A Case Report of Fourth-Degree Facial Burns Treated With Modified Traditional Chinese Medicine Combined With Laser Therapy
Funding: This work was supported by Featured Clinical Discipline Project of Shanghai Pudong, PWYts2021-16 and Characteristic Specialist Center for Burns and Wound Repair, 25-TZBZX-01.
ABSTRACT
This case report demonstrates the successful management of a 42-year-old male with fourth-degree facial burns using an integrated approach combining modified TCM and laser therapy. Following 12 months of combined treatment and 18 months of follow-up, the patient exhibited no evidence of scar hyperplasia or subcutaneous adhesions. This therapeutic strategy synergizes the systemic regulatory effects of TCM with precision laser technology, offering a clinically reproducible approach with significant translational potential. Our findings underscore two critical principles: (1) scar prevention supersedes corrective treatment, and (2) optimal scar outcomes originate from meticulous initial wound management. The case substantiates that comprehensive resolution of wound necrosis (“decay”) yields superior long-term results compared to expedited wound closure alone.
1 Introduction
Burn injuries result from exposure to thermal, chemical, electrical, or radiation sources. Burn depth is a critical determinant of clinical management, particularly the need for surgical intervention. Superficial (first-degree) burns, limited to the epidermis, are typically painful but heal without scarring and rarely require surgery. Partial-thickness (second-degree) burns extend into the dermis and are characterized by blister formation, with severity ranging from superficial (moist, hyperemic, blanching) to deep (dry, insensate, nonblanching). In contrast, full-thickness (third-degree) and fourth-degree burns, which involve deeper tissues (e.g., muscle or bone), often appear necrotic and insensate, necessitating surgical intervention and frequently resulting in significant scarring [1].
Burn management encompasses acute resuscitation, wound assessment, surgical excision, grafting, and long-term scar rehabilitation. Key challenges include infection control, fluid balance, pain management, and specialized care for high-risk populations (e.g., children and the elderly) [2-4]. Conventional treatments such as debridement, skin grafting, and biological dressings have limitations, including cost, infection risk, and scar formation. Traditional Chinese medicine (TCM) has shown promise in wound healing due to its anti-inflammatory, antioxidant, and fibroblast-stimulating properties [5, 6].
Pathologic scarring arises from dysregulated wound healing, involving prolonged inflammation, excessive proliferation, and aberrant remodeling [7]. Clinically, this manifests as pain, pruritus, functional impairment, and disfigurement. Fractional laser therapy has emerged as an effective scar treatment, utilizing controlled microthermal damage to stimulate tissue regeneration and remodeling [8].
2 Case History/Examination
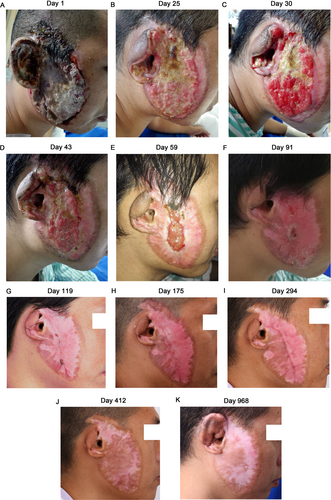
A male patient was admitted with a 1% total body surface area (TBSA) deep burn affecting the right face and ear, due to the hot crush injury. Physical examination identified a 12 cm × 6 cm fourth-degree burn involving underlying muscle and auricular cartilage, with focal necrosis and tissue loss (Figure 1A).
3 Differential Diagnosis, Investigations and Treatment
Given the clear etiology, no differential diagnosis was required. Admission blood tests revealed inflammatory markers. The patient had no significant comorbidities (e.g., diabetes or immunodeficiency) and maintained good nutritional status.
We implemented a standardized clinical protocol for this patient, consistent with our institutional approach for small-area deep burns (< 10% TBSA). The treatment was divided into three distinct phases based on wound healing pathophysiology.
3.1 Acute Phase (Inflammatory Phase): Day 1–25
Burn wounds are characterized by plasma leakage, leading to moist, exudative surfaces due to increased vascular permeability. Exposure of nerve endings causes localized pain and tenderness, while full-thickness burns develop a dry, leathery eschar composed of necrotic tissue. The inflammatory phase involves neutrophil and macrophage infiltration to clear debris and initiate repair. During this phase, Kushen ointment was applied for analgesia and anti-inflammatory effects. Kushen ointment is formulated from various Chinese medicinal ingredients, including KuShen (Radix Sophora Flavescens) 30 g, HuangQi (Radix Astragali Seu Hedysari) 15 g, DangGui (Radix Angelicae Sinensis) 15 g, and BingPian (Borneolum) 15 g. After being powdered, they are mixed with ZhiMaYou (Sesamum Indicum) and FengMi (Mel).
