A Modified Tracheostomy Technique in an Adult Patient With Klippel–Feil Syndrome
Funding: This work was supported by the Sherrold Haddad Award, Surrey Hospitals Foundation.
ABSTRACT
Placing a tracheostomy is challenging in patients with Klippel–Feil syndrome due to a short, flexed, and immobile neck that can limit surgical access to the trachea. Here, we report a modified technique with elements from both open and percutaneous tracheostomy without requiring sternotomy.
1 Introduction
Klippel–Feil syndrome is a rare congenital condition affecting approximately 1 in 40,000–42,000 births globally [1]. It is characterized by the abnormal fusion of the cervical vertebrae, most commonly, the C2–C3 and C5–C6 levels [1]. This fusion results in a shortened cervical spine, often accompanied by other skeletal and craniofacial anomalies [1]. Up to half of pediatric patients with Klippel–Feil syndrome may be asymptomatic, while symptoms related to the cervical spine are more prominent in adulthood [1]. Thus, patients with Klippel–Feil syndrome show considerable anatomic and clinical variation, with less than half displaying the classic triad of a short neck, low posterior hairline, and limited neck mobility, which can pose distinct challenges for airway management due to limited surgical access to the trachea [1].
In this report, we present the first published case of a tracheostomy in an adult patient with retrosternal trachea due to Klippel–Feil syndrome. This case highlights how a modified technique with elements from both open and percutaneous tracheostomy can be successfully used to secure a surgical airway in patients with challenging tracheal anatomy.
2 Case History and Examination
A 38-year-old male presented to our hospital with sepsis, necessitating emergent fiberoptic intubation. The patient's past medical history was significant for Wildervank syndrome with Klippel–Feil anomaly characterized by a small jaw, a non-existent neck, and a fused cervical spine. He was an active smoker, and the respirology service suspected previously undiagnosed obesity hypoventilation syndrome. As a result, he was referred to the otolaryngology service for consideration of a tracheostomy for prolonged mechanical ventilation.
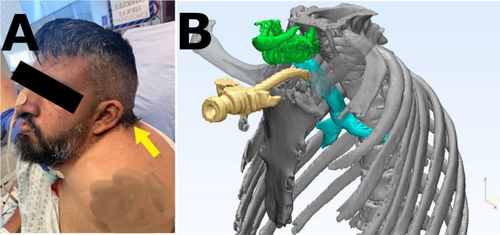
On physical examination, the patient's neck was found to be in a flexed position without any extension on maximum effort, and there was a 5 cm gap between the sternum and the retrognathic jaw. Furthermore, no palpable landmarks such as thyroid or cricoid cartilages were identified in the neck, suggesting a retrosternal larynx (Figure 1).

3 Methods (Differential Diagnosis, Investigations, and Treatment)
A computed tomography (CT) scan confirmed cervical spine fusion and a retrosternal cricoid cartilage. Given these findings, a challenging surgical procedure was anticipated. Informed consent was obtained from the patient's family to attempt an open tracheostomy, with the potential need for percutaneous assistance or sternotomy.
Surgical technique: The patient was brought to the operating room and positioned supine. The neck remained in a neutral position as it could not accommodate a shoulder roll, given the cervical spine fusion. A 4 cm horizontal incision was made above the sternum, a superior and inferior subplatysmal flap was raised, and the strap muscles were retracted laterally. The thyroid cartilage was identified at the sternal notch, while the cricoid cartilage was fully retrosternal. Despite the use of a cricoid hook and superior traction, the trachea could not be visualized in the neck.
Given the inability to visualize the trachea directly, a modified percutaneous tracheostomy was performed. With the cricoid hook on full superior traction, a finger was used to feel the cricoid and the tracheal rings retrosternally and gently guide the percutaneous needle through the trachea by palpation just inferior to the cricoid cartilage. Placement of the needle into the tracheal lumen was confirmed with a flexible bronchoscope.
Using the Seldinger technique, a guidewire was placed through the needle into the trachea that was then dilated with a Blue Rhino Percutaneous Tracheostomy Introducer Set (Cook Critical Care, Bloomington, IN, USA). A Shiley #7 cuffed extended-length tracheostomy tube was inserted over the guidewire and secured (Figure 2). Placement was confirmed by end-tidal CO2 detection. The wound was closed, and the patient was transferred to a high-acuity unit.
4 Discussion
To the best of our knowledge, this case represents the first published report of a tracheostomy in an adult patient with Klippel–Feil syndrome. It further emphasizes the importance for otolaryngologists to become familiar with features of Klippel–Feil anomaly, as similar challenging neck anomalies may be encountered in patients with other conditions, such as fetal alcohol syndrome and Goldenhar syndrome [1].
