Encephalopathy and Endophthalmitis Following Device-Related Invasive Clavispora Lusitaniae Infection in an Immunocompetent Patient: A Case Report
Funding: This work was supported by Taishan Scholar Project of Shandong Province, tsqn202103165.
Yi Cui, Zhenxing Huang and Hui Han are contributed equally to this work.
ABSTRACT
Device-related Candida infections are becoming more prevalent, even among immunocompetent individuals. For patients diagnosed with invasive candidiasis, it is essential to perform a fundoscopic examination, irrespective of the presence of ocular symptoms. If infected implanted devices cannot be removed, individualized antifungal regimens and long-term treatment are crucial.
1 Introduction
Candidiasis is an infectious disease caused by various pathogenic species of Candida, most frequently occurring in immunocompromised patients. Invasive candidiasis encompasses both candidemia and deep-seated tissue infections [1]. Common and severe complications of invasive candidiasis, such as central nervous system (CNS) involvement and endophthalmitis, are associated with high mortality [2]. Multiple fungal species within the Candida genus can lead to invasive candidiasis, with Candida albicans being the most prevalent [1]. Invasive infections caused by Clavispora lusitaniae (C. lusitaniae) are rare, with most strains exhibiting intrinsic resistance to amphotericin B. In recent years, infections caused by C. lusitaniae have been increasingly reported, often associated with conditions such as immunosuppression, chemotherapy, malignancy, and organ transplantation [3]. Cases of invasive candidiasis caused by C. lusitaniae in immunocompetent patients are rare. Furthermore, C. lusitaniae has demonstrated resistance to amphotericin B [4]. The use of indwelling medical devices has been steadily increasing, paralleled by a rising incidence of Candida-related device infections [5]. Here, we present a case involving a patient with normal immune function who developed an invasive C. lusitaniae infection associated with an artificial vascular graft. This infection disseminated through the bloodstream, leading to ischemic and hemorrhagic strokes in the right cerebral hemisphere, right endophthalmitis, and skin involvement on the right hand. Due to the inability to perform further surgical intervention, we opted for purely medical treatment. During the course of treatment, different antifungal regimens, including caspofungin, fluconazole, and 5-flucytosine (5-FC), were administered at various stages of infection. After a long-term follow-up of 2 years, the patient recovered from this severe case of invasive candidiasis.
2 Case History/Examination
A 46-year-old man underwent ascending aortic and total arch replacement using the stented elephant trunk technique, along with coronary artery bypass grafting, due to aortic dissection and coronary artery disease two years ago. Over the past two months, he has experienced recurrent episodes of fever and chills, with a peak temperature of 40.4°C, prompting him to seek treatment at a local hospital. A summary of the disease course is presented in Table 1.
| Timeline since admission to our institution | Events |
|---|---|
| Nearly 2 months ago | Fever presentation |
| About 1 months ago |
C. lusitaniae was identified in blood culture Caspofungin applied PET-CT |
| 1 day ago | Stroke was found in MRI |
| Admission day |
Rechecked blood culture observed C. lusitaniae Caspofungin applied continuously |
| Day 2 |
Brain CT confirmed hemorrhage in the right parietal lobe CTA found filling defect in the inner wall of the proximal brachiocephalic trunk Fluconazole was added with a load dosage of 800 mg and 400 mg qd |
| Day 5 | Candida endophthalmitis observed |
| Day 8 |
Generalized convulsions MRI and lamber puncture were performed Voriconazole intravitreal injections started |
| Day 10 | Fluconazole adjusted to 800 mg qd combined 5-Flucylosine replaced caspofungin for next 28 days |
| Day 13 and Day 14 |
Brain lesion improved Right eye lesions improved |
| Day 16 | Discharged |
| Day 22 | Right eye lesions recovered |
| Day 38 |
5-Flucylosine stopped Fluconazole 800 mg only for next 2 weeks |
| Day 47 | Enhanced lesions in brain improved |
| Day 52 | Fluconazole 400 mg for long-term |
The patient's vital sign and physical examination were unremarkable. A blood sample was sent to the laboratory, which revealed a white blood cell (WBC) count of 8.37 × 10 ^ 99/L. However, C-reactive protein (CRP) and procalcitonin (PCT) levels were elevated, measuring 139.03 mg/L and 2.98 ng/mL, respectively. He was subsequently treated empirically with piperacillin-tazobactam for 5 days, during which no blood culture was performed, leading to symptom alleviation. However, shortly after discharge, his fever recurred, with a peak temperature of 38.6°C. One month prior, he was readmitted to the local hospital. Upon readmission, a blood culture identified C. lusitaniae and a chest CT showed mild bronchitis in both lungs and postoperative changes in the sternum. Additionally, a positron emission tomography-computed tomography (PET-CT) scan revealed multiple abnormally high metabolic foci adjacent to the ascending aortic canal wall and behind the sternum, with no other areas showing significant uptake. Caspofungin was administered with a loading dose of 70 mg, followed by 50 mg daily. However, after eight days of caspofungin treatment, the patient experienced a recurrence of high fever with chills. On the same night, he developed weakness, difficulty grasping, and a loss of fine motor skills in his left hand. Subsequent brain magnetic resonance imaging (MRI) revealed findings consistent with infarctions or hemorrhages in the right cerebellum as well as in the right frontal, parietal, and occipital lobes (see Figure 1). Subsequently, the patient was transferred to our institution for further management.
