Unexpected Severe Tracheal Papilloma During Induction
Funding: This work was supported by Scientific Research Fund of Hunan Provincial Education Department, 22A0011. Natural Science Foundation of Hunan Province, 2025JJ60724. Health Research Project of Hunan Provincial Health Commission, W20243113. National Natural Science Foundation of China, 82103641, and 82071348.
Yanling Zhang and Shuiting Zhang contributed equally to this paper.
ABSTRACT
Tracheal papilloma (TP) is an intricate disorder that poses challenges in the diagnosis, therapy, and management of airways due to its association with human papillomavirus infection. In this case report, we present a patient with an unexpectedly large tracheal papilloma detected during induction of anesthesia. The patient successfully underwent surgical resection of the tracheal papilloma. Postoperatively, the patient recovered well, with no recurrence of airway obstruction symptoms during the follow-up period. Preoperative airway assessment was crucial in this case, enabling anticipation of potential airway difficulties, formulation of appropriate anesthetic and surgical plans, and ensuring the patient's safety during the perioperative period.
Summary
- Tracheal papilloma is a complex disorder that poses challenges in the diagnosis, treatment, and airway management due to its association with human papillomavirus (HPV) infection.
1 Introduction
Tracheal papilloma (TP), a benign disorder characterized by papillomatous growth of the bronchial epithelium involving the trachea, has an ambiguous clinical manifestation that can range from minor symptoms like cough to life-threatening problems like upper airway obstruction. Encountering a severe tracheal papilloma during anesthetic induction is extremely risky. The present study describes the coping strategies for an unexpected large tracheal papilloma.
2 Case History/Examination
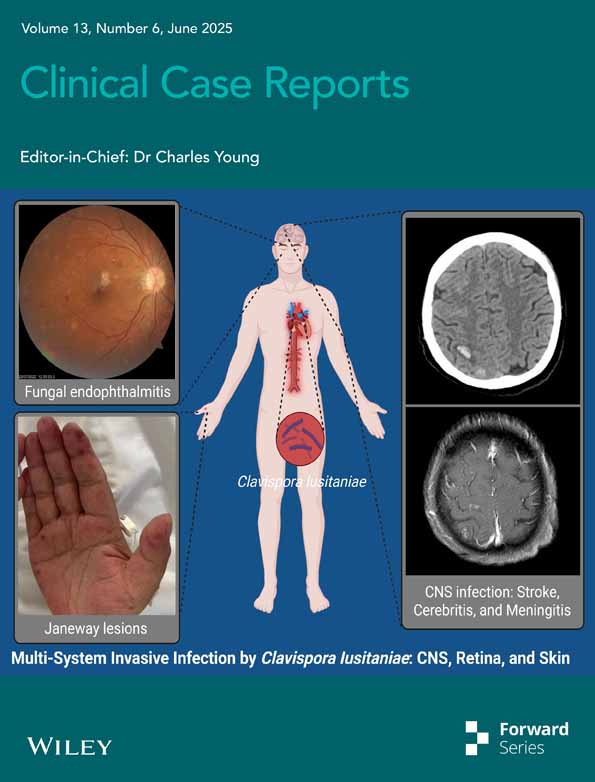
A 37-year-old male patient with vocal cord papilloma was referred to the Otorhinolaryngology Department for surgery. The patient, who had a 1-month history of mild dyspnea and no known comorbidities, had undergone surgical removal of a vocal cord papilloma 2 months ago. Laryngoscopy (Figure 1A,B) and neck computed tomography (Figure 1C,D) revealed several laryngeal lesions but no tracheal lesions.
