An Unusual Case of 11αB-Crystallin (CRYAB) Mutation as a Cause of Dilated Cardiomyopathy With Restrictive Physiology: A Case Report and Focused Review of the Literature
Funding: This work was supported by Pontificia Universidad Javeriana.
ABSTRACT
Several diseases have been linked to αB-crystallin (CRYAB) mutation. However, this mutation is an uncommon cause that has been associated in recent years with the development of dilated cardiomyopathy. We report a case of dilated cardiomyopathy with restrictive physiology due to a CRYAB mutation.
1 Introduction
The CRYAB gene encodes the protein Alpha-B-crystallin, or αB-crystallin, a protein belonging to the small heat shock family of proteins that has been linked to normal cardiac homeostasis as well as cardiomyopathies, among other diseases [1]. CRYAB, the causal gene, is 3.2 kilobases long and situated on chromosome 11 [2]. Although its role as a molecular chaperone for desmin is well established, it also engages in interactions with a diverse range of other proteins [1].
Mutations in the CRYAB gene have been associated with congenital cataracts, myopathies, neurodegenerative diseases, as well as hypertrophic cardiomyopathy (HCM), and less commonly with dilated cardiomyopathy (DCM) and restrictive cardiomyopathy (RCM) [1, 3-5].
However, the CRYAB association with DCM has recently emerged in the last decade, which is why it may not be included in the list of genetic mutations associated with DCM according to the most recent guidelines of the European Society of Cardiology (ESC) and some reviews in recent literature. However, increasing emerging observational evidence suggests an association with DCM.
Moreover, HCM, RCM, and DCM can lead to the development of chronic heart failure (HF), either with preserved ejection fraction or with reduced ejection fraction, conditions that must be treated according to current guidelines [6-9]. Respecting the treatment of HF with preserved ejection fraction; the current guidelines give a Class I recommendation to use a sodium-glucose cotransporter-2 (SGLT2) inhibitor, diuretics for fluid retention, and to treat for etiology, cardiovascular, and non-cardiovascular comorbidities [7-9].
Furthermore, regarding the treatment of HF with reduced ejection fraction, the current guidelines likewise give a Class I recommendation to use first-line SGLT2 inhibitors, as well as angiotensin receptor/neprilysin inhibitors, beta-blockers, and a mineralocorticoid antagonist. Although additional interventions could be required if the patient persists in being symptomatic despite these initial interventions [7-9].
Below we describe the case of a patient who developed HF with reduced ejection fraction due to DCM with restrictive physiology secondary to a heterozygous mutation of the CRYAB gene.
2 Case History/Examination
A 42-year-old man with a history of heart failure with a mildly reduced ejection fraction of 42% in whom the etiology of it was under evaluation consulted the heart failure program at a university hospital. He was receiving standard heart failure medications with sacubitril/valsartan, carvedilol, spironolactone, and empagliflozin at maximum tolerable doses. Among his previous studies, a transthoracic echocardiogram showed a left ventricle with normal size and diameter, systolic dysfunction with a 43% left ventricular ejection fraction (LVEF), grade III diastolic dysfunction, severe tricuspid regurgitation, and moderate mitral regurgitation, along with severe biatrial enlargement and a high probability of pulmonary hypertension.
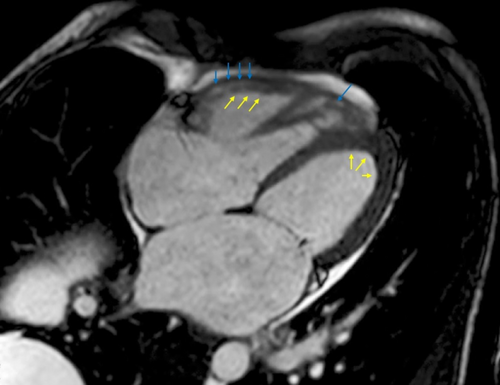
Besides, a cardiac magnetic resonance (CMR) with late gadolinium enhancement showed a left ventricle with mild dilatation and a decreased systolic function, without contractility disorders; however, there was late generalized gadolinium endocardial enhancement with severe mitral regurgitation and moderate tricuspid regurgitation, along with a biatrial and right ventricle dilatation (Figure 1), suggesting a DCM with restrictive physiology, taking into account the previously performed transthoracic echocardiogram.
