Abdominal epilepsy, an uncommon cause of chronic and recurrent abdominal pain: a case report
Key Clinical Message
Abdominal epilepsy is an uncommon cause of paroxysmal abdominal pain. It is relatively common in children, but very rare in adults. We report a case of 38-year-old, who reported with recurrent abdominal pain for 2 years. Electroencephalography confirmed the diagnosis; he responded well to carbamazepine and remains symptom-free on follow-up.
Introduction
Abdominal epilepsy (AE) is considered to be one of the rare causes of abdominal pain 1. AE is mainly characterized by a paroxysmal episode of abdominal pain, diverse abdominal complaints, definite electroencephalogram (EEG) abnormalities, and favorable response to the introduction of antiepileptic drugs (AED) 2.
Making diagnosis for AE can be very challenging; some patients with AE have been considered to have psychogenic abdominal pain and treated without improvement 3. Others have been exposed to explorative laparotomy without significant findings to explain the symptoms 1, 4.
According to International League Against Epilepsy, AEs are considered to be part of simple or complex partial seizures 5. This rare epileptic phenomenon should be suspected in patients with unexplained paroxysmal abdominal pain, loss or alteration of consciousness, migraine-like symptoms while the diagnosis can be confirmed with Epileptiform EEG abnormalities, and or a good response to antiepileptic drugs 6, 7.
We present a case of a 38-year-old male who presented with 2 years history of abdominal pain which was treated as a peptic ulcer disease (PUD) without any improvement. AE was suspected, “antiepileptic” medication was initiated, and the patient markedly improved. The uniqueness of this case is the fact that abdominal epilepsy is a rare presentation, especially among adults. To the best of our knowledge, there is no any reported case in Africa, as in many African settings, EEG is not readily available, and our case highlights the need to have a high index of suspicion in patients with chronic abdominal pain after excluding all common causes.
Case Report
We are reporting the case of a 38-year-old black African male patient who presented with a history of paroxysmal and recurrent abdominal pain located in the epigastric region for approximately 2 years. The pain was of burning in nature, gradual onset, nonradiating, and usually lasting for about 30 min without any specific periodicity. The pain was neither related to food intake nor was there any aggravating or alleviating factors were reported. The patient reported the history of bloating; however, there was no history of nausea or vomiting. There was the history of lethargy, but there was no history of altered level of consciousness or confusion. The patient reported a positive family history of epilepsy for his paternal grandfather but no history of symptoms suggestive of a migraine headache in the family. The above symptoms were being managed as peptic ulcer disease (PUD) on several occasions with proton pump inhibitors (rabeprazole injection, oral rabeprazole, on another occasion pantoprazole) and triple therapy (esomeprazole, clarithromycin, and amoxicillin) with no improvement. He was also given different types of analgesics, antihistamines, and multivitamins also without improvement.
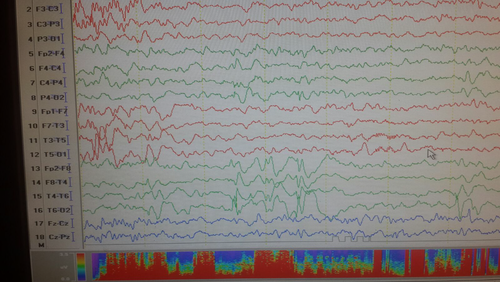
Physical examination, including abdominal examination and neurological examination, was unremarkable. Laboratory findings were all within normal range. The patient's complete workup included stool and urine examination, complete blood count, liver function test, serum amylase, and serology for Helicobacter pylori. Imaging including abdominal ultrasound, barium studies, and gastro-duodenoscopy were all normal. At this point, the possibility of abdominal epilepsy, abdominal migraine, and functional dyspepsia became more apparent. A 30-min awake electroencephalography was ordered and revealed local spikes and wave discharge with phase reversal on the right and left the temporal region which occurred during hyperventilation, and these findings confirmed the diagnosis of abdominal epilepsy (see Fig. 1).
The patient was initiated on carbamazepine 200 mg daily as a night time dose of which he was totally adherent to and reported no side effects and followed up after 1 month. Upon return to the clinic, the patient reported significant improvement. It is now more than 6 months since he had his last episode abdominal pain.
Discussion
Abdominal epilepsy is relatively an uncommon syndrome which presents with abdominal complaints resulting from seizure activity. This syndrome is characterized by unexplained, paroxysmal abdominal complaints, symptoms of central nervous system disturbance, an abnormal EEG with findings corresponding with seizure activity, and response to anticonvulsant 8. In one review, the most common gastrointestinal symptoms include abdominal pain, nausea, and vomiting, while the most common neurological symptoms include lethargy and confusion 8.
The syndrome has been well documented in children 2, 9, 10. However, there are very few reported cases among adults 11, 12. The paucity of reported cases in adults might be explained by the failure to suspect and diagnose AE in adults. One case series reported two patients aged 50 years and above 1. A more recent study showed that epileptic pain including abdominal pain is a rare symptom of seizures in both children and adults 13. Despite the scarcity of described cases among adults, there are several case reports of abdominal epilepsy in children 1, 10, 14. One study involving 150 children with chronic recurrent abdominal pain found that 74% of them had abdominal epilepsy 2.
The pathophysiology of AE is not well understood although several mechanisms have been proposed including the one which holds that abdominal epilepsy results from abnormal brain activity arising from temporal lobe which involves the amygdala. The amygdala then relays neurotransmission to gastrointestinal tract via dense direct projections to the dorsal motor nucleus of the vagus nerve through which gastrointestinal symptoms are said to originate. The hypothalamus is also thought to activate sympathetic pathways from amygdala to gastrointestinal tract to induce gastrointestinal symptoms. Patients with AE usually present with abnormal EEG demonstrating temporal lobe seizure disorders, although extratemporal origin such as parietal and temporal regions has also been reported 15.
There are four diagnostic criteria for AE. These are (i) otherwise unexplained, paroxysmal gastrointestinal complaints, (ii) symptoms of a CNS disturbance, (iii) an abnormal EEG with findings specific for a seizure disorder, and (iv) improvement with anticonvulsant drugs. Our patient fulfilled all four diagnostic criteria. He had unexplained, paroxysmal gastrointestinal complaints, lethargy (CNS disturbance), suggestive EEG findings, and sustained response to anticonvulsant. The most common differential for AE is an abdominal migraine. In patients presenting with a headache, it is very difficult to differentiate AE and abdominal migraine because symptoms usually overlap. Duration of the symptoms may be used to differentiate the two; the duration is longer in a migraine than in AE 8. EEG is usually abnormal in AE and may be used to confirm the diagnosis of AE.
We followed syndromic approach toward establishing a diagnosis; clinically, our patient met four of the set diagnostic criteria. In resources, limiting situation initiation of antiepileptic can be crucial regardless of the EEG findings which could differentiate AE from an abdominal migraine or functional dyspepsia both of which may respond well to antiseizure medications.
Conclusion
Our patient presented with recurrent abdominal pain as the main presenting feature of epilepsy. Despite being a rare symptom of seizures, the diagnosis of abdominal epilepsy should be considered in patients with recurrent attacks of severe abdominal pain after exclusion of other common conditions. A high index of suspicion is required to diagnose this condition especially in resource-limited settings where in most cases, EEG is not readily available.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Acknowledgment
We acknowledge the staff of Paradize specialized clinic for their support.
Conflict of Interest
The authors have no conflict of interest to declare.