Percutaneous tracheostomy, generally the preferred modality for managing patients requiring prolonged mechanical ventilation, is contraindicated in patients demonstrating the classical symptom triad of Klippel–Feil syndrome [2]. The procedure relies on adequate neck extension and anatomical access to midline structures, which can be compromised due to cervical vertebral fusion and retrosternal tracheal position. These limitations can make percutaneous access technically challenging and potentially unsafe when used alone, particularly when key landmarks are not palpable.
Although open tracheostomy is often preferred for managing patients with complicated airway anatomy, it can be challenging to perform an open tracheostomy in patients with Klippel–Feil syndrome due to the positioning of the trachea behind the manubrium sterni [3]. Such cases will require a sternotomy to access the trachea, but the procedure is deemed high risk and is either not clinically justifiable, and in the rare case when it is, the patient's family may refuse to provide consent as demonstrated by Lakshminarasimhaiah et al. [4]. Both tracheostomy and sternotomy can independently contribute to the risk of hemodynamic instability, infections, and delayed postoperative recovery due to the invasive nature of these techniques [5, 6]. In cases of acute airway obstruction when intubation is deemed unsafe, tracheostomy under local anesthesia is not preferred in adult patients with symptomatic Klippel–Feil syndrome, especially if accompanied by an elevated risk of tracheal compression due to an anomalous innominate artery that tends to be progressively rightward of the trachea with age, and the difficulty in getting or maintaining cooperation in patients with underlying anxiety or communication difficulties [7-10].
In our case, the inability to safely proceed with either technique alone led us to adopt a hybrid approach. The utility of combining open and percutaneous approaches to the tracheostomy was previously highlighted by Biderman et al. [11], who reported on successfully performing tracheostomies in 20 patients with difficult neck anatomy. The causes of difficult neck anatomy included hyper-flexion or impossible neck extension due to musculoskeletal deformation and hallow/C-spine fixation after a neck injury, morbid obesity, and goiter. Of note, none of the 20 patients had Klippel–Feil syndrome. While our patient's pathology was congenital rather than acquired, the principles guiding the use of a hybrid approach remained consistent.
Combining open and percutaneous tracheostomy techniques, as Biderman et al. [11] described, allowed us to perform a tracheostomy without direct visualization of the trachea. Importantly, sternotomy was avoided, which would have carried the risks of infection, prolonged recovery, and chronic pain. The modified tracheostomy technique described in this report would be contraindicated if preoperative imaging demonstrated a high-riding innominate artery or brachiocephalic vein, as placing a tracheostomy retrosternally in such cases could lead to a catastrophic hemorrhage.
This approach may also be adaptable to patients with other congenital craniofacial syndromes, such as Goldenhar syndrome and fetal alcohol syndrome (FAS). In Goldenhar syndrome, cervical vertebral fusion and mandibular hypoplasia can limit surgical exposure to the anterior trachea [12], while FAS has been associated with Klippel–Feil-like fusion anomalies in over half of affected patients, further contributing to difficult airway access [13]. Familiarity with such anatomical variations and the potential role of hybrid tracheostomy may assist surgeons in avoiding unnecessary sternotomy while maintaining airway safety.
5 Conclusion and Results (Outcome and Follow-Up)
Adult patients with congenital neck anomalies present a unique tracheostomy challenge. In some situations, neither open nor percutaneous approaches might be sufficient when attempted in isolation. To the best of our knowledge, this is the first case in the literature of an adult patient with Klippel–Feil syndrome managed successfully with a combination of open and percutaneous tracheostomy techniques. This technique might be of benefit to surgeons considering performing tracheostomies on adult patients with congenital anomalies.
The patient had an uneventful recovery. The tracheostomy was changed to a cuffless tube at the bedside, and he was discharged home with the tracheostomy in place. At the 8-month follow-up, the patient remained tracheostomy-dependent due to obesity hypoventilation syndrome but had no complications related to the procedure.
Author Contributions
Arshbir Aulakh: visualization, writing – original draft, writing – review and editing. Oleksandr Butskiy: conceptualization, project administration, resources, supervision, validation, visualization. Amir Parham Pirhadi Rad: software, visualization. Mohammad Nourizadeh: writing – original draft, writing – review and editing.
Acknowledgments
We would like to thank the Surrey Hospitals Foundation for their generous support, specifically through the Sherrold Haddad Excellence in Medicine Award Program.
Consent
Written informed consent was obtained from the patient to publish this case report, including images, in accordance with the journal's patient consent policy.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
All data presented in this case report that can be anonymized is available from the corresponding author upon reasonable request.