Percutaneous Transluminal Angioplasty Balloon-Assisted Adjacent Vascular Connection Without Stent Protection: Case Report
Funding: This work was supported by Suzhou Kowloon Hospital Scientific Research Pre-research Fund (Project SZJL202303).
ABSTRACT
The aneurysmal dilation and excessive blood flow of the cephalic vein caused by the relative stenosis of the cephalic venous arch are important challenges in the maintenance of arteriovenous fistulas, and the use of adjacent vascular connection without stent protection has shown great advantages over traditional open surgery.
1 Introduction
Maintaining vascular access is essential for end-stage renal failure patients receiving hemodialysis; the arteriovenous fistula (AVF) is recommended because of its longer lifespan and reduced risk of infection [1, 2].
Hemodialysis patients facing vascular access difficulties may find that Percutaneous Transluminal Angioplasty (PTA) is a potentially effective option [3]. Reliable vascular access is necessary for hemodialysis in patients with end-stage renal illness, as high flow rates and repetitive cannulation can cause cephalic vein (CV) arch stenosis [4]. Surgical revision was the standard of care, which comes with hazards and long recovery periods [5]. PTA restores venous flow dynamics and rapidly dilates stenotic segments, providing a less intrusive option [6].
Complications related to hemodialysis access seriously affect the quality of survival of hemodialysis patients. In this case report, we present a female patient with a relatively narrow cephalic venous arch resulting in cephalic venous hemangioma formation and difficulty in stopping bleeding after dialysis. This case highlights a new interventional procedure: under ultrasound guidance, a subcutaneous sinus tract is formed using a vascular sheath, and the sinus tract is assisted in the formation of a proposed vessel by a balloon dilatation technique, thereby introducing cephalic venous flow into the median cubital vein to solve the problem. This operation still has limitation. The simulated blood vessels do not have real vascular tissue and may form stenosis or thrombosis again. We still need long-term follow-up and perform another balloon dilatation surgery if necessary, but it is still a meaningful attempt to simplify the solution to the problem of vascular access.
2 Case History
An effective treatment of PTA balloon-assisted neighboring vascular communication without stent protection was carried out on a 42-year-old female patient with stage 5 chronic renal disease and a complicated vascular access history. Eighteen years ago, she underwent arteriovenous fistula (AVF) placement in the left forearm, followed by kidney transplantation 16 years ago. Subsequently, due to rising creatinine levels 3 years ago, the AVF was ligated, and 2 years ago, dialysis access reconstruction was performed. In 2024–2003, the patient developed enhanced AVF pulsation, prolonged hemostasis after dialysis (> 1 h), and was accompanied by left neck traction discomfort. Physical examination showed that the patient had a high arteriovenous fistula near the elbow in the left arm, the cephalic vein was tortuous and dilated, and there was palpable tremor, the arm elevation test was positive, and there were no obvious varicose veins in the chest wall of the upper extremity. In order to solve the problem encountered by the patient, we considered traditional open anastomosis surgery or interventional surgery, traditional open anastomosis surgery has a clear effect but is more traumatic, but interventional surgery can relieve the high pressure of the cephalic vein through median venous shunt, which solves the problem and causes only minimal trauma.
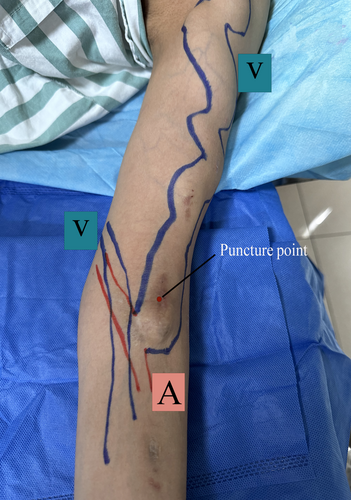
For the purpose of increasing the success of the operation and overcome the problem of blood extravasation that may occur during the operation, it is important to choose the appropriate puncture point and the route of vascular connection, so it is necessary to evaluate the direction of the patient's AVF before surgery, look for a short distance between the cephalic vein and the median elbow vein, and puncture the area of scar tissue formation.
3 Methods
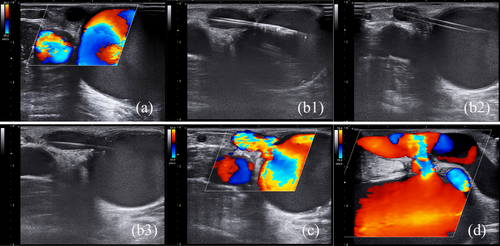
Preoperative vascular mapping (Figure 1) validated the accurate location of the puncture site at the distal end of the cephalic vein, which is essential for maximizing procedural planning and guaranteeing targeted intervention. Preoperative vascular flow exploration showed no blood flow connection between the cephalic vein and the median cubital vein (Figure 2a). The median cubital vein was then carefully opened by delicately inserting a vascular sheath (TERUMO6F-RS*A60K10SQ) through vessels in scar tissue and subcutaneous muscles. After the sheath was inserted, a drug-coated balloon (DCB, ACOTEC-Orchid 6F ORC07040A) extended the sinus tract and provided medicine, this effectively promoted vascular access patency and reduced endothelial proliferation (Figure 2b). Following surgery, a continuous ultrasound examination (Figure 2c) showed no discernible extravasation and continuing blood flow from the cephalic vein down the sinus tract to the median cubital vein. A significant pressure drop was found during the vascular access flow assessment, indicating better hemodialysis effectiveness and a lower risk of access-related problems (Table 1). Significantly, after surgery, there was a discernible drop in cephalic vein hemangiomas, In addition, the cephalic vein vascular resistance and peak flow velocity decreased significantly compared with before (Table 2), demonstrating the therapeutic effectiveness in treating vascular problems in this patient group. The successful resolution of vascular access challenges enabled the patient to undergo arteriovenous fistula (AVF) puncture the day after PTA dilation, facilitating the resumption of regular hemodialysis sessions. At the 1-month follow-up visit (Figure 2d), vascular ultrasound confirmed the structural integrity of the cephalic vein connected to the median cubital vein sinus, underscoring the durability and functional viability of the established vascular access site.
