Atrial Septal Defect and Percutaneous Closure: Healing the Heart From Within
Funding: The authors received no specific funding for this work.
ABSTRACT
Early diagnosis and percutaneous closure of symptomatic adult atrial septal defects can enhance cardiac function and relieve symptoms. Thorough pre-procedural evaluation and diligent follow-up care are essential for achieving the best outcomes and ensuring long-term success.
1 Introduction
Atrial septal defect (ASD) is a congenital heart defect characterized by an abnormal opening in the atrial septum, which separates the left and right atria of the heart. It allows for abnormal blood flow between these chambers, often leading to significant clinical symptoms and complications if left untreated. ASDs are commonly diagnosed in adulthood, despite being present from birth, due to their often asymptomatic nature in childhood [1, 2]. This condition can manifest through various symptoms, including central chest pain, shortness of breath on exertion, and palpitations, which can significantly impact a patient's quality of life [3].
The presentation of ASD can be subtle and varies depending on the size of the defect and the presence of associated hemodynamic changes. Larger ASDs tend to cause more noticeable symptoms due to increased blood flow and pressure changes within the heart. These changes can lead to right atrial and right ventricular enlargement, which may further exacerbate symptoms such as dyspnea and fatigue [4]. In cases where symptoms are not apparent, the defect may be discovered incidentally during evaluations for unrelated issues or through routine screening [5].
The diagnostic approach for ASD involves a combination of clinical assessment, electrocardiography (ECG), and echocardiography. An ECG may show right bundle branch block or right ventricular conduction delay, which can be indicative of ASD [6]. Transesophageal echocardiography (TEE) is employed when TTE does not provide sufficient detail, especially in complex cases or when a more precise assessment of shunt severity is required. Transthoracic echocardiography (TTE) is typically the first-line imaging modality, revealing the size of the defect and assessing its hemodynamic impact. TEE is employed when TTE does not provide sufficient detail, especially in complex cases or when a more precise assessment of shunt severity is required [7].
Management of ASD depends on the size of the defect, the presence of symptoms, and the overall impact on cardiac function. For patients with significant symptoms or evidence of right heart enlargement, closure of the defect is often indicated. This can be achieved through either surgical or percutaneous techniques. Percutaneous closure using devices such as the Amplatzer septal occluder has become the preferred approach due to its less invasive nature and favorable outcomes [8, 9]. The procedure involves the deployment of a closure device via a catheter inserted through the femoral vein, guided by fluoroscopy and echocardiography [10]. Post-procedure, patients typically require antiplatelet therapy to prevent thromboembolic complications and may continue on diuretics to manage residual symptoms [11].
The successful closure of ASD often results in the resolution of symptoms and improved cardiac function. Follow-up care is essential to monitor the effectiveness of the device, assess for any residual shunting, and ensure overall cardiac health. Regular echocardiographic evaluations are standard practice to confirm the stability of the closure device and to detect any potential complications early [12]. As the understanding of ASD management continues to evolve, ongoing research and advancements in technology contribute to improving patient outcomes and reducing the need for more invasive procedures. Here, we present a case of a 46-year-old female with late onset symptoms due to ASD.
2 Case History/Examination
The patient, a 46-year-old female housemaker, presented with central chest pain that had been intermittent for the past year but progressively worsened over the previous 2 months. She also reported experiencing shortness of breath on exertion during this period and had palpitations for the past month. She had no known history of other comorbid illnesses and did not smoke or consume alcohol.
On physical examination, she was alert and oriented to time, place, and person. Her vital signs were as follows: pulse rate of 74 beats per minute, blood pressure of 90/60 mmHg, respiratory rate of 12 breaths per minute, and oxygen saturation of 98% on room air. There were no observable signs of pallor, jaundice (icterus), lymphadenopathy, cyanosis, clubbing, edema, or dehydration. Auscultation of the chest revealed bilateral equal air entry with no additional abnormal sounds. Cardiovascular examination noted a widely split second heart sound over the second left intercostal space. The rest of the systemic examination was unremarkable.
