Incidentally discovered parathyroid lipoadenoma in thyroid surgery: A case report and review of the literature
Yihan Wang and Yan Chen contributed equally to this work.
Key Clinical Message
Parathyroid lipoadenoma is a rare type of parathyroid adenoma, described as a single parathyroid adenoma with more than 50% fat on histologic examination and an unknown etiology, which is one of the rare causes of primary hyperparathyroidism. The difficulty of parathyroid lipoadenoma is mainly diagnosed by preoperative imaging localization. We hope to arouse attention to the parathyroid adenoma which is difficult to locate through our case report. The patient was a middle-aged male with a body mass index of 38.4 kg/m2 who admitted to our hospital with a 40-day history of an untreated thyroid nodule. We incidentally discovered parathyroid lipoadenoma in his thyroid surgery. His prognosis was good, and there were no signs of recurrence at his 12-month follow-up appointment. We believe that parathyroid lipoadenoma needs to rely on paraffin pathology to make a final diagnosis. This case report serves as a reminder that parathyroid lipoadenomas are also possible in patients who do not have primary hyperparathyroidism preoperatively and who have negative imaging. Clinicians must carefully examine the adipose tissue for the presence of parathyroid lipoadenomas during thyroid surgery to avoid postoperative hypoparathyroidism and persistent hypocalcaemia.
1 INTRODUCTION
Parathyroid lipoadenoma, one of the rare causes of primary hyperparathyroidism, is an uncommon type of parathyroid adenoma, described as a single parathyroid adenoma with more than 50% fat on histologic examination and an unknown etiology.1 In this paper, using “parathyroid lipoadenoma” and “parathyroid lipothymoadenoma” as search terms, the number of cases of parathyroid lipoadenoma reported on PubMed from 1962 to date was 64. We present a case that supplements and supports the rare literature data concerning the clinical and therapeutic aspects of occasional parathyroid lipoadenoma in thyroid cancer surgery in our treatment center and review the relevant literature.
2 CASE DESCRIPTION
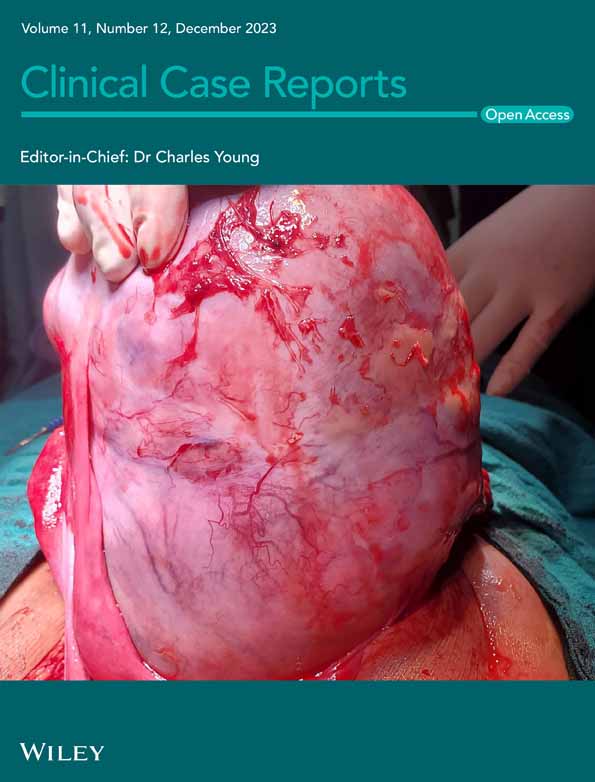
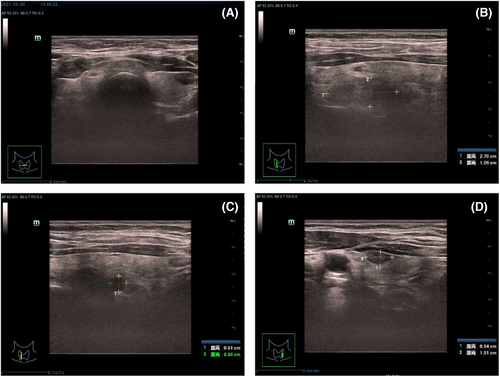
The patient was a middle-aged male with a body mass index (BMI) of 38.4 kg/m2 who visited the hospital 40 days following the identification of the thyroid nodule. The patient had no significant positive history, family history, and past medical and surgical history. Physical examination (Figure 1) showed that the thyroid gland had a firm texture and no detectable swelling; ultrasonography showed normal thyroid gland size, heterogeneous glandular echoes, patchy hypoechoic areas, the larger one was located in the right lobe, with a range of about 2.7 × 1.09 cm, a hypoechoic nodule was observed in the lower deep layer of the right lobe, with a size of about 0.61 × 0.60 cm, aspect ratio > 1, regular borders, and punctate hyperechogenicity was observed; an anechoic nodule was observed in the middle superficial layer, with a size of about 0.28 × 0.34, aspect ratio < 1, regular borders, and no significant focal hyperechogenicity was observed; a solid hypoechoic nodule was observed in the lower grade of the left lobe, with a size of about 0.54 × 1.01 cm, aspect ratio < 1, regular borders, and no significant focal hyperechogenicity was observed. No significant abnormal enlarged lymph nodes were found in bilateral neck. Cytological examination of the right thyroid lobe nodule showed atypical cells suggestive of papillary thyroid carcinoma. Thyroid function tests: thyroid stimulating hormone TSH 0.862 mIU/L (normal reference value 0.372–4.94 mIU/L); parathyroid hormone PTH 64.62 pg/mL (normal reference value 15–56 pg/mL); and serum calcium Ca 2.42 mmol/L (normal reference value 2.2–2.65 mmol/L). The patient was admitted to hospital without any abnormal results from renal function tests, and no indicators for vitamin D were assessed.