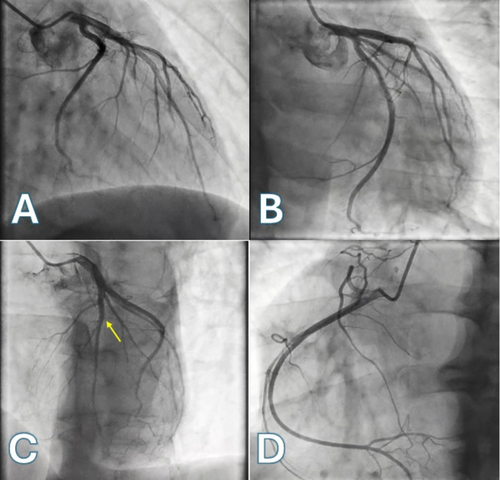
Besides, secondary causes of DCM such as Chagas disease, alcoholic cardiomyopathy, drugs and toxins causing DCM, myocarditis, and autoimmune disorders were also ruled out. Coronary artery disease (CAD) was ruled out too after performing a coronary arteriography (Figure 2).
After holding a multidisciplinary medical meeting, the medical staff considered that the patient had a heart failure with mildly reduced ejection fraction due to a DCM with restrictive physiology from idiopathic or genetic etiology, for which reason genetic testing of 76 cardiomyopathy genes was carried out, which ruled out the very common, common, and less common mutation genes for DCM among other cardiomyopathies, according to the ESC guidelines [6]. Nevertheless, a heterozygous CRYAB mutation was detected as a potential cause of cardiomyopathy.
Consequently, after genetic counseling and also after performing research regarding this mutation, which was found, a DCM with restrictive physiology due to the CRYAB mutation was diagnosed, highlighting the fact that the CRYA mutation is not a common gene mutation related to DCM according to the most recent ESC guidelines [6].
3 Differential Diagnosis, Investigations and Treatment
- Infectious causes (post-myocarditis): Chagas disease, viral (enteroviruses, adenoviruses, echoviruses, herpes viruses, parvovirus B19, HIV, SARS-CoV-2), bacterial (Lyme disease), mycobacterial, and fungal.
- Toxic and overload causes: Ethanol, cocaine, amphetamines, ecstasy, cobalt, anabolic/androgenic steroids, hemochromatosis, and other causes of iron overload.
- Endocrinology causes: Hypothyroidism and hyperthyroidism, Cushing's/Addison's disease, pheochromocytoma, acromegaly, diabetes mellitus.
- Nutritional deficiency causes: Selenium, thiamine, zinc, copper, and carnitine deficiencies have been described.
- Drugs: Antineoplastic drugs and mainly anthracyclines, but also antimetabolites, alkylating agents, taxol, hypomethylating agents, monoclonal antibodies, tyrosine kinase inhibitors, and immunomodulating agents. Besides, psychiatric drugs like clozapine, olanzapine, chlorpromazine, risperidone, lithium, methylphenidate, and tricyclic antidepressants. Finally, other drugs like all-trans retinoic acid, antiretroviral agents, and phenothiazines have been described.
- Peripartum
After reviewing the diagnostic criteria and performing an exhaustive interrogation and physical examination, and after performing the laboratory tests indicated for these diagnoses, these conditions were ruled out. Therefore, it is important to keep in mind that within the diagnostic approach of this cardiomyopathy, secondary non-genetic diseases must be ruled out; likewise, carrying out an adequate family pedigree of the patient's relatives in order to guide a possible genetic origin of the cardiomyopathy.
In our case, no first- or second-degree relatives of the patient had a history of cardiomyopathies or other relevant diseases, which is why it was considered a de novo mutation.