3 Methods (Differential Diagnosis, Investigations and Treatment)
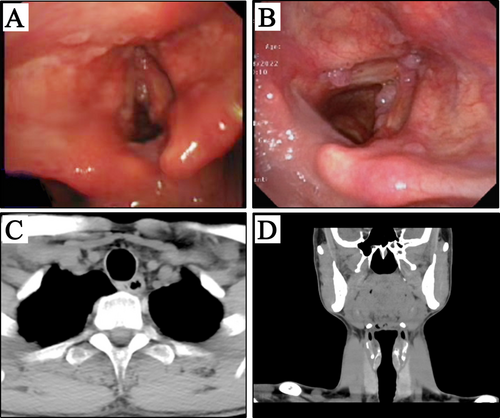
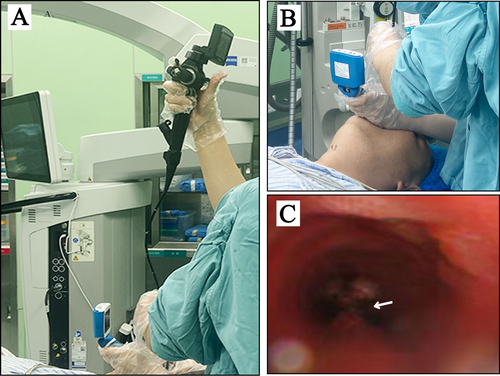
Given the patient's medical history and the characteristics of the papilloma, the anesthetist, after administering adequate local anesthesia, combined video laryngoscopy with fiberoptic bronchoscopy (Figure 2A,B) to assess the airway. This assessment revealed significant polypoidal lesions below the vocal cords and 5 cm from the bulge that almost completely obstructed the trachea (Figure 2C). Subsequently, tracheoscopy (Figure 3A,B) and chest computed tomography (Figure 3C–F) indicated a severe obstruction caused by a single cauliflower-like mass. A presumptive diagnosis of tracheal papilloma was made. Considering the presence of polypoidal lesions and the patient's history of papilloma, we initially entertained other possibilities such as tracheal carcinoma, tracheal granuloma, and foreign body in the trachea. Tracheal carcinoma was ruled out due to the absence of typical malignant features such as an invasive growth pattern on imaging (CT scans did not show infiltration into adjacent tissues). Tracheal granulomas usually exhibit different morphological characteristics, often associated with signs of inflammation, which were not evident in our patient's case. Foreign body in the trachea was excluded as there was no history of foreign body ingestion.
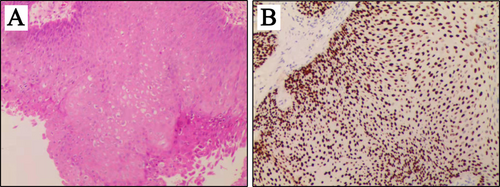
Regarding the management, upon the diagnosis of the tracheal papilloma, the initial procedure of the patient was terminated to allow for further assessment and planning. The patient then underwent bronchoscopic surgery using flexible bronchoscopes to remove the papillomatous lesions. The flexible bronchoscope, equipped with advanced imaging and biopsy capabilities, facilitated precise visualization and removal of the papillomatous lesions. Regarding anesthesia, general anesthesia was induced with Propofol and Sufentanil and maintained with Remimazolam. Throughout the procedure, the patient's vital signs, including heart rate, blood pressure, and oxygen saturation, were continuously monitored to ensure a safe and stable surgical environment. Postoperatively, the patient was transferred to the intensive care unit for close monitoring of respiratory function. Oxygen supplementation was provided as needed, and the patient's airway was closely observed for any signs of edema or obstruction. Histologic examination of the postoperative specimen showed mild-to-moderate-grade atypia dysplasia with squamous papilloma (Figure 4A,B). The patient declined further testing for human papillomavirus (HPV).
4 Conclusion and Results (Outcome and Follow-Up)
The tumor was successfully removed via bronchoscopic excision. Pathological examination of the postoperative specimens confirmed squamous cell papilloma (Figure 4A,B). The patient declined further HPV testing. During the one-week follow-up period, the patient reported improved breathing and minimal discomfort.