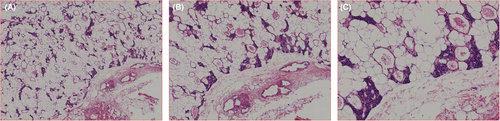
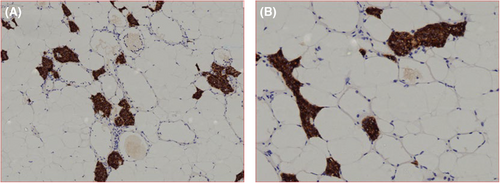
Resection of the right lobe and isthmus of the thyroid gland and central lymph node dissection were planned, during which the right lobe and isthmus of the thyroid gland were first removed, and grayish white nodules were observed in the right lobe of the thyroid gland by dissection, about 0.4 cm in diameter, and the remaining sections were grayish red and soft. During the resection, two masses measuring 1.5 × 0.8 × 0.7 cm and 2.5 × 1.5 × 0.5 cm were found in the dorsal and lateral aspects of the middle and upper parts of the right lobe, respectively. The texture was firm, the surface was smooth, and the boundary was clear. The possibility of parathyroid gland mass was considered, so the tissue for intraoperative pathological examination was removed. The results showed that round cells were scattered in the fibroadipose tissue of the middle and upper dorsa of the right lobe, not excluding the mass of parathyroid gland origin; most of the tissues submitted to the lateral aspect of the middle and lower parts of the right lobe were fat, in which a few round cells were scattered. At the same time, the left thyroid gland was dissected to explore the tracheoesophageal groove of the lower pole of the thyroid gland in its dorsal pole, and no abnormal hyperplastic parathyroid tissue was observed. PTH values were 29.68 pg/mL and 35.71 pg/mL at 15 and 30 min after tumor resection, respectively, and serum calcium was 2.30 mmol/L on the first day after surgery. Postoperative paraffin pathology (Figure 2) revealed that the superior dorsal mass and the middle and lower lateral mass in the right lobe were consistent with parathyroid lipoadenoma, and immunohistochemistry (Figure 3) revealed PTH (+); CgA (+); SyN (−); CD56 (−); TTF-1 (−); Tg (−); Ki-67 (<1% +), and the right lobe of the thyroid gland was papillary thyroid carcinoma 0.4 cm in diameter; there was one lymph node metastasis in the central group, and the diameter of the metastasis was 0.05 cm; the isthmus was nodular goiter. Euthyrox (50 μg) was orally administered daily after surgery.
One month later, the patient came to our hospital for reexamination, without perioral numbness or numbness of extremities, TSH 1.30000 mIU/L; PTH 28.51 pg/mL; Ca 2.59 mmol/L, which were within normal range. The patient's prognosis was good, exhibiting no evidence of relapse or discomfort during the 12-month follow-up appointment.
