Delay in Diagnosis of a Rare Case of Microcystic Adnexal Carcinoma in a Middle-Aged Woman
Funding: The authors received no specific funding for this work.
ABSTRACT
MAC is a rare adnexal tumor with nonspecific clinical presentation. Dermatologists should consider the diagnosis of MAC when there is a solitary, longstanding lesion with aberrant clinical behavior supported by typical pathological findings of sweat gland malignant changes.
1 Introduction
Microcystic adnexal carcinoma (MAC) is a rare and highly invasive tumor that arises from the eccrine ducts, with a propensity for local recurrence [1]. MAC primarily affects young to middle-aged individuals, with a higher incidence in women, though it can occasionally occur in children. The lesions typically exhibit a gradual increase in size over several years, often leading to misdiagnosis due to their unusual presentation. Accurate identification of MAC is crucial for appropriate management and treatment. Clinically, MAC often presents as a firm, flesh-colored plaque that progressively enlarges. Notably, variations in the clinical morphology of MAC have been reported. Additionally, it has been observed that MAC tends to have a higher prevalence on the left side of the body [2]. Microscopically, MAC tends to extend beyond the visible margins of the tumor, infiltrating the dermal, subcutaneous, and sometimes perineural tissues. Potential triggers include UV exposure, immunosuppression, and previous radiotherapy. Histologically, MAC is characterized by well-differentiated nests and cords of keratinocytes, displaying both follicular and ductal features within a sclerotic stroma. Treatment options for MAC commonly involve surgical interventions such as excision or Mohs micrographic surgery, which aim to completely remove the tumor while minimizing damage to surrounding healthy tissues [3].
2 Case Presentation/Examination
A 58-year-old woman was referred to Razi Dermatology Hospital with a complaint of a painless, solitary atrophic plaque on her left cheek that was first noticed 12 years ago. The atrophic plaque was asymptomatic and gradually enlarged during the last 12 years. The atrophic plaque became more prominent and indurated in the past 4 months, following weight loss due to lifestyle changes and dietary control. There was no significant past medical history, radiation exposure, or trauma. In addition, she denied cigarette smoking or any drug abuse.
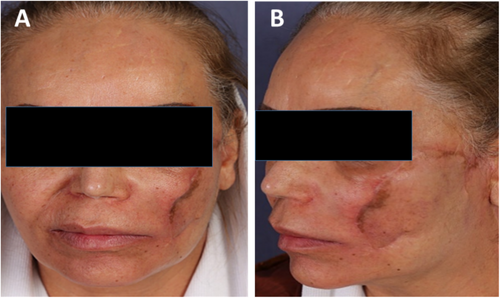
On physical examination, a solitary, skin-red colored atrophic plaque, measuring 1 × 1.5 cm, was observed in the left cheek, which was deeply indurated upon deep palpation (Figure 1A–C). Cervical and axillary lymphadenopathy were not found.

2.1 Differential Diagnosis, Investigations, and Treatment
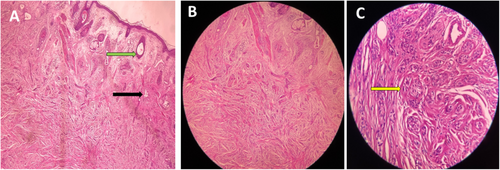
Sonography identified a hypoechoic area with indistinct boundaries and posterior shadowing in the hypodermis of the left buccal zone, measuring approximately 10 × 13 mm. Skin biopsy was performed with the differential diagnosis of morphed, morpheaform basal cell carcinoma, localized lipodystrophy, lupus panniculitis, and adnexal tumors. The skin biopsy revealed poorly circumscribed infiltrations in the dermis. Pseudo-horn cysts with lamellar keratin were identified in the upper dermis. Also, there were numerous small solid nests. Some of these nests displayed ductal lumina while others exhibited tadpole-like features, deeply infiltrated into the dermis with extension to the hypodermis, although deeper nests had a tumoral appearance. The infiltrating nests were surrounded by a dense fibrous stroma, which was transected by the margin edges. Cytologically, mild cytologic atypia and a few mitotic figures were present (Figure 2A–C). These findings were consistent with a diagnosis of MAC. Perineural invasion was also identified in the biopsy specimen. Complementary imaging was done to rule out metastasis and there were no suspicious findings. The patient underwent wide local excision with a 1-cm margin including the entire dermis and subcutaneous fat (Cervicofacial flap) (Figure 3A,B).
