Experience With Vaughan-Jackson Syndrome at Eastern Regional Referral Hospital, Bhutan: Diagnosis and Its Treatment
Funding: The author received no specific funding for this work.
ABSTRACT
Vaughan-Jackson syndrome is a clinical diagnosis that does not require advanced investigations. Timely intervention with tendon suturing or reconstruction, along with addressing the offending structures, can result in a successful functional outcome.
1 Introduction
Digital extensor tendon injuries occur more frequently than flexor tendon injuries and are highly prevalent (61%) being located superficially and lacking overlying subcutaneous tissue [1]. The common mechanism of injury to the extensor tendon are direct laceration by sharp objects, injury due to a crush, avulsions, burns, animal or human bites, and deep abrasions [1]. There are reports on non-traumatic ruptures of the extensor tendon; however, the literature is very limited [2]. Few papers have reported on spontaneous rupture of the digital extensor tendon and its causes, such as Vaughan-Jackson syndrome, Kienbock's disease, rheumatoid arthritis, and distal radial fracture [1, 3]. Rheumatic arthritis is the most common cause of spontaneous rupture of the extensor tendons of the hand reported to date [4].
Vaughan-Jackson syndrome was first described by Oj Vaughan Jackson in 1948. In his original paper, he described a case series of two patients with spontaneous rupture of extensor tendons of the ring and little fingers secondary to osteoarthritis of the distal radio-ulnar joint(DRUJ) [3]. This syndrome, which is rare and not often well-documented, is not fully understood [5, 6]. Its pathophysiology includes attrition from bone margins in the DRUJ and ulnar head, chronic inflammation, and hypovascularity at the rupture site [7, 8]. Ulnar translation can also be seen in patients with traumatic injury to radiocarpal ligaments and in those with rheumatoid arthritis [7, 9]. However, in osteoarthritis patients with this syndrome, positive ulnar variance, volar carpal transition, and dorsal osteophyte formation are suggested as related factors [10, 11].
We hereby present a report of a Vaughan-Jackson syndrome case related to primary DRUJ OA and its treatment.
2 Case History and Examination
A 59-year-old male from one of the remotest parts of eastern Bhutan presented with the chief complaint of sudden painless loss of extension of the right ring and little fingers for 1 month. He was a right-hand dominant and doing his activities as usual before the incident. He was a farmer by occupation. He initially developed sudden painless loss of extension at the metacarpophalangeal (MCP) joint of the right little finger while cutting wood (Figure 1). There was no previous history of right wrist trauma nor known underlying diseases. He sought local treatment at his community but did not improve. After a month, he developed limitation of extension of the ring finger (Figure 2). Therefore, he visited the nearest hospital in his community, which ultimately led to a referral to Eastern Regional Referral Hospital.


The physical examination revealed dorsal prominence of the ulnar head, inability to extend the little finger and ring finger at the MCP joint (Figure 3). There was a palpable mass on the dorso-ulnar aspect of extensor zone 6. There were no abnormalities of skin or any scarring over the tendons. No subcutaneous nodules were noted. An absent tenodesis effect was noted over the affected digits. The range of motion of the forearm and wrist was normal.

3 Treatment
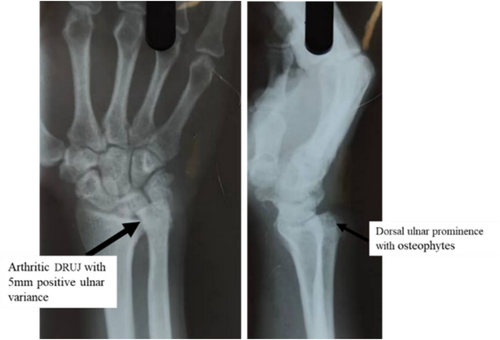
Differential diagnoses, including metacarpophalangeal joint dislocation, gout, and Dupuytren's contracture, were excluded. Rheumatoid arthritis was ruled out after assessing serum markers and applying clinical criteria for the condition. Radiographs of the wrist revealed distal radioulnar joint (DRUJ) arthritis with positive ulnar variance, dorsal prominence, and osteophytes (Figure 4). Consequently, Vaughan-Jackson syndrome of the right hand was diagnosed.
A detailed explanation of the patient's condition and its underlying cause was provided. The need for surgical intervention, including repair or reconstruction of tendons, along with treatment aimed at addressing the cause of the tendon rupture, was discussed. Preoperatively, plans included either a side-to-side tendon transfer or a tendon transfer combined with ulnar head resection.
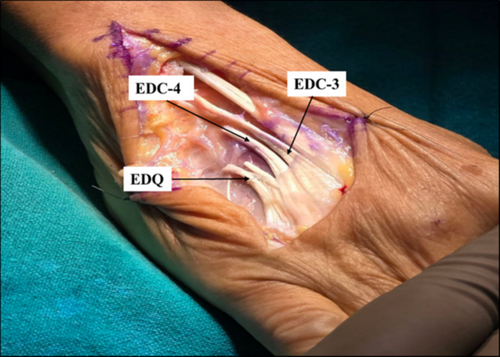
A brachial block was administered along with the application of a pneumatic tourniquet over the right upper limb. A dorsal longitudinal incision was made between the fourth and fifth finger web space extending to the ulnar head. The tendons of the extensor digiti quinti (EDQ) and the extensor digitorum communis (EDC) of the ring finger were found to be ruptured, with their distal ends matted together in scar tissue (Figure 5). The proximal ends were located just proximal to the DRUJ. Both distal tendon ends were friable but showed no established tenosynovitis. The distal stumps were meticulously debrided until healthy tendon tissue was identified.
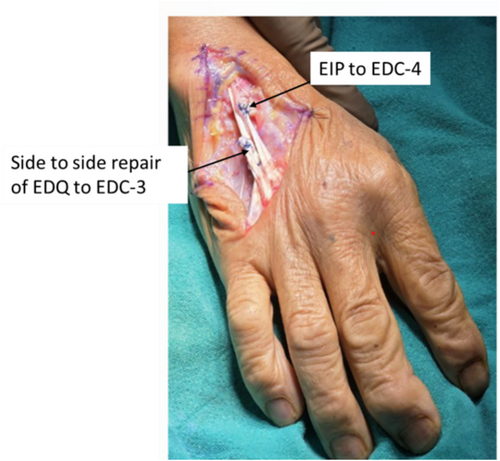
A Darrach procedure (ulnar head excision) was initially performed to prevent recurrent tendon rupture. Subsequently, a side-to-side repair of the EDQ tendon to the third extensor digitorum communis (EDC-3) tendon was performed, along with the transfer of the extensor indicis proprius (EIP) to the fourth extensor digitorum communis (EDC-4) (Figure 6). The tenodesis effect was achieved immediately post-repair.
4 Outcome and Follow Up
A cock-up splint with the metacarpophalangeal (MCP) joints fully extended and the interphalangeal joints in a neutral position was applied postoperatively. Gentle passive range-of-motion exercises were initiated in the third week, with active motion exercises started in the sixth week (Figure 7). The splint was removed 6 weeks postoperatively, and the patient was able to achieve both full active flexion and extension of the little and ring fingers, as illustrated in Figure 7. Strengthening exercises were recommended for an additional 2 weeks.

