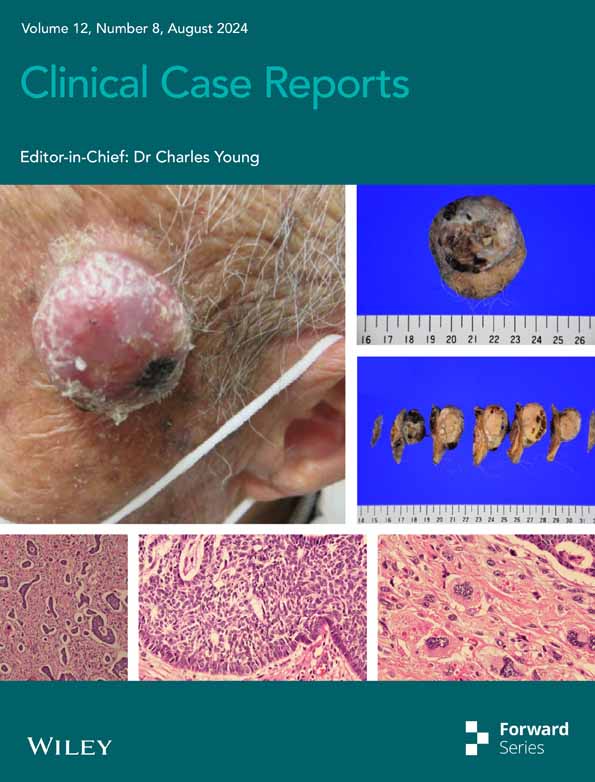
The child was oriented according to time, place, and person and vital signs were stable. On examination, the child had fish-like brownish scales over upper and lower limbs, trunk, and face. The scalp was also involved, and some scarring hair loss was observed (Figure 1). Teeth and eyes were normal. Examination of genitals revealed an empty left scrotal pouch and the presence of macerated scales over the bilateral scrotal skin. An unpleasant smell coming from the child's body was also noted.

2.2 Anesthetic evaluation and planning
The child weighed 15.5 kilograms. Developmental milestones were appropriate for age. Cardiac, respiratory, and nervous system examination was unremarkable. Mouth opening was more than 2 fingers. Routine blood investigations were normal (hemoglobin: 12.3 g/dL (11–15 g/dL), total leukocyte count: 6600/mm3 (4000/mm3–11,000/mm3), platelets: 225,000/mm3 (150,000/mm3–450,000/mm3), serum sodium: 141 mEq/L (135–145 mEq/L), potassium: 4.1 mEq/L (4.0–5.0 mEq/L)).
The dorsal surface of the right hand showed comparatively less desquamation than dorsum of left hand and was chosen for intravenous cannulation. Cotton gauze bandage was kept ready to secure cannula.
Macerated skin and flaking were also evident in sacral area. So, we did not opt caudal neuraxial technique to provide analgesia and looked for a combination of opioids, paracetamol, and NSAIDs.
Regarding airway management, we decided on supraglottic airway placement and planned to secure it with the help of a cotton gauze bandage.
We planned not to tape the eyes and instead use lubricant eye drops during the procedure due to the presence of scaling.
Temperature regulation of the operating room was kept in mind to prevent overheating and hypothermia.
ECG electrodes were kept and decided to be inserted in the site with minimal scaling.
2.3 Anesthetic management
The child was premedicated with 5 mg of oral midazolam by combining with honey and the effect was adequate after 20 min. Then, the child was taken inside theater. Cannulation was done with 24G cannula and secured with bandage. Induction was done with fentanyl (35 mcg), propofol (45 mg), and supraglottic airway device(igel) was placed. Anesthesia was maintained with sevoflurane, oxygen, and air mixture. Orchidopexy took 40 min to complete. During the procedure, body parts were covered with sheets to minimize heat loss. After completion wound dressing was done and scrotal support was applied (Figure 2). The child was extubated and shifted to the postoperative unit.