3 DISCUSSION
Parathyroid lipoadenomas are rare and are incidentally detected during thyroid cancer surgery in this case. The article reports 40 cases of parathyroid lipoadenoma reported in PubMed from 1962 to date using the search terms “parathyroid lipoadenoma” and “parathyroid lipoadenoma”,1, 2, 4, 5, 7-42 of which 65 cases of parathyroid lipoadenoma were reported (including this case). After excluding 18 cases with missing clinical data, 47 cases had complete clinical data, including 30 females and 17 males, with a female-to-male ratio of about 1.8:1, that is, parathyroid lipoadenoma accounted for a higher proportion in females than in males. In addition, it has been reported in the literature that parathyroid lipoadenoma may account for a higher proportion in males than parathyroid adenoma.2 The age of onset of parathyroid lipoadenomas varies from 24 to 88 years, mostly located in the neck, but up to 15% of parathyroid lipoadenomas are ectopic or located in the mediastinum, much higher than common parathyroid adenomas.3
In 1958, Ober and Kaiser4 first described parathyroid lipoadenoma in a middle-aged man with a gradually enlarging neck mass that was painless and without manifestations of hyperparathyroidism. A large lipoma was found under the sternum on neck exploration. Because the tumor was nonfunctional, they named it “parathyroid hamartoma.”The concept of “parathyroid lipoadenoma” was first introduced in 1962 by Abul Haj et al.1 Parathyroid lipoadenoma is a rare type of parathyroid adenoma with an incidence of 0.5%–1.6% of primary hyperparathyroidism and contains fat, principal cells, and eosinophils, of which fat content is >50%, unlike adenomas with fatty infiltration, and the fat component is an integral part of parathyroid lipoadenoma.5 In 2022, the World Health Organization defined parathyroid lipoadenoma as “a tumor with simultaneous increases in parathyroid parenchyma and adipose tissue, and more than 50% of the glandular volume consists of adipose tissue.”6 In the currently reported cases of parathyroid lipoadenoma, the origin of the adipose tissue component is unknown, and most of them are small brown lesions with the largest reported weight of 480 g. Some researchers have speculated that the factors of increased fat composition may be the same as those of increased parathyroid chief cells.7, 8 It has been suggested that fat may be present in adenomas by high BMI, and some speculations suggest that some adipogenic factors may be produced by epithelial cells or stromal cells in adenomas, which in turn stimulate adipocyte proliferation.9 Christofer Juhlin proposed that parathyroid lipoadenomas may be associated with hypertension.5
Parathyroid lipoadenomas can be categorized as either functional or non-functional. Of the cases previously reported, the majority (64%) were symptomatic, with 28% being asymptomatic and 7% displaying suspicious symptoms.10, 11 Additionally, another four cases of parathyroid lipoadenomas were uncovered during autopsy, with the ability to determine their functionality unclear. Functional parathyroid lipoadenomas exhibit clinical features and laboratory investigations similar to those of parathyroid adenomas. Patients typically experience recurrent urinary stones and hip or shoulder fractures; however, the elevation of parathyroid hormone and blood calcium caused by them may not be as prominent as in the case of parathyroid adenomas. A small number of patients may present with asymptomatic hypercalcemia.
The difficulty of parathyroid lipoadenoma is mainly diagnosed by preoperative imaging localization. 29 of 64 patients (45%) had lesions localized using imaging studies. Ultrasonography was performed in 24 cases, and lesions or suspected lesions were found in 14 (58%) of them. Computed tomography (CT) was reported in 12 cases, of which lesions were detected or suspected in 9 (75%). Technicium-99 m-sestamibi scintigraphy was reported in 15 cases, of which 8 (53%) reported detection or suspicion of lesions. In one of them, an X-ray was performed and the tumor was found to be located in the mediastinal cavity. Positron emission tomography (PET) scans were used in six cases, of which three (50%) were reported as lesions (chart 1). Because of the high adipose tissue content, lipomas tend not to be detected by preoperative imaging techniques. On ultrasound, typical parathyroid adenomas are homogeneous hypoechoic lesions, however, fat-rich variants of parathyroid adenomas sometimes present as hyperechoic lesions,9 resulting in reduced accuracy, and ultrasonography could not show parathyroid lesions in this patient; they can be localized as lipomatous masses on CT, and Johnson et al.12 reported cases in which CT scans of parathyroid lipoadenomas had CT values of −60 to −90 HU, consistent with lipoma density, proposing the possibility of parathyroid lipoadenomas on such CT scans in similar cases of non-local primary HPT. However, CT may also be confused with lipomas, lymph nodes, or other fat-rich lesions; the accuracy of dual-phase sestamibi scanning of the parathyroid depends on the proportion of parathyroid chief cells, which are more than 50% fat in parathyroid lipoadenomas and have less principal cell content than normal parathyroid tissue, resulting in reduced accuracy of sestamibi scanning; however, there are cases13 indicating the usefulness of using 99Tcm-MIBI imaging in localizing the diagnosis, reoperation, and persistent hyperparathyroidism, and they propose speculation that the lesion may be shown based on the space-occupying appearance, or that the target may have a low signal ratio to the background. Cases showed a good target-background signal ratio in Tc-99 m sestamibi imaging, which may be due to the relatively large size of the lesion, as well as the fact that the main part of the lesion consists of parathyroid chief cells; for the same reasons outlined earlier, SPECT demonstrates notably lower sensitivity in detecting parathyroid lipoadenomas.12 However, Sabri et al.1 concluded that although SPECT is not as effective as parathyroid adenoma in the diagnosis of parathyroid lipoadenoma, it may be superior to ultrasound. Cholinergic PET-CT imaging is superior to ultrasound and CT in the localization of parathyroid adenoma, but there is no relevant report for parathyroid lipoadenoma.
