A Case of Trimethoprim-Sulfamethoxazole Associated Aseptic Meningitis
Funding: The authors received no specific funding for this work.
ABSTRACT
Most cases of aseptic meningitis, or nonsuppurative meningitis, are caused by viruses or systemic diseases. Nonetheless, drug-induced aseptic meningitis should be considered in the differential diagnosis, particularly with the recent use of antibiotics and nonsteroidal anti-inflammatory drugs. We describe a case of meningitis associated with the use of Trimethoprim-Sulfamethoxazole (TMP-SMX) in a 72-year-old male with comorbidities. A 72-year-old male with a history of diabetes, hypertension, Parkinson's disease, benign prostatic hyperplasia, and a recent use of TMP-SMX for a urinary tract infection (UTI) presented with altered mental status, neck rigidity, tachycardia, and a fever of 102.8°F. CT scan of the head and abdomen and chest x-ray revealed no significant findings. Empiric treatment with ampicillin, vancomycin, acyclovir, and ceftriaxone was initiated after two failed attempts at lumbar puncture, resulting in the improvement of all symptoms except for altered mental status within 24 h. Analysis of CSF, obtained via a successful subsequent lumbar puncture, was negative for microorganisms. The patient was labeled as a case of TMP-SMX-induced aseptic meningitis (TSIAM) due to the recent use of the drug for UTI. All the antibiotics and antivirals were discontinued, and all his symptoms resolved within 5 days of presentation. TSIAM is a diagnosis of exclusion, and a low threshold of suspicion should be maintained when CSF microscopy and culture show no microorganisms. This case illustrates the significance of prompt recognition of TSIAM and highlights the importance of thorough history-taking in preventing complications associated with drug-induced aseptic meningitis, thereby improving patient outcomes.
Summary
- Drug-induced aseptic meningitis, particularly from trimethoprim-sulfamethoxazole, can mimic symptoms of infectious meningitis, complicating diagnosis.
- Patients with autoimmune disorders, diabetes, or other predisposing conditions may be more prone to TSIAM. A comprehensive medical and drug history, along with CSF studies and imaging, is crucial for timely diagnosis and for preventing delays in care.
1 Introduction
Aseptic meningitis is an inflammatory condition of the meninges that is not associated with bacterial or fungal infection, presenting with symptoms of headache, nuchal rigidity, often leading to diagnostic challenges due to its overlapping symptoms with bacterial meningitis. Enteroviruses are the most frequent cause of aseptic meningitis, with autoimmune diseases, vaccines, leukemia, and drugs being the less common causes [1].
Drug-induced aseptic meningitis (DIAM) symptomatically can mimic infectious meningitis or meningitis secondary to the underlying condition being treated with these drugs. Therefore, diagnosing a DIAM case can be a challenging task for a physician. Nonsteroidal anti-inflammatory drugs (NSAIDs), antibiotics, intravenous immunoglobulins, and OKT3 antibodies (monoclonal antibodies against the T3 receptor) are considered to be the most frequent causes of DIAM [2]. Symptoms range from fever, headache, meningism, and mental status changes, and resolve with the withdrawal of TMP-SMX, over 48 to 72 h [3].
Trimethoprim-sulfamethoxazole (TMP-SMX) is considered the most commonly responsible culprit for antibiotic-associated aseptic meningitis [4]. It is a commonly prescribed antibiotic for various infections, including urinary tract infections (UTIs), pneumocystis jirovecii (formerly Pneumocystis carinii) pneumonia, otitis media, and shigellosis. Despite its widespread use, TMP-SMX is associated with many adverse effects, the most common being gastrointestinal reactions, hematotoxicity, anaphylaxis, and nephrotoxicity, and the less common being aseptic meningitis [1, 5, 6]. TMP-SMX-induced aseptic meningitis (TSIAM)–although a very rare side effect—is observed more commonly in women and in patients with autoimmune disorders [1].
Herein, we describe a case of a 72-year-old male who developed aseptic meningitis associated with TMP-SMX, highlighting the diagnostic process, treatment considerations, and the importance of recognizing this rare but significant side effect.