Dongju lotion was used for wound cleansing and debridement, effectively removing necrotic tissue and microbial contaminants while preserving viable tissue, thereby promoting autolytic debridement, reducing bacterial load, and creating an optimal environment for subsequent healing phases. Dongju lotion is made from Chinese medicinal materials including RenDongTeng (Lonicerae Japonicae Caulis) 20 g, YeJuHua (Chrysanthemum Indicum) 20 g, JinJi (Schizonepeta Tenuifolia Briq) 10 g, DaHuang (Rheum Palmatum L) 10 g, ShuiZhi (Hirudo) 3 g, LvCao (Humulus Scandens) 15 g, and YiMuCao (Leonurus Japonicus Houtt)15 g. Soak the ingredients in 500 mL of clear water for 2 h, then bring to a boil. After boiling, reduce the heat and simmer for 30 min. Filter out 150 mL of the decoction, then add 250 mL of clear water to the remaining residue and continue boiling for another 30 min. Combine the two decocted liquids and add warm water (35°C–37°C) to achieve a final volume of approximately 3000 mL.
3.2 Wound Healing Phase (Proliferative Phase): Day 26–91
As wound inflammation subsides, necrotic tissue gradually sloughs off, and new granulation tissue forms at the wound base. Concurrently, vascularized granulation tissue develops, and peripheral reepithelialization begins, marking the transition to the proliferative phase. Clinically, this shift necessitates a change from anti-inflammatory/debridement therapies to interventions that promote tissue regeneration. Dongju lotion was used to remove necrotic tissues on the surface of wounds and reduce inflammation, and Shaoshang Zhangpi ointment was used to promote wound healing and facilitate scab shedding. Apply an appropriate amount of Shaoshang Zhangpi ointment evenly to the wound, and then cover it with sterile gauze or cotton pads. Secure the dressing in place and change it once a day until the wound has healed. Shaoshang Zhangpi ointment is made from Chinese medicinal materials including HuangQi (Radix Astragali Seu Hedysari) 30 g, DangGui (Radix Angelicae Sinensis) 30 g, DanShen (Radix Salviae Miltiorrhizae) 30 g, BaiZhi (Radix Angelicae Dahuricae) 20 g, LiuJiNv (Herba Artemisiae Anomalae) 20 g, GanCao (Radix Glycyrrhizae) 20 g, and BingPian (Borneolum) 5 g. After being powdered, they are mixed with ZhiMaYou (Sesamum Indicum). All the aforementioned TCM preparations were produced by the Seventh People's Hospital Affiliated to Shanghai University of Traditional Chinese Medicine. We adhere to established protocols to ensure the consistency and quality of the traditional medicine formulations. Fully automated pharmaceutical machines are used to manufacture these preparations, ensuring quality control. The samples of the Chinese medicinal materials and the prepared Chinese medicines are stored in our hospital. During the later stages of wound healing when necrotic tissue has been fully cleared and only clean granulation tissue remains, topical application of Shaoshang Zhangpi ointment alone is sufficient to support further tissue repair.
3.3 Scar Management Phase (Remodeling Phase): Day 92–412
Hypertrophic scarring, characterized by raised, erythematous, and fibrotic tissue confined to the original wound boundaries, represents a common complication of burn injuries. These scars are frequently accompanied by pigmentary disturbances, manifesting as either hypopigmentation or hyperpigmentation. While scar maturation occurs gradually through remodeling processes that improve pliability and reduce erythema over 12–24 months, complete restoration of native skin architecture and function is never achieved. Therefore, anti-scar treatment should be initiated promptly after burn wound closure. An ultra-pulsed CO2 lattice laser assisted with Kushen ointment was used to inhibit scar formation. After treatment with the ultra-pulsed CO2 lattice laser, a new superficial wound was created. Then, approximately 1 mm of Kushen ointment was applied to the wound site continuously for about 1 week, until the scab falls off. The laser treatment, along with Kushen ointment, was administered once a month until the scar ceases to progress.
4 Outcome and Follow-Up
After 1 month of treatment, new skin tissue had formed at the edges of the wound; however, a significant amount of necrotic tissue remained attached to the burned area in the center (Figure 1A–C). After 3 months of treatment, the burn wound had nearly healed (Figure 1D–F). Throughout the entire wound management process, antibiotics were never administered, and the patient did not experience any systemic infection. Subsequently, we discontinued wound treatment and proceeded with the first session of laser therapy. After 13 laser therapy sessions, the wound exhibited substantial epithelialization (Figure 1G–J) with marked improvement in scar assessment parameters (Table S1,S3). Following a follow-up period of one and a half years, the treated area showed no signs of contracture, hypertrophic scarring, or subcutaneous adhesions (Figure 1K and Video S1).
5 Discussion
Burn injuries result in long-term physiological and functional alterations that persist beyond wound closure, necessitating comprehensive management to optimize patient outcomes and quality of life [1, 9]. Achieving high-quality wound healing with minimal scar formation remains a critical therapeutic goal.