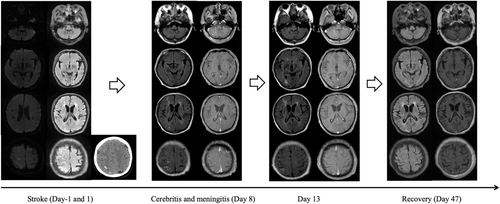
3 Methods
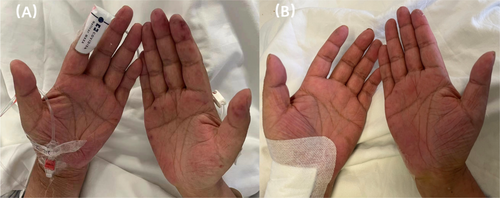
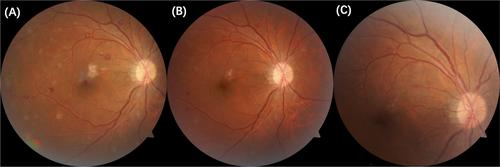
On the day of admission, the patient's vital signs revealed a temperature of 37.9°C, a pulse rate of 65 beats per minute, a respiratory rate of 15 breaths per minute, and a blood pressure of 130/54 mmHg. Physical examination indicated delirium with a normal pupillary light reflex and Janeway lesions scattered across his right hand (Figure 2). Laboratory results showed a WBC count of 6.07 × 109/L (3.5–9.5 × 109/L), with neutrophils comprising 80.8% (40%–75%) and lymphocytes 11.3% (20%–50%). The procalcitonin (PCT) level was 1.55 ng/mL (< 0.1 ng/mL), interleukin-6 (IL-6) was 15.06 pg/mL (< 7.0 pg/mL), and serum 1,3-beta-D-glucan (BDG) was 273.2 pg/mL (70–95 pg/mL). Repeated blood cultures again identified C. lusitaniae, which was sensitive to fluconazole, 5-FC, voriconazole, and caspofungin, but resistant to amphotericin B. Caspofungin treatment was continued while further evidence of infection was sought. By reviewing the patient's prior surgical records, we identified ICU admission post-surgery, during which C. lusitaniae was cultured from his blood. Following antifungal treatment, his symptoms improved, but he was discharged without subsequent long-term antifungal therapy. Given the high suspicion of infection in the artificial vascular graft and the need for screening of other organs, the patient underwent aortic computed tomography angiography (CTA) of the aorta and a whole-body CT scan on the second day of admission. These exams revealed a small filling defect in the inner wall of the proximal brachiocephalic trunk and confirmed the hemorrhage in the right parietal lobe (Figure 1). We performed a transesophageal echocardiogram (TEE), which ruled out endocarditis. Due to the unremovability of the artificial vascular graft and the poor tissue penetration of caspofungin, fluconazole was added with a loading dose of 800 mg, followed by 400 mg daily. On the fifth day of admission, a fundus examination revealed tortuous and dilated retinal veins, multiple exudates, hemorrhages around the macula and fundus, and a Roth spot, all of which strongly indicated Candida endophthalmitis (see Figure 3A). Consequently, intravitreal injections of voriconazole were administered at a dose of 0.1 mg/0.1 mL on the eighth day of hospitalization. However, on the same day, the patient experienced a generalized convulsion, followed by transient unconsciousness. An MRI scan and lumbar puncture were promptly performed to determine the underlying cause. The MRI showed multiple small dot-like, patchy, or linear ring-enhanced lesions in the right frontal, parietal, and occipital lobes. The larger lesions exhibited long T1 and long T2 signals, with high signals on diffusion-weighted imaging (DWI), all highly suggestive of meningitis (see Figure 1). Cerebrospinal fluid (CSF) analysis revealed elevated WBC count, increased immunoglobulin levels, and raised lactate levels. Although no pathogen was detected in conventional cultures, polymerase chain reaction (PCR) assays identified the presence of C. lusitaniae. Based on these findings, the fluconazole dose was adjusted to 800 mg daily, and caspofungin was replaced with 5-FC at a dose of 2.5 g every eight hours on the tenth day of admission, forming the final antifungal regimen. During the course of treatment, both the body temperature and serum 1,3-BDG levels gradually decreased. The patient's blood cultures were negative for fungi on the twelfth day of admission. Additionally, the brain and ocular lesions showed improvement on the thirteenth and fourteenth day of admission (see Figures 1 and 3B). The patient was discharged on the sixteenth day of admission.