4 Outcome and Follow Up
During follow-up, despite the treatment of heart failure with optimal medical therapy, including foundational therapy and cardiac rehabilitation among others, his mitral and tricuspid regurgitations progressed to a worse severe grade, preventing an improvement in the symptoms reported by the patient, with a gradual increase in symptoms. This is why, after holding a new medical meeting, it was considered that he was a candidate for mitral valve replacement and tricuspid valve plasty. Besides, a myocardial biopsy was performed during the surgery.
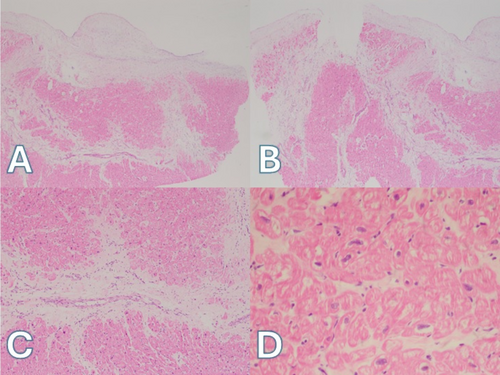
Although in an interesting way, the myocardial biopsy revealed endocardial and subendocardial fibrosis with anisonucleosis of the cardiomyocytes, also with altered architecture of the myocardial fibers (Figure 3). Currently, the patient is receiving optimal medical therapy for his heart failure and is undergoing cardiac rehabilitation.
5 Discussion
Regarding cardiomyopathies, the CRYAB mutation gene has been linked to HCM as a common mutation gene, according to the ESC guidelines [6]. However, after performing a review of the available medical literature in the major clinical databases (Pubmed, Google Scholar, and Scielo), we found some manuscripts describing a relation between the CRYAB mutation and DCM in humans [2, 4, 10, 11].
Regarding DCM, it's important to keep in mind that it is defined by the presence of left ventricular dilatation and systolic dysfunction unexplained solely by abnormal loading conditions or coronary artery disease (CAD) [6]. In our case, abnormal loading conditions were ruled out, as CAD was confirmed by right and left coronary arteriography without epicardial lesions.
According to epidemiology, familial DCM accounts for 30%–40% of all DCM cases; in 20%–40% of those cases, a gene has been found [4, 6]. According to the ESC guidelines, the very common, common, or less common genes associated with DCM include ABCC9, ACTC1, ACTN2, ANKRD1, BAG3, CSRP3, CTF1, DES, DMD, DSG2, DSP, DTNA, EYA4, FLNC, GATAD1, ILK, JPH2, LAMA4, LDB3, LMNA, LRRC10, MIB1, MYBPC3, MYH6, MYH7, MYL2, MYL3, MYPN, NEBL, NEXN, NKX2-5, NPPA, OBSCN, PDLIM3, PKP2, PLEKHM2, PLN, PRDM16, PSEN1, PSEN2, RBM20, SCN5A, SGCD, TBX20, TCAP, TMEM43, TMP0, TMNC1, TNNI3, TNNI3K, TNNT2, TPM1, TTN, and VCL [6].
Despite the CRYAB mutation not being included in the previous list, in the last years this mutation has been described as a pathogenic mutation in DCM in several articles [2, 4, 10, 11]. In our case, a heterozygous CRYAB mutation was detected after excluding other causes of secondary DCM and may be de novo due to the absence of documented cardiomyopathies in his relatives.
Respect the physiopathology why this mutation causes cardiomyopathy; in mouse models, it has been found that an R120G missense mutation causes “desmin-related cardiomyopathy,” which is characterized by the formation of aggregates of oligomeric amyloid containing CRYAB and desmin with accumulation of them within cardiac muscle, generating mitochondrial deficiencies, activation of apoptosis, and heart failure [12, 13]. These oligomeric amyloid intermediates have also been seen in cardiomyocytes from many humans with dilated and hypertrophic cardiomyopathies [12, 13].