Current standard therapies include silver sulfadiazine, the first-line antimicrobial agent for burn infections, which exhibits broad-spectrum activity against Gram-positive, Gram-negative, and fungal pathogens [10]. Enzymatic debridement with bromelain-based agents (e.g., NexoBrid) has emerged as an effective adjunct for mixed-depth dermal burns, primarily through selective removal of necrotic tissue rather than direct antimicrobial effects [11, 12]. TCM conceptualizes burn wounds as “ulcers” attributed to tissue “decay.” The principle of “removing decay and promoting regeneration” aligns with modern debridement strategies [13]. TCM formulations enhance phagocytic activity of neutrophils and macrophages, facilitating necrotic tissue clearance and inflammatory resolution [14]. This mechanism complements conventional approaches by modulating the wound microenvironment during critical healing phases.
The primary advantage of TCM lies in its multicomponent nature, allowing for simultaneous targeting of multiple pathways and producing synergistic effects [15]. Traditional hemostatic drugs, such as DanShen (Radix Salviae Miltiorrhizae), SanQi (Radix Notoginseng), and JiangHuang (Curcumae Longae), have been extensively utilized in wound healing [16]. KuShen (Radix Sophora Flavescens), traditionally used to treat damp-heat syndromes [17], contains over 200 bioactive compounds, primarily flavonoids and alkaloids. Studies demonstrate its extracts exhibit broad pharmacological effects including anti-inflammatory, antimicrobial, and antipyretic activities [18]. The therapeutic mechanisms involve modulation of critical signaling pathways, particularly the NF-κB-mediated inflammatory response and Nrf2-ARE antioxidant pathway, as demonstrated by extracts of Chrysanthemum zawadskii and Glycyrrhiza uralensis [19]. Other components like carboxymethylated polysaccharides from YeJuHua (Chrysanthemum indicum) contribute antimicrobial and hemostatic properties [20], while RenDongTeng (Lonicerae Japonicae Caulis) shows protective effects against cell injury through MAPK pathway inhibition [21]. Several TCM herbs including HuangQi (Radix Astragali Seu Hedysari), DangShen (Radix Codonopsis Pilosulae), BaiZhu (Rhizoma Atractylodis Macrocephalae), DangGui (Radix Angelicae Sinensis), and BaiZhi (Radix Angelicae Dahuricae) exhibit antitumor and immunomodulatory effects through cell cycle regulation and apoptosis induction [22, 23]. These compounds modulate key signaling pathways including Wnt, PI3K/Akt, NF-κB, TGF-β/Smad, to promote diabetic wound healing by balancing inflammatory responses and oxidative stress [24]. Recent studies further demonstrate their ability to enhance neural stem cell proliferation and migration [25]. The oil-based vehicles in TCM preparations provide additional benefits by maintaining optimal wound moisture. However, despite promising clinical applications in various wound types [26], further research is needed to standardize formulations and evaluate long-term safety profiles. TCM treatments may lead to adverse wound healing effects, such as local irritation and allergic reactions. The integration of TCM's multitarget approach with conventional therapies represents a promising treatment strategy that warrants rigorous clinical investigation.
Our protocol recommends initiating combined laser and Kushen ointment therapy immediately after wound closure, continuing until scar stabilization. Adjunctive therapies including scar massage, pressure therapy, and silicone gel sheet application should be incorporated. Treatment endpoints include: normalized skin color without erythema/hyperpigmentation, soft pliable texture without induration, stable scar thickness, and absence of pruritus or pain. This combined approach achieved excellent esthetic and functional outcomes in our patient without wound contracture or pathological scarring.
While our nonsurgical protocol requires longer treatment duration than operative approaches, it avoids the need for repeated debridement, autografting, or expensive biological dressings, reducing hospitalization costs by approximately 50% (~$4000). The favorable safety profile and patient tolerance further enhance its clinical utility. However, treatment efficacy may be limited in patients with extensive burns (> 20% TBSA) or significant comorbidities, as seen in our healthy patient with optimal outcomes.
This case demonstrates that simply achieving wound closure without addressing the pathological wound microenvironment (“decay”) may be insufficient. Although time-intensive, our approach effectively minimizes late scar complications. While promising for small-area deep burns, limitations include prolonged treatment courses and compliance demands. Further evidence-based evaluation is needed to optimize TCM integration into burn care.
Author Contributions
Yating Yin: data curation, investigation, supervision, writing – original draft, writing – review and editing. Shun Xu: funding acquisition, investigation, methodology, resources, supervision, visualization, writing – review and editing.
Ethics Statement
Ethical approval for the study was granted by the ethics committee of the Seventh People's Hospital Affiliated to Shanghai University of Traditional Chinese Medicine (2023-7th-HIRB-040). A written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.