5 Discussion
Tracheal papilloma is the tracheal manifestation of recurrent respiratory papilloma, which has been observed in all ethnic groups and affects both male and female patients. HPV infection is the primary cause of TP [1, 2]. However, an individual's immunological response is also of great significance [3]. Sometimes papilloma develops and recurs because a compromised immune system is unable to adequately eradicate the virus. Furthermore, because of its nonspecific clinical presentation, the diagnosis may be overlooked in clinical practice, which could result in the disease developing further [4]. Therefore, intubation difficulties during elective or emergency surgery may be unexpectedly caused by TP. This case described the strategies for coping used by the anesthesiologist in response to a male patient's large, unidentified, isolated papilloma in the major bronchus combined with a vocal cord papilloma.
The treatment of TP is a long-term process that requires diverse treatment methods. The recommended therapeutic approach is bronchoscopy-assisted surgical excision of the TP [2]. This minimizes harm to the surrounding healthy tissue while enabling the papilloma to be precisely removed with a very thin surgical instrument. Even after surgical removal, there is a chance of recurrence, and eventually, additional surgeries can be required. Interferon alpha has been used as an adjuvant treatment, as it is believed to have antiviral and immunomodulatory effects [5]. Research on immunotherapy for TP is still ongoing [6]. The possibility of HPV-targeting vaccinations to prevent papilloma from returning in infected individuals is being investigated. More crucial than treatment, it is essential that patients undergo routine endoscopic exams, such as tracheoscopy or laryngoscopy, following treatment [7]. This is done to find any early indications of recurrence. In our case, the patient did not receive routine throat examinations and did not take the early signs of breathing difficulties seriously. Consequently, a massive papilloma developed in the trachea.
Additionally, because of the possibility of airway blockage and other related issues, tracheal large papilloma might pose serious difficulties during anesthesia. A thorough evaluation of the perioperative airway is essential [8, 9]. To determine the exact location and size of the papilloma, a comprehensive airway evaluation may initially entail a review of imaging modalities, such as computed tomography (CT) scans and ultrasound [10, 11]. Enhanced interdisciplinary communication, particularly among anesthesiologists, surgeons, and radiologists, can ensure a thorough understanding of the patient's condition prior to induction. Second, maintaining spontaneous breathing may be preferable [12]. This is crucial because it helps avoid positive pressure ventilation, which can lead the papilloma to further constrict the airway. Third, keep all the equipment needed for difficult airways close to hand, including tracheostomy kits, fiber optic bronchoscopes, and various sized laryngeal mask airways. Regular training on emergency airway procedures is also crucial. Furthermore, prompt action can be necessary if there is an unexpected airway compromise during induction [13]. Extubation should be performed only when the patient is fully awake and has regained protective airway reflexes. To make sure that the airway stays open following tracheal extubation, it could occasionally be required to do an extubation trial while keeping a fiber optic bronchoscope on standby [14].
6 Conclusions
In summary, TP is a disease that is complex to treat and has a high recurrence rate. Patients with laryngeal papilloma should be monitored for undetected tracheal papillomas. Preoperative airway assessment is crucial for future cases, enabling anticipation of potential airway difficulties, formulation of appropriate anesthetic and surgical plans, and ensuring the patient's safety during the perioperative period.
Author Contributions
Yanling Zhang: conceptualization, data curation, resources, writing – original draft. Xin Li: data curation, investigation, visualization. Ting Tan: investigation, validation. Shuiting Zhang: conceptualization, data curation, funding acquisition, supervision, writing – review and editing.
Acknowledgments
This study was supported by the National Natural Science Foundation of China (82103641), the Key Fund Project of Hunan Provincial Department of Education (22A0011), the Natural Science Foundation of Hunan Province (2025JJ60724), and the Health Research Project of Hunan Provincial Health Commission (W20243113).
Consent
The patient provided written informed consent to publish this report, in line with the journal's patient consent policy.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
All data underlying the results are available as part of the article and no additional source data are required.