Bilateral Total Hip Arthroplasty for Osteofibrous Dysplasia Assisted by CT-Guided 3D Printing: A Case Report
Funding: This work was supported by grants from the Medical Science and Technology Project of Zhejiang Province (No. 2024KY1794) and Taizhou Social Development Science and Technology Plan Project (No. 23ywa08).
ABSTRACT
Osteofibrous dysplasia with obvious deformities, persistent pain, functional problems, or pathological fractures usually requires surgical intervention. This report highlights that computed tomography-based 3D printing preoperative planning can facilitate precise intraoperative positioning of the osteotomy plane and prosthesis stem design for complex bone deformities.
1 Introduction
Osteofibrous dysplasia (OFD) is a benign and deformity-inducing fibro-osseous disease, comprising approximately 0.2% of all primary bone tumors. OFD usually occurs in children under 20 years old, more often in boys than in girls, and often affects unilateral intracortical tibia [1]. OFD can present without symptoms or with pain, swelling, mass, deformity, and even pathological fracture [2]. X-ray shows eccentric lytic with cortical expansion and intramedullary extension that could lead to bowing deformity and even pathological fracture. MRI presents a bubbly appearance with well-circumscribed sclerotic edges [3, 4]. The main treatment approach for patients with mild symptoms or asymptomatic OFD is conservative treatment [5], while OFD patients with obvious deformities, persistent pain, functional problems, or pathological fracture usually require surgical intervention [6].
Surgical planning in two dimensions presents inherent limitations for patients with multifaceted deformities and fractures, including torsional and mixed angle deformities across various planes [7]. An advantage of three-dimensional (3D) surgical planning is that it allows for comprehensive assessment of deformity correction across multiple planes at the same time, which ensures greater precision and efficiency during surgery [8]. 3D surgical planning has been widely used in complex orthopedic surgeries, such as periprosthetic femoral fractures [9] and orthopedic osteotomy [10]. We reported this case of severe bilateral femoral deformity and femoral neck fracture, which adopted the 3D corrective osteotomy planning to perform total hip arthroplasty (THA), corrective osteotomy, and femoral isthmus plasty (reduce the diameter of the medullary cavity inwards). This case showed 3D printing-assisted THA for OFD achieved satisfactory clinical and radiological outcomes.
2 Case History/Examination