2 Case Description
A 72-year-old male was brought to the emergency department with altered mental status (AMS) persisting for the last 2 days. On presentation, the patient's Glasgow Coma Scale (GCS) score was 14/15, with spontaneous eye opening (E4), confused verbal responses (V4), and purposeful motor responses (M6). The mild confusion was consistent with toxic metabolic encephalopathy and the patient's baseline dementia. The patient's past medical history included diabetes, hypertension, Parkinson's disease, and benign prostatic hyperplasia (BPH), and some recent falls with no cardiovascular accident history. On examination, the patient exhibited a fever of 102.8°F, a heart rate of 116 beats per minute, and neck rigidity. On presentation, the patient's blood pressure was well documented over the last 24 h, ranging from 117 to 137 mmHg systolic to 66–73 mmHg diastolic, with the most recent recorded value being 126/73 mmHg.
3 Methods (Differential Diagnosis, Investigations, and Treatment)
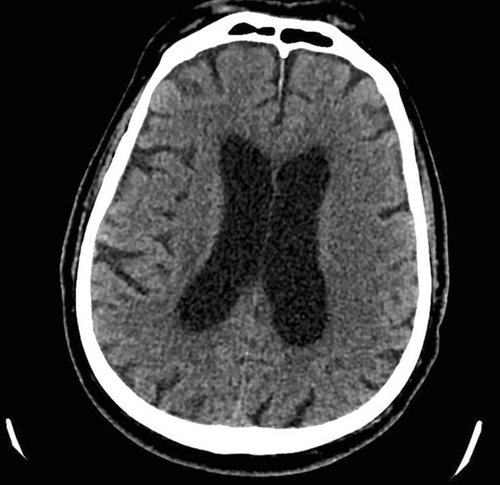
A CT scan of the head showed no acute demarcated territorial infarct or subarachnoid hemorrhage (Figure 1). A chest X-ray was done for possible consolidations or other findings of pneumonia; it revealed mild atelectasis within the dependent lung bases, with no evidence of pneumonia or pulmonary edema. A CT chest, abdomen, and pelvis was performed, indicated due to fever of unknown origin and vomiting to rule out intraabdominal pathology. The scan demonstrated normal findings in the colon and appendix, with no evidence of diverticulitis or colitis. Notably, the patient had recently used Bactrim for a presumed urinary tract infection (UTI). The patient developed altered mental status and fever 2 weeks after starting TMP-SMX for a presumed UTI.
The presence of neck rigidity, fever, and altered mental status indicated a diagnostic suspicion of meningitis. Two failed attempts of lumbar puncture were performed in the ED, and the patient was initiated on empiric treatment with ampicillin, vancomycin, acyclovir, and ceftriaxone. Top of Form Laboratory investigations revealed negative blood cultures after 24 h. Similarly, urine analysis showed the absence of leukocytosis or elevations in markers for UTI. Vital signs normalized within 24 h, with the patient's temperature ranging from 97.8°F to 98.8°F, pulse at 52 beats per min, respiratory rate at 18 breaths per min, blood pressure at 126/73 mmHg, and oxygen saturation between 95% and 100%. During the hospital stay, the patient's laboratory evaluation exhibited anemia and low calcium levels. The patient demonstrated mild anemia with hemoglobin of 12.3 g/dL (consistent with anemia of chronic disease) and mild hypocalcemia with a calcium level of 8.2 mg/dL.
A systemic review after 24 h showed no significant findings, and the physical examination was largely unremarkable except for the patient's altered mentation, which remained close to the baseline presentation. A lumbar puncture was successfully performed via CT guidance at the L2–L3 level following consultation with Neuro Interventional Radiology (NIR). The cerebrospinal fluid analysis was negative for any microorganisms, including Haemophilus influenzae, Streptococcus A, and Streptococcus pneumoniae (Table 1).