The patient was followed up at a local clinic 3 months postoperatively, where he demonstrated a full range of motion in all the affected digits.
5 Discussion
Vaughan Jackson syndrome is a rare condition without a defined prevalence. Literature on this syndrome is limited to case reports and case series. The clinical presentations of this syndrome are variable. In approximately half of the patients, tendon rupture may occur abruptly without prior signs, such as pain or swelling. In the other half, a history of distal radioulnar joint (DRUJ) pain may be present. Therefore, the presence or absence of pain does not definitely confirm or rule out tendon involvement [6, 8, 12].
Typically, the condition begins with weakness and/or the inability to extend the little finger because of the extensor digiti quinti (EDQ) rupture, which is a characteristic and diagnostic feature regardless of the prior nonspecific symptoms [3, 10, 11]. In our patient, the pain was absent, but the primary complaint was a limitation in the extension of the little finger, followed by the ring finger.
While the exact etiology of the condition is unknown, it is clear that the DRUJ arthritis, osteophytes, and ulnar head dysplasia, features that are all present in our patient play a critical role in the syndrome's progression [6, 10]. Moreover, it is associated with osteoarthritis, rheumatoid arthritis tenosynovitis, and joint erosion. Although uncommon, it may also be associated to Madelung's deformity, carpal bone loss, [12, 13] extravasation of intravenous infusions, [14, 15] gout or pseudogout-related arthropathies, [16] and Kienböck disease [5].
This syndrome significantly impacts the patient's quality of life and function, as it progresses rapidly and often affects the dominant hand [17]. Therefore, making an accurate and early diagnosis is imperative [18].
Vaughan-Jackson syndrome is associated with the repetitive use of the wrist during exercise, work, or daily activities and/or forced motion of the wrist or hand [5, 13]. In our patient, being a farmer with prolonged engagement in work-related activities, the condition is linked to underlying osteoarthritis of the DRUJ. The pathophysiology involves direct attrition caused by prominent bone margins in the DRUJ and ulnar head, chronic inflammatory changes, and hypovascularity at the rupture site [6, 18, 19].
The main aim of the treatment of this condition is to restore tendon function besides correcting the underlying etiology. Treatment options consist of: (1) reconstruction and/or transfer of tendons, (2) tendon protection and stabilization, (3) resection of the ulnar head and osteophytes along with synovectomy [19, 20]. A few cases of tendon transfer without ulnar head excision are reported, but these are associated with a higher risk of re-rupture. Therefore, the ulnar head excision should be included as a part of comprehensive treatment [6, 21]. Accordingly, ulnar head excision was performed alongside tendon transfer in our patient.
There are different methods of treatment for tendon rupture; however, tendon transfer is the first line of treatment [9, 22]. End-to-end tendon repair may be an option in acute cases, but it is not ideal in chronic presentations like our case. Although tendon grafting is another option but the need for a donor tendon and associated morbidity limit its usage [22]. Therefore, tendon transfer or side-to-side tendon suture technique is the best option in this case.
To achieve a successful outcome, treating the underlying structures causing the injury, repairing the extensor tendons, and implementing postoperative hand physiotherapy are essential components of management [5, 15].
6 Conclusion
Vaughan -Jackson syndrome is a rare condition; however, it is a progressive disorder that can affect the patient's quality of life and function. Early diagnosis and treatment are crucial for an optimal outcome. Comprehensive management involves treatment of offending structures causing the tendon rupture and restoring tendon function.
Author Contributions
Kinzang Dorji: conceptualization, data curation, formal analysis, investigation, methodology, project administration, writing – original draft, writing – review and editing.
Acknowledgments
The author has nothing to report.
Consent
An Informed written consent was obtained from the patient for the publishing of images and his case report.
Open Research
Data Availability Statement
The author has nothing to report.