A 39-year-old male was hospitalized with chief complaints of bilateral hip pain and limited mobility for over 30 years. He suffered from a left femoral neck fracture at eight and was treated with cast immobilization. Since then, he had a claudication symptom. When he was 10 and 27 years old, he had left femur fractures, both of which were treated conservatively. Since last week, the patient's pain in the right hip was worsened and painkillers cannot relieve the pain. The patient is unable to weight bear and perform daily activities. No similar patients existed in his relatives.
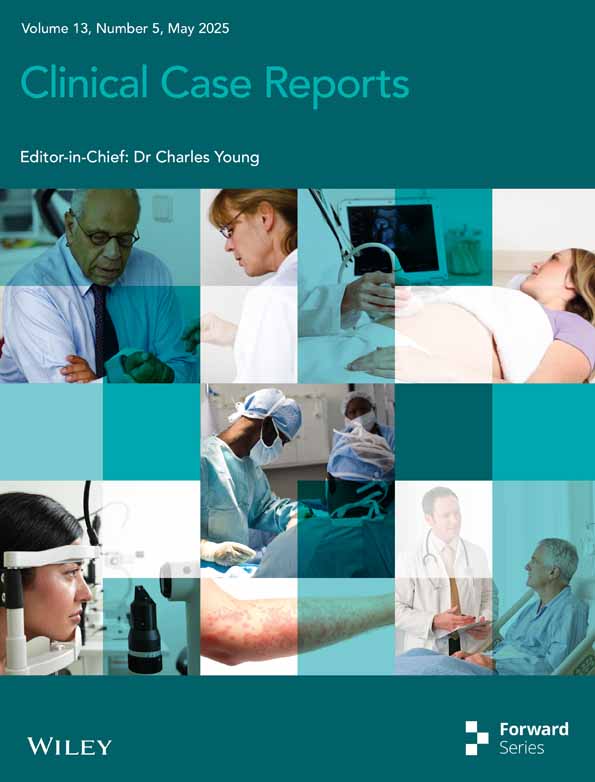
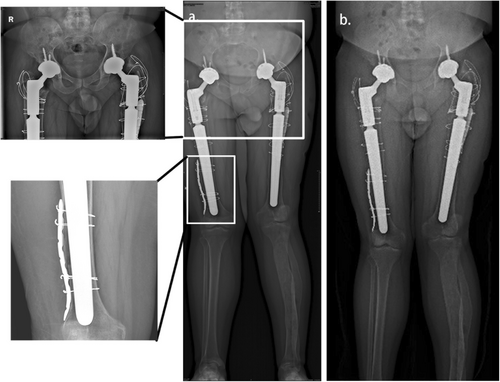
Upon examination, there were scars on the left lateral thigh. The right lower limb was about 3 cm shorter than the left lower limb based on the alignment view (Figure 1a). No increase in local heat was detected when both femurs were palpated. He had limited bilateral hip joint movement and tenderness in both inguinal regions. The sensation in the extremities was intact, and the blood supply was normal following distal neurovascular assessment.
3 Methods (Differential Diagnosis, Investigations, and Treatment)
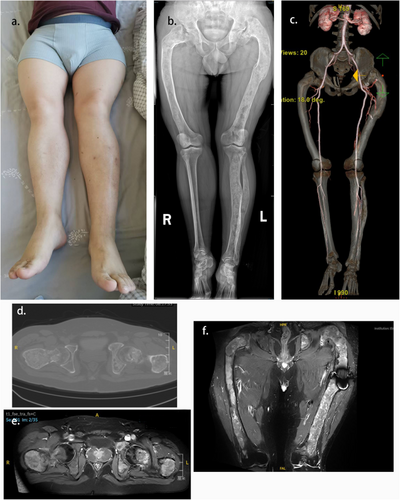
X-ray and CT scan showed the typical “ground-glass” appearance, bilateral proximal femoral shepherd's crook deformity, bilateral femoral neck fractures and old fractures of the left femur (Figure 1b,d). Enhanced MR Imaging showed large areas of low signal on T1WI and high signal on T2WI + FS. The edge of the lesion was blurred. The lesion was dominated by changes in the bilateral femur, and the enhancement was obviously uneven after enhancement (Figure 1e,f). CT angiography (CTA) showed the distribution of large blood vessels in both lower extremities (Figure 1c). On bone scan imaging, increased uptake was observed in the bilateral femur, acetabulum along with left tibia and fibula. No abnormal absorption was detected in other bones in the body (Figure 2). The patient was diagnosed with OFD.
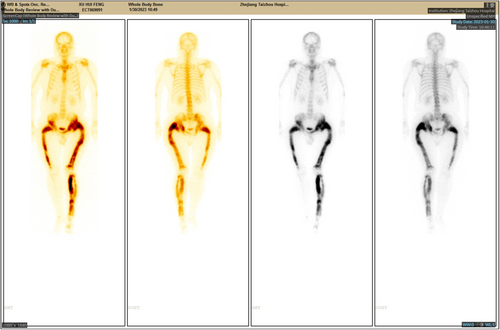
The chosen surgical approach entailed right THA, femoral osteotomy, and isthmus plasty. In view of the complexity of the operation, a preoperative simulation of osteotomy and implantation of the prosthesis stem was carefully designed according to the 3D reconstructive bone model, and large blood vessels were avoided according to the CTA results. To begin with, 3D computer models of the femoral bones of this patient were created based on the data obtained from the 3D-CT scan (GE Additive Arcam Spectra H). The mechanical alignment of the femur and osteotomy requirements, including angle and position, could be simulated on a 3D reconstruction model. The femoral morphology and mechanical alignment could be evaluated again following corrective osteotomy. In order to determine the optimal insertion points and direction of implantation, we simulated the implantation of prosthesis stems and determined their size and diameter, which matched with the medullary cavity (Figure 3). In addition, the 3D osteotomy plan was replicated in vitro.