| Parameter | Result |
|---|---|
| Opening pressure | 12 cm H2O |
| Appearance | Clear |
| WBC | < 1/μL |
| RBC | 0/μL |
| Glucose | 65 mg/dL |
| Protein | 42 mg/dL |
| Gram stain | Negative |
| Bacterial cultures | Negative |
| Multiplex meningitis/encephalitis panel | Negative (includes HSV, VZV, enterovirus, etc.) |
Altered mental status is a common but complex presentation with multiple potential causes. In our case, differentials included infectious etiologies (e.g., meningitis, encephalitis), metabolic derangements (e.g., hypocalcemia, uremia), medication side effects (i.e., antibiotics), and structural causes (e.g., stroke, microvascular ischemic changes). Consequently, we conducted comprehensive investigations, including a lumbar puncture, metabolic panel, and CT head, which ruled out infectious, metabolic, and structural causes, respectively (Table 2). The timeline of symptoms and resolution after discontinuing TMP-SMX strongly supported a diagnosis of TSIAM.
| Differential diagnosis | Investigations performed | Results/findings |
|---|---|---|
| Meningitis (bacterial/viral) | Lumbar puncture, CSF analysis | Negative |
| Structural brain pathology | CT head | No acute findings |
| Metabolic/toxic encephalopathy | Labs: glucose, electrolytes, calcium, etc. | Mild hypocalcemia only |
| Drug-induced encephalopathy | Medication review (TMP-SMX timeline) | Strong temporal association |
Since the diagnosis (of exclusion) was pointing towards the TMP-SMX use for the UTI as the likely cause of the patient's symptoms, all antibiotics, including TMP-SMX and antivirals, were discontinued after 5 days of presentation. The diagnosis of TSIAM was made based on the temporal association with TMP-SMX use (symptom onset 2 weeks after starting), exclusion of infectious or other causes (negative LP and serologies), and resolution of symptoms upon discontinuation of TMP-SMX.
4 Conclusion and Result (Outcome and Follow-Up)
The patient's altered mental status resolved only after the complete cessation of TMP-SMX. Management of comorbidities included treatment as needed for elevated point-of-care glucose levels in diabetes. The patient was continued on carbidopa-levodopa 25–100 mg three times daily and carbidopa-levodopa extended-release (SINEMET CR) 25–100 mg one tablet nightly for Parkinson's disease and associated progressive supranuclear palsy. A Foley catheter was retained to manage BPH-related urinary incontinence. Hypertension was stable off medication.
5 Discussion
TMP-SMX is an FDA-approved, widely used antibiotic for infections such as acute infective exacerbation of chronic bronchitis, otitis media, traveler's diarrhea, urinary tract infections, shigellosis, Pneumocystis jirovecii pneumonia/pneumocystis carinii pneumonia (PJP/PCP), and toxoplasmosis [5]. However, the adverse effects of this drug warrant careful consideration. One such life-threatening side effect of this drug is TMP-SMX induced aseptic meningitis (TSIAM). In a study that collected case reports and case series published before July 31, 2023, 55 such cases of TSIAM were collected [1]. In another study that reviewed literature from 1990 to 2019, 42 such cases were identified [6]. In yet another study, the symptoms of meningitis were reproduced after a TMP-SMX rechallenge in a suspected case of TSIAM [7].
The patient's stable blood pressure suggests stable hemodynamics with no evidence of significant hypotension or hypertension, both of which could influence cerebral perfusion or contribute to worsening neurological symptoms. The stable blood pressure supports adequate cerebral perfusion at the time of evaluation, minimizing the likelihood of secondary ischemic or hypoperfusion-related brain injury.
CSF analysis in our patient could not be attained at first due to two failed lumbar puncture attempts. Hence, in the presence of meningitis symptoms, the patient was treated with ampicillin, vancomycin, acyclovir, and ceftriaxone. Our patient reported consistent symptoms of altered mental status even after the resolution of other meningitis symptoms. The altered mental status resolved only after complete cessation of TMP-SMX, further strengthening the diagnosis of TSIAM. This also highlights the importance of CSF analysis in suspected TSIAM patients, which can help prevent polypharmacy, especially in the elderly population. The exact mechanism of TSIAM is not clear. However, a study hypothesizes IL-6 as an important mediator in TSIAM, attributed to the raised level of IL-6 in such patients [8]. Another study suggests hypersensitivity, direct irritation, and toxicity as possible mechanisms for TSIAM [9]. Hypersensitivity type I and type II have also been proposed as a possible mechanism of TSIAM. A study claims the presence of immune complexes in the plasma in cases of TSIAM [10]. Another study also points out the possible binding of the drug to the human leukocyte antigen (HLA) on T-cell receptors and, hence, eliciting a type IV hypersensitivity reaction [11].