| VED (cm/s) | PSV (cm/s) | RI | PI | Qa (mL/min) | |
|---|---|---|---|---|---|
| Before | 62.3 | 121.0 | 0.48 | 0.71 | 1047.5 |
| 1 month | 77.0 | 119.2 | 0.35 | 0.45 | 1158.3 |
| 3 months | 80.7 | 128.3 | 0.37 | 0.46 | 1143.9 |
| VED (cm/s) | PSV (cm/s) | RI | PI | |
|---|---|---|---|---|
| Before | 189.8 | 250.4 | 0.24 | 0.27 |
| 1 month | 66.5 | 91.9 | 0.28 | 0.35 |
| 3 months | 20.2 | 31.2 | 0.35 | 0.38 |
4 Conclusion and Results
The patient underwent hemodialysis treatment through AVF puncture on the second day after interventional surgery, and the treatment was successful and discharged. One month after discharge, the patient was followed up again for the AVF, and there was no obvious bleeding observed in the sinus tract at the puncture site, and blood was successfully shunted from the cephalic vein to the median elbow vein, which reduced the excessive blood flow caused by cephalic vein arch stenosis, and the hemostasis after dialysis became simple. The successful application of percutaneous puncture to create an artificial sinus tract for diverting blood from the cephalic vein to the median elbow vein was confirmed by the patient's recovery and absence of complications. This case suggests that similar patients could use this approach to achieve effective drainage. However, it is crucial to emphasize the importance of strict adherence to sterile technique protocols and comprehensive patient monitoring throughout the treatment process to ensure patient safety. Maturate pre-procedural preparation and on-the-spot procedural modifications, depending on the patient's response and vascular dynamics, reduced the possible hazards of the innovative intervention. Patients undergoing hemodialysis may find a viable alternative in balloon-assisted adjacent vascular communication for addressing difficult vascular access issues. This technique effectively improves vascular access results by addressing important flow dynamics and hemostasis concerns, suggesting it may be a good substitute for conventional surgical procedures. The main goals of future studies should be validating these results in more significant cohorts and evaluating their long-term durability and cost-effectiveness.
5 Discussion
A case study demonstrating the effective use of PTA in the management of excessive cephalic venous blood flow without stent protection is presented in this paper. It assesses the viability of the procedure, the immediate results, and the long-term effectiveness of utilizing a drug-coated balloon (DCB) to create adjacent vascular contact between the median cubital vein (MCV) and the CV. This emphasizes the function of PTA in improving vascular access and lowering the consequences of CV arch stenosis. It not only solves the excessive cephalic vein flow caused by cephalic vein arch stenosis, but also connects the median elbow vein and the basilic vein, and the subsequent dialysis can puncture the blood vessels, replacing the traditional vascular transposition reconstruction with minimal trauma, killing two birds with one stone. PTA effectively improved vascular access for hemodialysis. The treatment successfully decreased hemangiomas, corrected tortuous dilatation, and controlled excessive blood flow, reducing the risk of bleeding problems during dialysis.
To maximize procedural success and patient safety, our approach required careful preoperative vascular mapping to pinpoint the puncture site exactly. The sinus tract can be expanded, and endothelial proliferation can be reduced using a trocar to connect the cephalic and median cubital veins and dilate with DCB [7]. This procedure significantly reduced the postoperative difficulties associated with traditional hemodialysis access techniques while simultaneously improving blood flow dynamics.
Continuous ultrasonography monitoring following surgery verified no appreciable extravasation and that blood continued to flow down the sinus tract to the median cubital vein. Evaluations of vascular access flow showed a substantial decrease in pressure, suggesting enhanced hemodialysis effectiveness. Also, the observed decline in cephalic vein hemangiomas confirms that DCB is a therapeutically effective treatment for vascular problems in this group of patients.
PTA balloon-assisted neighboring vascular communication without stent protection has shown encouraging results for managing hemodialysis difficulties in our patients with complicated vascular access issues. This innovative method successfully addressed problems frequently encountered by dialysis patients, such as substantial cephalic vein flow and challenges in attaining hemostasis.
It is essential to comprehend the efficacy of PTA in order to maximize hemodialysis results and care [8]. PTA may reduce the likelihood of thrombosis and infection in the future while preserving dialysis effectiveness by avoiding the implantation of stents [9]. This method offers a workable answer for patients with complicated vascular anatomy or those who would rather not have surgery.
Investigating novel approaches, like PTA, to treat CV arch stenosis and excessive venous flow indicates how interventional nephrology is developing [10]. This case study highlights the impact of PTA on enhancing patient quality of life and treatment outcomes and offers insightful information about how to apply PTA in renal care.
Author Contributions
Xiaoyi Sun: data curation, writing – original draft. Xiang Shao: methodology, validation, writing – review and editing. Weixin Kong: supervision. Hejing Liu: investigation. Xiang Li: writing – review and editing.
Acknowledgments
We are particularly grateful to all the people who have helped us with our article.
Consent
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.