Using lateral position, a standard surgical approach through hip posterior lateral incision was routinely conducted to expose the acetabulum and proximal femur. The ideal inclination angle for the acetabular cup was 40° ± 10°, and the combined anteversion of the acetabular cup and femoral stem was 37° ± 10°. Firstly, perform femoral neck osteotomy and remove the femoral head. Thoroughly clean the acetabular lesion and fill the acetabulum defect with allogeneic cancellous bone graft before acetabular component placement. Secondly, subtrochanteric osteotomy and middle femoral osteotomy according to preoperative template measurement were followed by curetting all abnormal fibrous tissue from the femoral segment. Thirdly, isthmus plasty was performed by designing a tongue-shaped bone flap at the distal femur and fixing the flap with steel plates and wires to reduce the diameter of the medullary cavity inwards. Fourthly, the 3D-designed prosthesis femoral stem, which was sized prior to surgery, was pressed one time into the intramedullary cavity of the femur. Finally, the femoral shaft and greater trochanter were immobilized using multiple wire cerclages. During intraoperative fluoroscopy, the fixation was confirmed viable. Histological analysis of bone tissue samples was performed after the procedure. Observations of spindle-shaped fibroblasts within the bone stroma, intermixed with irregular bone tissue, confirmed the diagnosis of OFD microscopically.
4 Results
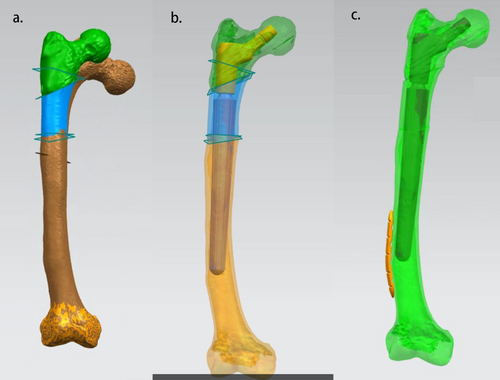
Exercises in active and passive ranges of motion were carried out immediately after surgery, with nonweight-bearing walking permitted over the first 4 weeks after surgery, followed by protected weight-bearing. The patient was ambulating with crutches by 8 weeks after surgery. The patient's lower limbs recovered equal length. Verification demonstrated alignment with preoperative planning postoperatively.
During a 12-month follow-up, the patient's radiological and functional results were satisfactory (Figure 4). The Harris Hip Score (HHS) improved to 86 from 31 preoperatively. The patient was very satisfied with the outcome of the surgery.
5 Discussion
Patients with OFD have severe femoral deformities and poor bone conditions, making the implantation of the prosthesis stem difficult. Reconstructive images in 3D are able to provide an accurate evaluation of patients' bone configurations, femoral deformity sites, affected bone lengths, abnormal mechanical alignments as well as multilevel diameters of the medullary cavity. Surgical procedures and the size of the implanted prosthesis stem can be preoperatively planned. In this case, we used CT-guided 3D printing technology to present a bilateral THA for treating OFD accompanied by severe bilateral femoral deformity and femoral neck pathological fracture using a cementless long stem. Preoperative planning greatly reduced the difficulty of the operation. No early loosening of the prostheses was observed in the first year of follow-up.
In OFD, bone fragility is common. The intramedullary nailing of fractures in the proximal femur, especially subtrochanteric fractures, is a reliable fixation choice because it stabilizes the femur, prevents refractures, and preserves neck shaft angles [11]. Ippolito et al. suggested intramedullary nailing was the best treatment when a child's femur and tibia were totally affected by OFD [12]. 12% of patients with OFD will develop hip osteoarthrtitis and may need THA during their lifetime [13]. Sierra believed that OFD patients could relieve long-term pain and improve hip function after THA [14]. Besides, Garceau et al. treated nine patients with OFD with THA, with an average follow-up time of 6.0 years. The results showed low complication and revision rates [15]. The reasons why we used THA for this OFD patient were: (1) bilateral acetabular lesions; (2) bilateral femoral neck pathological fractures, being at risk of femoral head necrosis; (3) severe femoral deformity requiring osteotomy.