TSIAM is a rare but potentially severe adverse effect of TMP-SMX. Risk factors include advanced age, diabetes mellitus, and chronic illnesses, all of which were present in this patient. The presence of these factors, coupled with the onset of symptoms shortly after TMP-SMX initiation, underscores the importance of careful consideration when prescribing TMP-SMX in high-risk populations. In our case, the patient developed symptoms of altered mental status and fever ~2 weeks after initiating TMP-SMX for a presumed urinary tract infection. Symptoms improved significantly following TMP-SMX discontinuation, further supporting the diagnosis of TSIAM.
Predisposing factors for TSIAM include autoimmune diseases, diabetes, immunosuppression, and alcohol abuse [7]. In a study of 55 TSIAM cases, out of 27 patients whose past medical history was provided, 10.9% of the patients were immunocompromised with HIV, 10.93% had autoimmune diseases like Systemic lupus erythematosus (7.3%) and Sjogren syndrome (3.63%), and 3.63% had diabetes [1]. Our patient also had a history of diabetes; diabetes, being an immunocompromised state, seems to be making patients susceptible to TSIAM as reported by other cases of TSIAM in patients with a diabetic history [12]. Studies also show that the occurrence of TSIAM was higher in females than in males, which can be attributed to the higher incidence of autoimmune diseases in the female population [1, 6, 7]. The higher incidence of TSIAM in the female population can also be due to the higher number of UTIs in the female population, for which TMP-SMX is one of the first-line treatments [1].
Our patient also had a history of BPH that predisposed him to infections of the urinary tract for which the patient was treated with TMP-SMX. The use of TMP-SMX in UTI and its correlation with TSIAM cannot be ignored. One study reported that 61.8% of patients in its study population were prescribed TMP-SMX for the treatment of UTI, a finding reported in our case as well [1]. Our patient had an additional history of hypertension. The same study also reports that 10.9% of its study population had concomitant use of other medications including hydrochlorothiazide and lisinopril, which are first-line drug treatments for hypertension.
An important clinical question in such cases is, what are the chances that a patient presenting with meningitis symptoms and a recent history of TMP-SMX intake has TSIAM? In general, antibiotic-induced aseptic meningitis is a rare occasion and should only be diagnosed after other potential causes of meningitis have been excluded with CSF analysis and imaging. However, among the reported cases of antibiotic-induced aseptic meningitis, TMP-SMX or cotrimoxazole is the most identified culprit [13]. Additionally, in a previously stated study that identified possible predisposing factors for TSIAM, the probability of TSIAM should not be ignored if the said predisposing factors are present in a meningitis patient with recent TMP-SMX intake [5].
6 Conclusion
TSIAM, being the diagnosis of exclusion, poses a challenge for physicians to diagnose and manage in clinical settings. This study highlights the importance of predisposing factors in the diagnosis of TSIAM. It is also important to recognize the importance of thorough medical and drug history, in addition to CSF studies and imaging, to reach a diagnosis early and prevent any delay in care. Despite the condition resembling bacterial and secondary meningitis, the primary step in the treatment of TSIAM is the complete cessation of the offending drug, TMP-SMX.
Author Contributions
Malik W. Z. Khan: conceptualization, visualization, writing – original draft, writing – review and editing. Abdul Moeez: conceptualization, writing – original draft, writing – review and editing. Sameen Farooq: project administration, supervision, writing – review and editing. Adam Saeed: data curation, writing – original draft, writing – review and editing. Salma Qudrat: conceptualization, visualization, writing – original draft. Farishta Ali: validation, visualization, writing – review and editing. Faheemullah Khan: data curation, resources, writing – review and editing.
Acknowledgments
The authors acknowledge the cooperation of the patient and their family.
Consent
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data used to support the findings of this study are included within the article.




