Beyond the obvious: A case presentation on the misdiagnosis of posterior femoral cutaneous nerve entrapment as semitendinosus muscle tear
Key Clinical Message
To underscore the importance of evaluating the entrapment of the posterior femoral cutaneous nerve (PFCN) in patients exhibiting symptoms in the posterior thigh region. A 42-year-old male dentist, initially diagnosed with a semitendinosus muscle tear and persistent pain and tingling in the posterior thigh, sought treatment at our outpatient clinic. Despite unsuccessful physiotherapy, a comprehensive evaluation revealed an unusual entrapment of the PFCN between the sacrotuberous ligament and the semitendinosus muscle stump. The patient was subjected to a series of specialized therapeutic interventions, including soft tissue release, kinesiology taping, and lifestyle modifications. The patient's symptoms, including pain and tingling, were completely resolved, enabling him to sit on a stool for extended periods without discomfort. This case presentation emphasizes the need for physical therapists to consider the possibility of PFCN entrapment in patients experiencing pain and tingling in the posterior thigh. These symptoms can be easily mistaken for conditions such as sciatica or a hamstring muscle tear.
1 INTRODUCTION
The posterior femoral cutaneous nerve (PFCN) is a highly variable sensory nerve arising from the anterior and posterior rami of the first three sacral nerves, as well as the anterior divisions of S2 and S3, and the posterior rami of S1–S3.1 Its anatomy encompasses a wide range, potentially including branches extending from as high as L4 to as low as S4.1 Emerging beneath the gluteus maximus alongside the inferior gluteal artery, the PFCN passes through the sciatic foramen beneath the piriformis muscle, then travels down the buttock and thigh along the medial aspect of the sciatic nerve, occasionally referred to as the “lesser sciatic nerve”.1 This long cutaneous nerve exits the pelvis through the sciatic foramen, coursing inferiorly down the posterior thigh and providing extensive sensation to various regions, including two-thirds of the posterior thigh, the entire infragluteal fold, and small portions of the lateral anal/perineal region through its numerous terminal branches.1, 2
Entrapment of the PFCN is an uncommon, potentially under-recognized cause of low back, buttock, perineal, and posterior and lateral thigh pain and tingling. Most reports of nerve injuries related to the PFCN are caused by intramuscular injections.2 There are also reports of injuries due to other factors such as hematoma or tumor formation,3 piriformis hypertrophy,4 operations like above-knee amputation with a thigh pressure cuff,5 or posterior hip replacement.6 Other causes include abnormal venous formations,7 pressure injuries against the sciatic tuberosity or the inferior margin of the gluteus maximus from sitting on hard surfaces or falls,1, 3 and hamstring injuries due to their proximity to the origin of the hamstring muscle.8
The PFCN injuries have been reported in cases involving hamstring pathology, such as hamstring tears, as well as surgeries and other trauma affecting pelvic neurovasculature.9 This case report presents a unique scenario where the PFCN was impinged between the sacrotuberous ligament and the stump of the semitendinosus muscle, which was used as a graft for anterior cruciate ligament (ACL) reconstruction.
2 CASE HISTORY AND EXAMINATION
In August 2023, a 42-year-old man weighing 105 kg and standing at a height of 1.81 m visited the outpatient clinic due to persistent and worsening pain and tingling in the posterior of his right thigh, which had been bothering him for 3 months. The onset of symptoms occurred after he went mountain climbing 3 months ago, during which he walked backward with slightly flexed knees and took short steps for about one and a half hours. Later that night, he felt discomfort in the upper posterior region of his right thigh, which he first thought was just muscle soreness from the climb. However, when the pain continued and he started feeling tingling in the posterior of his right thigh, he became worried (Figure 1). He found relief by using a hot pack under his right thigh for about 20 minutes. Furthermore, his sedentary job requires him to sit for extended periods of time, and the symptoms tended to get worse at night, although he did not feel any pain while walking or running.
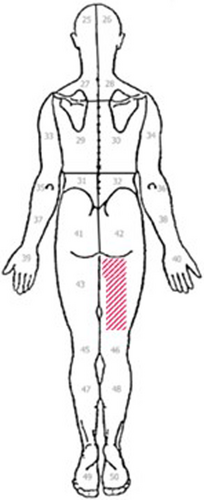
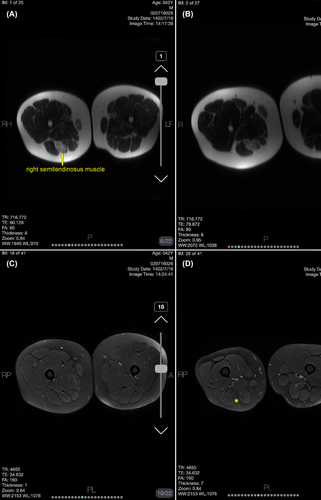
Following a month of persistent symptoms, the patient consulted an orthopedic specialist who recommended an magnetic resonance imaging (MRI) for the posterior thigh muscles, as there was no history of low back pain. The MRI results revealed a high-grade tear in the semitendinosus muscle, located in the distal part of the hamstring muscle (Figure 2). Subsequently, the patient underwent five sessions of physiotherapy at a physiotherapy center, which included electrophysiological modalities such as ultrasound, transcutaneous electrical nerve stimulation, low-level laser therapy, and hamstring setting exercises. However, these interventions did not result in significant improvement of the symptoms, leading to the patient's referral to our physiotherapy center. It is noteworthy that the patient has no history of tobacco use or alcohol consumption, and he does not have any underlying health conditions such as systemic illnesses, metabolic disorders like diabetes, or inflammatory disorders, nor does he use any medications.