4 Conclusions and Results
During follow-up, the lesions in the patient's right fundus had completely resolved (Figure 3C). The patient was treated with a combination of fluconazole (800 mg daily) and 5-FC (2.5 g every eight hours) for 28 days, followed by fluconazole monotherapy at 800 mg daily for an additional 14 days. A follow-up brain MRI performed on day 47 showed substantial improvement. Given the inability to surgically remove the artificial implants, long-term fluconazole therapy at a daily dose of 400 mg is recommended. At the two-year follow-up, the patient remained afebrile, and the condition was well controlled. Invasive candidiasis associated with implants requires tailored anti-infective regimens at various stages of infection, with careful consideration of the tissue penetration of the drugs. If surgical removal of the implant is not feasible, long-term pharmacological therapy may be indicated.
5 Discussion
C. lusitaniae is an uncommon pathogen in clinical practice, accounting for approximately 0.2% to 19.3% of candidemia cases in susceptible populations [6]. Invasive C. lusitaniae infections are rare in patients with normal immune function [6]. Previous studies have shown that C. lusitaniae is prone to infect the peritoneum, central nervous system, and urinary tract [7]. Before the widespread use of fluconazole, the mortality rate due to C. lusitaniae infection ranged from 53.9% to 78%, with most strains demonstrating resistance to amphotericin B [4]. However, with the introduction of fluconazole, the mortality rate dropped to 5% [7]. C. lusitaniae infections can now be effectively treated with 5-FC, azoles, and echinocandins.
Although nearly half of Candida infections occur without identifiable predisposing conditions, immunosuppressed patients are more vulnerable to C. lusitaniae infection [7]. In the case we present, the patient was immunocompetent. However, increased uptake around the aorta was observed on PET-CT. The artificial aorta may have been the source of the infection, resulting in severe candidemia. In addition to CNS involvement, the patient exhibited vascular damage, as evidenced by Janeway lesions on the right hand and Roth spots in the right eye—findings that highlight the vascular invasiveness of C. lusitaniae.
Most central nervous system (CNS) Candida infections are associated with disseminated candidiasis and typically occur in immunosuppressed patients or those undergoing neurosurgical procedures [8]. The prognosis is generally poor, with mortality rates approaching 90% [9]. The clinical manifestations of CNS Candida infection typically depend on the location of the lesion in the brain, potentially resulting in personality changes, seizures, paralysis, and other symptoms. The most common manifestations of CNS Candida infection are meningitis or meningoencephalitis [9]. However, brain abscess, hydrocephalus, and strokes can also occur [10, 11]. In our case, despite the patient's competent immune system, the artificial implant was a significant risk factor for developing serious CNS C. lusitaniae infection, which presented as cerebritis along with sequential ischemic and hemorrhagic strokes [12, 13]. Interestingly, all lesions were confined to the right hemisphere, likely due to an embolus observed in the inner wall of the proximal brachiocephalic trunk. Although the composition of the embolus could not be confirmed, we infer that it was highly associated with C. lusitaniae and responsible for the brain lesions. Fungal invasion of blood vessels can lead to thrombosis and infarction, thereby causing small-vessel vasculitis, cerebral vasculitis, or endocarditis [14]. Candida can activate the alternate complement pathway via its polysaccharides, leading to the inflammatory reaction characteristic of vasculitis [15]. Nicolini et al. [16] reported an ascending aortic graft thrombosis caused by C. albicans infection. As for C. lusitaniae, Sarma et al. [17] observed a hemorrhagic CSF in patients with C. lusitaniae meningitis. Libertin et al. [18] also described an invasive C. lusitaniae-associated vasculitis that resulted in pulmonary and cerebral infarctions, as well as anterior spinal artery embolism. Additionally, the proximity of stroke and cerebritis lesions suggests that the same factors causing the stroke also led to the infection. This evidence, along with the sequence of clinical manifestations, reflects the progressively invasive nature of the infection. Initially, a fungal embolus may have caused infarction and vascular damage, followed by C. lusitaniae breaching the blood–brain barrier and causing cerebritis.