3 Methods (Differential Diagnosis, Investigations, and Treatment)
The initial differential diagnosis included coronary artery disease, pulmonary embolism, and heart failure. Given the patient's age and symptoms, coronary artery disease was considered; however, the normal ECG findings and lack of significant cardiac biomarkers made this diagnosis less likely. Pulmonary embolism was also considered but was less probable due to the patient's normal oxygen saturation and absence of additional symptoms typically associated with embolism. Heart failure was a possible diagnosis due to the presence of right atrial and right ventricular dilatation observed on imaging; however, the patient's left ventricular ejection fraction (LVEF) was found to be normal after the procedure, making this diagnosis less likely. The most probable diagnosis was an ASD, which was supported by imaging studies and clinical presentation.
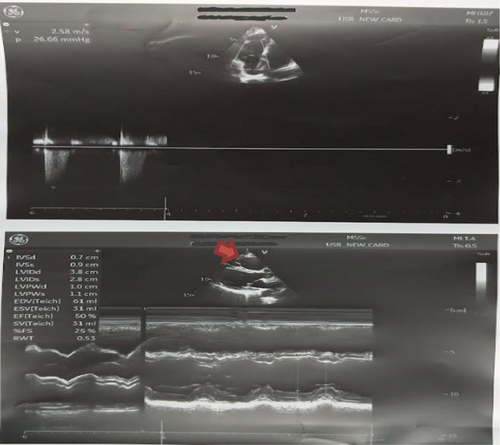
The diagnostic workup included an ECG showing an rSR pattern in V1 and V2, often indicative of right bundle branch block or right ventricular conduction delay (Figure 1). A transthoracic echocardiogram (TTE) revealed an ostium secundum ASD measuring 10 × 12 mm with mild tricuspid regurgitation (TR) and dilatation of the right atrium and right ventricle (Figure 2). The LVEF was noted to be between 40%–45%, indicating some degree of compromised cardiac function. Further evaluation with TEE confirmed a larger ASD measuring 15 × 18 mm with significant left-to-right shunting, which was deemed suitable for device closure. Cardiac catheterization and fluoroscopy were utilized to confirm the ASD size, verify the absence of associated partial anomalous pulmonary venous return (PAPVC), and guide the deployment of the closure device.


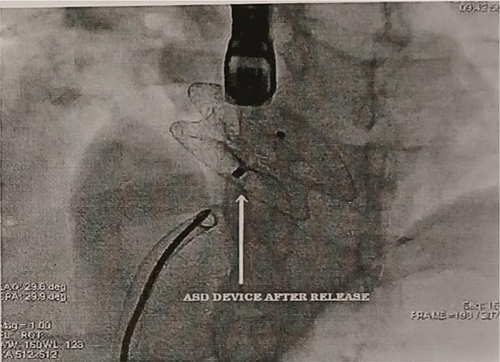
The initial management plan included the use of diuretics: furosemide 10 mg daily and spironolactone 25 mg daily to manage symptoms and reduce fluid overload. The patient was scheduled for an ASD device closure procedure. The procedure was performed via the right femoral vein under general anesthesia, using fluoroscopy and TEE for guidance. The ASD size was reconfirmed as 20 mm using a sizing balloon. An Amplatzer septal occluder (24 mm) was deployed using the left upper pulmonary vein technique (Figure 3). The device was carefully positioned and confirmed stable via TTE, TEE, and fluoroscopy (Figure 4). Post-procedure, the patient was placed on dual antiplatelet therapy for 1 month to prevent thromboembolic complications. Continued use of Furosemide and Spironolactone was advised to manage residual symptoms.
4 Results and Conclusion (Outcome and Follow-Up)
The ASD device closure was successful, with no residual shunt observed on post-procedure TTE. Mild tricuspid regurgitation was present, with a gradient of 26 mmHg. The right atrium and right ventricle, though still dilated, showed improved function with an LVEF of 60% post-procedure. The resolution of symptoms such as chest pain, shortness of breath, and palpitations was anticipated as the patient continued to recover.
Follow-up care was crucial to monitor the function of the ASD closure device, assess for any residual shunting, and ensure overall cardiac health. The patient continued with dual antiplatelet therapy for 1 month, and her management regimen included ongoing treatment with furosemide and spironolactone as necessary. Regular follow-up visits were scheduled to ensure optimal recovery and address any further issues that might arise.
5 Discussion
ASD is a common congenital heart condition that can present with a range of symptoms depending on the size of the defect and the presence of associated complications. This case presents a 46-year-old female with progressive central chest pain, shortness of breath on exertion, and palpitations, which were ultimately attributed to an ASD. The novelty of this case lies in the patient's relatively late presentation, the detailed diagnostic approach employed, and the successful outcome achieved through percutaneous closure.