3 DISCUSSION
X-linked ichthyosis strikes one out of every 2500–6000 males. Usually, 15%–20% of individuals exhibit symptoms at birth, while others experience hallmarks in the following weeks. Desquamation in X-linked ichthyosis usually impacts the extensor aspect of the extremities while avoiding the nails, palms, soles, and flexor aspects of extremities. However, in our patient bilateral hands with antecubital fossa (Figures 3 and 4), bilateral lower extremities (Figure 2), scalp along with neck and face (Figure 1), and anterior and posterior trunk (Figures 5 and 6) were involved.1




Various multiple issues like corneal opacities, nystagmus, behavioral disorders, developmental delay, cryptorchidism, recurrent seizures, and anosmia are sometimes associated with classic X-linked ichthyosis.1 In our patient, cryptorchidism was the additional feature.
The fundamental method of therapy in ichthyosis seeks to alleviate skin dryness, mitigate scales, reduce unpleasant smell, and improve skin aesthetic. Utilizing emollients and keratolytic agents like lactic (5%–10%) or glycolic acid (5%–12%) and retinoic acid (0.1% cream) on a regular basis will help reduce scaling. Patients in severe variants of X-linked ichthyosis can reap benefits from systemic retinoids.1-3
The anesthetic management of children with ichthyosis is an uphill task and warrants continuous meticulous care. Gaining intravenous access is tough due to the presence of macerated scales preventing visualization of veins. Fixing the intravenous cannula with adhesive tape is frequently unsuccessful due to the crust of scales and requires bandage to secure it (Figure 3). Endotracheal tube, nasogastric tube, drains, and catheter sometimes need to be sewn to prevent dislodgement. ECG electrodes can sometimes become nonadherent and monitoring could turn messy due to inadequate signal.2, 3
The neuraxial technique is often contraindicated due to the presence of macerated scales and excoriation.2, 3 In our patient, caudal analgesic technique is avoided due to the presence of desquamated skin flakes around sacral hiatus (Figure 6). Therefore, analgesia was provided with the combination of intravenous opioids, NSAIDs, and paracetamol.
Temperature regulation is impaired, and hypothermia or hyperthermia can ensue in the perioperative period due to abnormal keratinization and impaired sweating. The use of forced air warmers could result in overheating and resultant hyperthermia and should be reserved for lengthy surgical procedures. Hypothermia can be avoided by providing warm fluids, covering the exposed body parts with sheets, using warm irrigation fluids to wash surgical wounds, regulating theater temperature, and using warmers in case of prolonged surgical procedure.2 These patients are susceptible to develop postoperative wound infection. Hence, pre-operative and postoperative antibiotic prophylaxis should be well suited according to the type of surgical procedure.3
If a child has associated ectropion, eye protection is advised with the use of lubricant eye drops and covering the eyes with tape.3 The child could have psychological issues from unhealthy appearance, and it should be addressed by involving a child psychologist in the team.2
4 CONCLUSION
To effectively manage X-linked ichthyosis perioperatively, rigorous planning and proficient anesthetic management are crucial. This entails airway management, venous access, monitoring (electrocardiogram, bispectral index, entropy, neuromuscular blockade monitoring), preventing ocular trauma, and maintaining normothermia. Managing ichthyosis is generally a multidisciplinary endeavor that requires close coordination and communication among caregivers from different specialties.
AUTHOR CONTRIBUTIONS
Sunil Bhatta: Conceptualization; formal analysis; methodology; resources; validation; writing – original draft. Sukriti Pandit: Resources; writing – review and editing. Pratik Chaudhary: Resources; writing – review and editing. Naresh Thapa Chhetri: Resources; writing – review and editing.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST STATEMENT
Non conflict of interests.
CONSENT
Written and informed consent was obtained from the patient's mother for the publication of the case report, which is available for review by the editor of this journal.
ETHICAL APPROVAL
Ethics approval of this case report is not needed in accordance with local ethical guidelines.
Open Research
DATA AVAILABILITY STATEMENT
Data described to support the findings are openly accessible in the article.