3 METHODS
3.1 Differential diagnosis, investigations, and treatment
In the assessment room, the patient exhibited a normal gait pattern, aligned posture, and symmetrical weight distribution on both legs. No signs of ecchymosis, edema, or muscle atrophy were observed at the site of symptoms. The skin color and hair growth in the affected region appeared normal compared to the unaffected side. A scar tissue was observed below the patellar bone on the front of the right knee, attributed to ACL reconstruction surgery performed 5 years ago. It was clarified that the observed muscle asymmetry between the right and left thigh was a result of the surgical procedure rather than an acute traumatic high-grade tear of the semitendinosus muscle.
During the examination, the right hip joint showed a full range of active and passive movements without associated pain. The isometric resistance test of the semitendinosus muscle in the affected leg showed reduced strength compared to the unaffected side but did not cause discomfort. To rule out lumbar spine, sacroiliac joint, and piriformis muscle disorders, several special tests were conducted, including straight leg raise,10 slump test while seated on the treatment table,10 distraction test,10 compression test,10 flexion, abduction, and external rotation (FABER) test,10 Gaenslen's test,11 thigh thrust test,10 active piriformis stretch test,12 ipsilateral lateral rotation of the right leg,10 Freiberg's maneuver,13 and flexion, adduction, and internal rotation (FAIR) test.10
In order to assess the PFCN near the sacrotuberous ligament, the examiner exerted pressure on the nerve situated between the sacrotuberous ligament and the stump of the semitendinosus muscle using his thumbs. This pressure was sustained for a duration of 30 s (Figure 3). The patient's symptoms were triggered in a way that matched his initial complaints. However, applying pressure along the path of the nerve branch in the thigh did not elicit these symptoms. Therefore, the authors decided to release the soft tissues adjacent to the PFCN near the inferior gluteal fold.

The therapeutic process was carried out by a physical therapist, who holds a PhD in the field and has 14 years of experience in treating musculoskeletal disorders. The primary goal of the procedure was to relieve tension in the sacrotuberous ligament. The physical therapist employed a two-handed technique, with one hand positioned on the ischial tuberosity side of the ligament and the other hand performing small, back-and-forth sliding motions.14 This method was employed to initially relax and subsequently stretch the sacrotuberous ligament (Figure 4).14 In addition, kinesiology taping was applied to reduce soft tissue tension near the PFCN. To alleviate tension on the sacrotuberous ligament and semitendinosus muscle, I-strips of kinesiology tape (Ares Tape®) were carefully applied with a tension of 25% (Figure 5). Furthermore, the patient was advised to use a small cushion when sitting on a stool to provide support.


Each treatment session lasted for 30 min, and the patient underwent a total of four sessions, with a day of rest between treatments, to achieve symptom relief.
4 OUTCOME AND FOLLOW-UP
After four treatment sessions, a significant reduction in pain and tingling in the area of symptoms in the posterior aspect of the right thigh was observed. The patient reported no symptom provocation after prolonged periods of sitting on a stool during work-related tasks. During the two-month follow-up period post-treatment, the patient did not report any discomfort, demonstrating the effectiveness of our therapeutic intervention.
5 DISCUSSION
This case report presents a 42-year-old male patient who underwent physiotherapy assessment and treatment for PFCN compression adjacent to the sacrotuberous ligament and the stump of the semitendinosus muscle. The PFCN is a sensory nerve that runs adjacent to the sciatic nerve and can be compressed by the piriformis muscle or injured by prolonged tourniquet.9 Compression or pressure on the PFCN as it passes through or near the sacrotuberous ligament can also lead to PFCN entrapment.1 In addition to these factors, intramuscular gluteal injections have been identified as a potential cause of PFCN entrapment, as the needle can damage the nerve or surrounding structures.9 Furthermore, prolonged bicycle rides, pelvic tumors, venous malformations, and pressure on the nerve at the inferior margin of the gluteus maximus due to sitting on hard surfaces have also been associated with PFCN trauma.9
The PFCN entrapment is an under-recognized cause of posterior thigh and perineal pain. The pain patterns associated with PFCN entrapment can be complex and overlapping, often leading to misdiagnosis as sciatica. Therefore, it is crucial to actively investigate the underlying cause of PFCN entrapment for an accurate diagnosis. The diagnosis of PFCN entrapment primarily relies on a thorough physical examination, ruling out potential issues in adjacent joints and muscles such as sacroiliac joint dysfunction, lumbar spine problems, and piriformis muscle tightness. Special attention should be given to symptoms located between the heads of the hamstring muscles at the ischium or along the nerve distribution behind the thigh. While ultrasound and MRI are available diagnostic tools, Murinova et al.1 suggested that physical examination remains more effective in diagnosing PFCN entrapment compared to imaging modalities.