ASD often remains asymptomatic in childhood, and symptoms typically manifest later in life, sometimes decades after birth. This patient's presentation at age 46 with worsening symptoms over a year, including progressive chest pain and exertional dyspnea, highlights a critical aspect of ASD management: the need for heightened awareness of this condition in adults, particularly those with unexplained cardiac symptoms or right heart enlargement. Although ASDs are frequently diagnosed in children or young adults, adult cases are becoming increasingly recognized due to improved diagnostic techniques and greater awareness among clinicians [1].
In comparing this case with other reported cases, the diagnostic approach utilized here aligns with current best practices but also illustrates some unique aspects. For instance, the use of a TTE followed by TEE for detailed assessment is consistent with established guidelines for ASD evaluation [2]. However, the integration of fluoroscopic guidance during the percutaneous closure procedure, while standard, underscores the precision required in modern interventional cardiology. This case emphasizes the importance of a multimodal diagnostic approach, including advanced imaging techniques and detailed hemodynamic assessments, to accurately characterize the defect and plan appropriate treatment.
The patient's ASD was initially identified as an ostium secundum type, which is the most common form of ASD [4]. The progression to a larger defect of 20 mm observed during the procedure, as well as the significant left-to-right shunting, underscores the importance of precise measurements and the potential for changes in defect size over time. The presence of mild tricuspid regurgitation and right heart dilation further complicated the clinical picture but also provided additional insight into the hemodynamic impact of the ASD. This highlights the importance of thorough pre-procedural assessment to inform the choice of intervention and predict potential post-procedural outcomes.
The successful use of an Amplatzer septal occluder in this case is noteworthy. This device has become a standard for ASD closure due to its effectiveness and safety profile [4]. Compared to surgical closure, percutaneous techniques have the advantage of reduced recovery time and fewer complications, making them a preferred option for many patients. This case's outcome, with resolution of symptoms and improvement in cardiac function, reflects the efficacy of this approach. The patient's LVEF improved from 40%–45% pre-procedure to 60% post-procedure, indicating significant functional recovery, a finding consistent with other studies reporting similar improvements in cardiac function following ASD closure [9].
A comparison with other cases reveals that while ASD closure outcomes are generally favorable, individual results can vary based on factors such as defect size, patient age, and comorbid conditions. For instance, a study by Tzemos et al. found that device closure of ASDs in adults led to significant symptomatic relief and improved cardiac function, similar to the results observed in this case [8]. Conversely, complications such as residual shunting or device-related issues can occur, necessitating careful long-term follow-up. This case emphasizes the importance of a multimodal diagnostic approach, including advanced imaging techniques and detailed hemodynamic assessments, to accurately characterize the defect and plan appropriate treatment.
Furthermore, the use of dual antiplatelet therapy following ASD closure, as observed in this case, is a well-established practice to prevent thromboembolic events. This approach is supported by evidence showing that dual antiplatelet therapy effectively reduces the risk of device-related thrombus formation and stroke [11]. The continued use of diuretics to manage residual symptoms also aligns with standard postoperative care protocols and reflects a comprehensive approach to managing ASD-related complications.
This case contributes valuable insights into the management of adult ASD, particularly regarding late presentation and the use of advanced diagnostic and interventional techniques. The patient's successful outcome following percutaneous closure with an Amplatzer septal occluder highlights the effectiveness of modern treatment approaches and reinforces the importance of individualized care. Continued research and clinical experience will further refine these approaches, ensuring that patients with ASD receive optimal care tailored to their specific needs and conditions.
Author Contributions
Rikesh Acharya: conceptualization, writing – original draft. Prashant Shah: conceptualization, writing – original draft, writing – review and editing, writing – review and editing. Ayurda Pradhan: writing – original draft. Sajjad Ahmed Khan: writing – original draft. Udip Yadav: writing – original draft. Sudhan Neupane: writing – original draft. Madhav Panthi: writing – original draft.
Acknowledgments
Authors are thankful to the department of cardiovascular medicine for providing the needful information. We express our gratitude to the patient's family members for their co-operation.
Consent
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
Data will be provided by the corresponding author upon reasonable request. Images uploaded in the separate files.