| Preoperative imaging localization | Cases | Positive cases | Percentage (%) |
|---|---|---|---|
| Ultrasonography | 24 | 14 | 58 |
| CT | 12 | 9 | 75 |
| Technicium-99 m sestamibi scintigraphy | 15 | 8 | 53 |
| X-ray | 1 | 1 | 100 |
| PET | 6 | 3 | 50 |
Primary hyperparathyroidism is most commonly caused by solitary parathyroid adenomas, accounting for more than 80%–85%; less commonly, parathyroid hyperplasia, parathyroid carcinoma, and multiple parathyroid adenomas.3 Parathyroid lipoadenoma is a very rare cause of primary hyperparathyroidism with an incidence of 0.5%–1.6% of primary hyperparathyroidism. In parathyroid lipoadenomas, the sensitivity of imaging is significantly reduced by low parathyroid cell concentration and excessive fat content. The presence of adipocytes in parathyroid tissue is observed in the following conditions: normal tissue, adipose hyperplasia, adipose adenoma, and carcinoma infiltrating the surrounding adipose tissue. Differentiating between these diagnoses using intraoperative rapid frozen sections is challenging. Therefore, definitive diagnosis of parathyroid lipoadenoma should include pathologic diagnosis of parathyroid hyperplasia within adipose tissue, as well as a significant decrease in hormone following intraoperative removal of the parathyroid gland. Increases in parathyroid gland weight (>40–60 mg) may also represent parathyroid lipoadenomas in appropriate morphologic and clinical settings.6 Parathyroid lipoadenomas should be considered when no lesions are reported on ultrasound but clearly identified by CT or SPECT. Parathyroid carcinoma infiltrating in adipose tissue may be misdiagnosed as parathyroid lipoadenoma, so careful pathological examination is still required for differential diagnosis.
A mass was discovered in the thyroid bed region during thyroid surgery in this case. It was excised and subjected to pathological examination, which revealed it to be a parathyroid lipoadenoma. If preoperative testing identifies the presence of a parathyroid adenoma or parathyroid lipoadenoma that is not linked to hyperfunction or other symptoms, we recommend periodic monitoring.
4 CONCLUSIONS
The high fat content present in parathyroid lipoadenomas poses a challenge for their preoperative localization and diagnosis. Therefore, we suggest that parathyroid lipoadenomas should be diagnosed based on paraffin pathology as the final and reliable diagnosis. This case report serves as a reminder that parathyroid lipoadenomas are also possible in patients who do not have primary hyperparathyroidism preoperatively and who have negative imaging. Clinicians must carefully examine the adipose tissue for the presence of parathyroid lipoadenomas during thyroid surgery to avoid postoperative hypoparathyroidism and persistent hypocalcaemia.
AUTHOR CONTRIBUTIONS
Yihan Wang: Conceptualization; data curation; investigation; methodology; writing – review and editing. Yan Chen: Data curation; investigation; writing – review and editing. Yantao Fu: Conceptualization; data curation; project administration; writing – review and editing.
ACKNOWLEDGMENTS
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Dr. Zhehui Wang (Department of Pathology, China-Japan Union Hospital of Jilin University, China) is acknowledged for providing pathological images.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest to declare.
ETHICS STATEMENT
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
CONSENT
Written patient consent has been signed and collected in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
In this paper, 40 literatures with “parathyroid lipoademona” as search term on PubMed and 65 cases of parathyroid lipoadenoma (including this case) were counted. This case comes from the Department of Thyroid Surgery, China-Japan Union Hospital of Jilin University, The authors do not wish to share the data for the sake of patient privacy protection principles.