The presented case in this paper is intriguing, as the patient was initially misdiagnosed with a high-grade tear of the semitendinosus muscle following participation in a recreational mountain climbing activity. The activity involved a rapid transition from decelerating knee extension to hip joint extension, which is known to make the two-joint muscle susceptible to strain.15 Petersen and Hölmich16 have highlighted that this specific biomechanical transition puts these muscles at the highest risk of injury. The patient exhibited tenderness to palpation and induration in the posterior thigh along the hamstring muscle bellies, which aligned with the clinical findings of a high-grade tear of the semitendinosus muscle. Furthermore, the absence of edema and bleeding on the MRI conducted 1 month after symptom onset further supported this diagnosis. Consequently, the patient was referred for physical therapy to alleviate his symptoms. However, the patient's symptoms persisted when he sat on a dentistry stool for an extended period.
The prevalence of PFCN entrapment appears to be quite low, as there is currently no valid reference reporting the prevalence of this condition. Additionally, the entrapment of the PFCN is not routinely evaluated in patients presenting with symptoms such as pain, tingling, or tingling in the posterior buttock and thigh regions. Initially, patients with these symptoms may be diagnosed with sciatica or sacroiliac joint dysfunction. However, this case presentation highlights that PFCN entrapment could be an alternative explanation for these symptoms, as the major sensory branch of the PFCN innervates and generates pain in the skin of the posterior thigh, popliteal fossa, and upper part of the leg. Previous studies have explored various therapeutic options for PFCN entrapment, such as the landmark- or image-guided anesthetic nerve injections, which have shown significant pain relief in patients with persistent PFCN pain.17, 18 However, further studies are needed to confirm the validity of these injection techniques in real patient cohorts. It is crucial to acknowledge that nerve blockade injections carry the risk of serious adverse effects, such as bleeding, rash, itching, soreness at the injection site, and infection.19 These potential adverse effects should be taken into consideration when considering nerve injection procedures.
In our study, we opted for a conservative approach to releasing soft tissues around the PFCN, as informed by our examination results. We applied a stretching force to the sacrotuberous ligament while stabilizing the ischial tuberosity. To maintain the release of the ligament, we employed kinesiology taping with a 25% stretch. Additionally, the Gate Control Theory of pain posits that the mechanical stimulus delivered by the tape acts through large-diameter non-nociceptive fibers, leading to pain inhibition and relief.20 This study provides evidence that releasing the soft tissues around the PFCN can lead to an improvement in symptoms for patients experiencing pain and tingling in the posterior region of the thigh.20 Changes in soft tissue hardness may affect the pain perception of the human skin.20 Weerapong et al.21 reported that changes in muscle flexibility, rearrangements of muscle structure and relaxation of muscle fibers help in relieving pain. They argued that these muscular modifications block pain signals through presynaptic inhibition or increase pain pressure threshold values by reducing or preventing pain signals from reaching the level of consciousness.21
6 CONCLUSION
This case presentation describes an interesting scenario involving a male dentist who was referred to our physical therapy clinic with complaints of pain and tingling in the posterior portion of the thigh. Initially, he was misdiagnosed with a torn semitendinosus muscle. However, upon detailed examination, it was discovered that the pain and symptoms were actually caused by entrapment of the PFCN between the sacrotuberous ligament and the stump of the semitendinosus muscle. To address this issue, a manual technique was used to release the entrapped ligament, followed by the application of kinesiology taping on the sacrotuberous ligament and the semitendinosus muscle. Remarkably, these interventions led to a complete resolution of the patient's symptoms.
AUTHOR CONTRIBUTIONS
Mohammadreza Pourahmadi: Conceptualization; data curation; supervision; writing – original draft; writing – review and editing. Alireza Yaseri Gohari: Conceptualization; writing – review and editing. Mohammad Mahdi Ghorbani Duqaei: Investigation; writing – review and editing.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST STATEMENT
Authors declare no conflict of interest.
ETHICS STATEMENT
Due to research protocol in Iran University of medical sciences, ethical committee's approval for case reports is not needed however patient's consent for publication is obtained.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The authors affirm that the data supporting the findings of this study are available within the article.