Different Candida species can present similar CNS infection patterns on MRI scans, with meningitis appearing as leptomeningeal, ring-shaped, or nodular enhancements. If vascular involvement occurs, intracranial hemorrhage or infarction may be observed. While CSF culture is critical for diagnosis, its low sensitivity limits its utility. A negative CSF culture does not exclude CNS Candida infection; thus, a comprehensive diagnostic approach is necessary. Elevated protein levels, decreased glucose, and high neutrophilic or lymphocytic counts in the CSF can provide preliminary evidence of infection [8]. PCR assays and next-generation sequencing (NGS) can also be utilized on CSF samples due to their ability to detect low pathogen burdens. However, NGS results should be interpreted with caution due to a relatively high false-positive rate. Regarding treatment, although echinocandins are first-line agents for candidemia, their tissue penetration, including the eye and brain, is poor compared to 5-FC [19]. Fluconazole, which exhibits good penetration in most organs, is recommended for CNS Candida infection [8].
C. lusitaniae candidemia has been reported to have a 2.2%–16% risk of developing endophthalmitis [20], as was observed in our case. Therefore, it is recommended that all patients with candidemia undergo an eye examination [19]. The diagnosis of Candida endophthalmitis should rely on eye examination findings rather than culture, as 20%–30% of cases may have negative cultures [20]. It remains unclear whether different Candida species cause unique manifestations of endophthalmitis; however, a white chorioretinal exudate lesion is a typical finding in fungal endophthalmitis [21]. Sight-threatening lesions near the macula or those involving vitreous invasion typically require intravitreal injection of antifungal agents, such as amphotericin B deoxycholate or voriconazole, with or without vitrectomy, alongside systemic antifungal therapy [22]. Ultimately, our patient achieved full recovery after receiving voriconazole intravitreal injections.
C. lusitaniae exhibits resistance to amphotericin B, though it generally remains susceptible to flucytosine and azoles [3]. While this susceptibility pattern is typical, several studies have documented the emergence of resistance to both flucytosine and azoles in some strains [23], making C. lusitaniae challenging to treat. Echinocandins, which target the β-1,3-D-glucan synthase encoded by the FKS genes, are commonly used to manage C. lusitaniae-associated candidemia. However, resistance to echinocandins has also been reported in multiple strains [24]. In this case, given the inherent resistance of C. lusitaniae and the inability to remove the vascular implant, we utilized a combination therapy approach, initially with caspofungin and fluconazole, followed by fluconazole and flucytosine.
In conclusion, C. lusitaniae candidemia can exhibit high invasiveness, even in immunocompetent individuals. CNS and ocular involvement should be carefully considered, particularly in patients with candidemia. Invasive candidiasis related to implants necessitates stage-specific anti-infective regimens. While echinocandins are recommended for uncomplicated candidemia, disseminated infections require antifungal medications with strong tissue penetration to be used in combination. When surgical removal of the implant is not possible, long-term antifungal therapy is recommended.
Author Contributions
Yi Cui: writing – original draft, writing – review and editing. Zhenxing Huang: writing – original draft, writing – review and editing. Hui Han: writing – review and editing. Yang Ma: writing – review and editing. Shanshan Li: data curation, writing – review and editing. Yuanyuan Hu: data curation, writing – review and editing. Hui Zhang: data curation, writing – review and editing. Xuehai Zhang: data curation, writing – review and editing. Xiuhe Zhao: writing – review and editing. Dexin Yu: writing – review and editing. Jianqiao Li: writing – review and editing. Han Liu: writing – review and editing. Chen Li: writing – review and editing. Hao Wang: writing – review and editing.
Acknowledgments
The authors would like to acknowledge the patient and the multidisciplinary care team that have contributed to his care.
Ethics Statement
The authors have nothing to report.
Consent
Written informed consent was obtained from the patient for the publication of this case report and accompanying images.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.