Choosing the prosthesis stem is based upon the primary stability and long-term survival of the patient, especially in cases where the patient has bone deformities or poor bone health. Firstly, the stem we chose was cementless. The compromised bone, marked by an expansive and uneven medullary cavity along with a thin cortex, lacks the strength to adequately support the cement-bone interface [16]. The cement-bone interface during cemented stem implantation is definitely affected by massive intramedullary bleeding [14]. What's more, cement leakage may prevent bone healing and promote bone resorption around the osteotomy site [17]. Secondly, the stem we applied was long. Sierra reported that short uncemented stem fixation for proximal femur OFD patients displayed a high rate of aseptic loosening (60%). He highly recommended a long stem prosthesis for patients with OFD combined with hip joint OA. To reduce the risk of fractures after surgery, he recommended extending the stem by at least two femoral canal diameters above the lesion length [14]. Advances in instrumentation and the use of longer stems to bypass areas of weak cortical bone distally have reduced the risk of stem subsidence and femoral fracture [18]. Thirdly, we used 3D image-based custom stems. Anderson et al. recommended a custom-made stem for complex cases to achieve well-fixed implants and restore hip biomechanics [19]. Custom-made implants had been accepted in femoral revision surgery [20], reverse shoulder arthroplasty [21], THA [19] and developmental dysplasia of the hip [22]. Primary THA using 3D image-based custom stems had promising survival, clinical, and radiographic outcomes [23]. Based on 3D reconstruction model measurements, the predicted sizes of femoral prosthesis are more accurate than the conventional preoperative template. In a word, we chose a custom-made cementless long stem to create precise, stable, and durable fixation.
Besides prosthesis stems, a good press-fit between the bone and the femoral component contributes to the primary stability of the femoral stem in cementless THA models; moreover, long-term stability requires osseointegration of the cancellous bone [24]. Radiological features of OFD include cortical thinning and expansion, intramedullary extension, and deformity. In addition, the femur cavities exhibited irregularities postcurettage. Garceau et al. used a large volume of allograft material in the proximal femur when treating OFD patients with THA. Following a 6-year follow-up period, cementless components and routine use of allograft material showed low complication rates and revision rates [15]. In addition, Yao et al. hold that medullary wall cavities and periacetabular should be grafted with allogeneic cancellous bone to improve prosthesis contact, enhance bone integration, and improve long-term stability with an average duration of 47 months follow-up [25]. In this case, we filled the acetabulum defect with allogeneic cancellous bone graft before acetabular component placement. The femoral isthmus provides stem stability with 2–3 cm of diaphyseal contact [26]. Given intramedullary extension in OFD patients, the femoral isthmus loses its ability to provide distal fixation to the prosthesis. In order to improve the morphological match of the prosthesis with the bone to reduce prosthetic failure, we designed femoral isthmus plasty to reduce the inner diameter of the medullary cavity and increase the stability of the stem in the early stage. The one-year follow-up results showed that the femoral stem was fixed in place without subsidence.
One limitation of this case study was that the follow-up was 1 year. Long-term complications may include implant loosening, loss of deformity correction, or periprosthetic fracture, which need further follow-up.
6 Conclusion
This study emphasized the critical role of preoperative planning in guiding corrective osteotomy and prosthesis stem design, thereby enhancing the accuracy and feasibility of complex surgical procedures. The postoperative results showed that stems were stable and mechanical alignment was precisely restored. Following 1 year of follow-up, radiological and functional results were satisfactory.
Author Contributions
Liwei Ying: data curation, investigation, writing – original draft, writing – review and editing. Yuhang Zhang: writing – original draft, writing – review and editing. Zhong Zhu: data curation, writing – review and editing. Zhongyi Chen: data curation, investigation. Jiajing Ye: conceptualization, data curation, investigation, methodology, supervision, validation.
Ethics Statement
This case study complied with the Helsinki Declaration standards and was approved by the Medical Ethics Committee of Taizhou Hospital Affiliated with Wenzhou Medical University (K20221219).
Consent
A written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.