Besides, it has even been shown that this mutation in vitro cardiomyocytes leads to mitochondrial dysfunction and subsequent apoptosis, which eventually results in cardiomyocyte death, dilatation, and heart failure [14].
Moreover, it has been proposed that naturally occurring mutations in the gene encoding alpha-B-crystallin, CRYAB, modify ionic intermolecular interactions that impact chaperone function and dimerization. Through various mechanisms, including desmin aggregation, increased reductive stress, or stimulation of calcineurin-NFAT signaling, these mutations induce pathological hypertrophy and have been linked to the development of myofibrillar myopathy, RCM, HCM, and DCM [1].
Regarding the treatment of chronic heart failure with reduced ejection fraction, it must be according to the international guidelines provided by the ESC and ACC guidelines, among other relevant guidelines [7-9]. However, regarding the treatment of genetic DCM, it is important to assess if the patient carries some specific mutations associated with an increased risk of sudden cardiac death, like FLNC, DES, DSP, PLN, LMNA, TMEM43, and RMB20, among others [6]. In our case, these mutations were ruled out.
Although predicting SCD is a challenging aspect of the clinical care of patients with DCM, mainly in primary prevention, because in secondary prevention they have demonstrated a reduction in mortality among survivors of cardiac arrest and in those who have experienced sustained ventricular arrhythmias with hemodynamic compromise [6].
Nevertheless, a LEVF ≤ 35% has been reported as an independent risk marker of all-cause and cardiac death in DCM despite its modest ability to identify DCM patients with a higher risk of SCD; also, DCM patients harboring DCM-causing variants in high-risk genes (LMNA, EMD, TMEM43, DSP, RBM20, PLN, FLNC-truncating variants) should be considered as patients with a high-risk genetic background for SCD, and primary prevention ICD implantation should be considered with LVEF thresholds higher than 35% [6]. In our case, these conditions were absent, so actually, an indication to implant an ICD for primary prevention is not considered.
Likewise, in an interesting way, voluntary exercises have shown a significant improvement in survival among a mouse model, also reducing the accumulation of preamyloid due to the CRYAB mutation, slowing the progression of heart failure in this animal model. Nevertheless, more research is needed to confirm this finding in humans [15].
Finally, it is important to remark that while more evidence emerges regarding the association of the CRYAB gene and DCM, it is probable that this gene will be included in the genetic screening in DCM suggested by cardiomyopathy guidelines. Currently, this gene mutation may be considered in the screening of DCM after ruling out very common, common, or less common genes associated with DCM according to current ESC guidelines, also taking into account that genetic testing may be indicated in the patient relatives [6].
6 Conclusions
Even though CRYAB mutations have been linked mainly with HCM according to the ESC guidelines, new emerging evidence relates it to DCM cases, whereby, in the presence of a DCM, this mutation may be considered an unusual potential cause to be screened within the diagnostic approach in the genetic test screening.
Author Contributions
Porras Bueno Cristian Orlando: conceptualization, data curation, formal analysis, investigation, methodology, project administration, supervision, validation, writing – original draft, writing – review and editing. Cruz Buitrago Roberto Hernando: conceptualization, data curation, formal analysis, investigation, writing – original draft, writing – review and editing. Mariño Correa Alejandro: conceptualization, data curation, formal analysis, investigation, methodology, project administration, supervision, validation, writing – original draft, writing – review and editing. Cáceres Méndez Edward Andres: conceptualization, data curation, formal analysis, investigation, methodology, project administration, supervision, validation, writing – original draft, writing – review and editing. Eugenio Meek: conceptualization, data curation, formal analysis, investigation, writing – original draft, writing – review and editing. Ríos Dueñas Edgar Giovanni: conceptualization, data curation, formal analysis, investigation, writing – original draft, writing – review and editing.
Acknowledgments
To the Pontifical Xavierian University and its cardiology department for promoting publication and research.
Ethics Statement
The publication of this case has been approved by the institutional ethics committee.
Consent
In compliance with the journal's patient consent policy, written informed consent was obtained from the patient to publish this report.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.