2.2 Outcome and Follow Up
Post-operating histology confirmed the previous diagnosis of MAC. Malignant cells were not seen within 8 mm from the tissue edge and 2.6 mm from the deep margin; however, there was a perineural invasion. Post-surgical magnetic resonance imaging (MRI) of the cervical soft tissues and face revealed an enhancing lesion measuring approximately 34 × 17 mm in the left buccal space, superficial to the masseter muscle. This finding suggests the potential presence of residual tumor tissue. According to the patient's MRI findings and the locally aggressive nature of MAC, radiotherapy was initiated to control local disease progression and minimize the risk of recurrence.
3 Discussion
MAC is a rare and locally aggressive neoplasm of eccrine ductal origin, initially described in 1982 with 700 reported cases in the literature [4]. Predominantly affecting young or middle-aged adults, especially in women, Potential triggers include UV exposure, immunosuppression, and previous radiotherapy [1]. MAC typically presents as an indurated, asymptomatic, indolent nodule, papule, plaque, mass, or cystic lesion with a smooth surface and flesh-colored to yellowish hue, commonly located in the head and neck region, often on the left side. Despite variations reported in morphology, MAC tends to grow slowly over several years and may recur locally post-excision but rarely metastasizes [2]. Due to its rarity and atypical presentation, MAC is often misdiagnosed. Differential diagnoses include desmoplastic trichoepithelioma and morpheaform basal cell carcinoma, both of which could be ruled out via histology and immunohistochemistry [5]. Accurate diagnosis is crucial for effective management. Microscopically, MAC is characterized by well-differentiated nests and cords of keratinocytes with follicular and ductal features within a sclerotic stroma. The tumor often extends beyond visible margins, infiltrating dermal, subcutaneous, perineural tissues, and even skeletal muscle [6]. A review of the literature reveals several cases of MAC with varying presentations and outcomes; for example, a 44-year-old man presented with a large MAC that invaded the perichondrium, muscle, nerve, and blood vessel adventitia [7]. Another study reviewed 48 cases, noting that MAC is misdiagnosed 30% of the time, predominantly affects the left side of the face in middle-aged women, and has a recurrence rate of 1.98% per patient/year. The study also highlighted the effectiveness of Mohs micrographic surgery in achieving clear margins [8]. Lei Zhang et al. characterized and compared two rare cases of MAC, one occurring in the tongue and the other in the lip, highlighting the diagnostic challenges and histological features [9]. Treatment options for MAC commonly include surgical interventions such as wide local excision or the Mohs surgery technique. These modalities aim to remove the tumor entirely while minimizing damage to adjacent healthy tissues. The use of radiation therapy as a monotherapy for MAC remains unsatisfying due to the limited evidence and rarity of the disease [10].
Our patient presented with a long-lasting, asymptomatic skin-colored lesion in the left buccal area, persisting for over a decade and initially misdiagnosed as lipodystrophy. The lesion's slow growth and indolent nature challenged the conventional understanding of MAC. In physical examination, it appeared as an atrophic area with induration only detected upon deep palpation. Sonography identified a hypoechoic area with indistinct boundaries and posterior shadowing in the hypodermis of the left buccal zone. MAC was not initially considered in the differential diagnosis, making the pathological confirmation a significant surprise.
The patient underwent wide local excision with a 1-cm margin and Cervicofacial flap reconstruction. Unfortunately, post-surgical MRI revealed residual tumor tissue, prompting adjuvant radiotherapy due to MAC's aggressive nature and perineural invasion. After 36 radiotherapy sessions, no remaining tumor tissue was detected. Post-surgery, the patient experienced significant complications, including facial nerve paralysis and dry mouth due to facial nerve involvement. Despite surgical efforts, these complications have impacted the patient's quality of life and present ongoing management challenges. The facial nerve dysfunction has led to paralysis on the affected side of the face and persistent dry mouth, which remain challenging issues for the patient despite several physiotherapy sessions. These complications highlight the importance of diagnosing MAC as early as possible to prevent nerve involvement and tumor growth, which complicate treatment and necessitate careful surgical planning and comprehensive postoperative care.
4 Conclusion
This case underscores the importance of a thorough diagnosis and a tailored treatment approach for MAC. The indolent yet potentially aggressive behavior of the tumor necessitates caution in long-term management to prevent recurrence and ensure patient well-being. This case's unique clinical presentation and prolonged duration highlight the complexities in diagnosing and managing MAC. The significant postoperative complications also emphasize the need for comprehensive patient care and support.
Author Contributions
Saman Al-Zahawi: writing – original draft, writing – review and editing. Neda Serkani: writing – original draft, writing – review and editing. Vahideh Sadat Azhari: visualization. Zahra Razavi: conceptualization, data curation. Kamran Balighi: conceptualization, data curation. Fatemeh Saberi: supervision, writing – original draft, writing – review and editing.
Acknowledgments
The authors are grateful to the Tehran University of Medical Science.
Consent
Written informed consent was obtained from the patient to publish this report per the journal's patient consent policy.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The authors elect to share data per request.