POEMS syndrome: A rare cause of ascites and pelvic effusion
Abstract
POEMS syndrome is a rare clonal plasma cell disease associated with multisystem involvement. We reported a case of 48-year-old woman with large volume of exudative ascites with an increased level of λ-light chain and hepatosplenomegaly. The patient was treated with thalidomide and dexamethasone and showed a good clinical response.
1 INTRODUCTION
POEMS syndrome is a rare paraneoplastic disorder secondary to an underlying plasma cell neoplasm, which is characterized by polyneuropathy, organomegaly, endocrinopathy, monoclonal protein, and skin changes.1 Peripheral neuropathy was present in almost all patients, while extravascular volume overload and other clinical features were present in some patients during the development of the disease. Given the rarity of POEMS syndrome, early identification and diagnosis is essential for treatment. Making the diagnosis of POEMS syndrome can be a challenge.
Here, we report this rare case of unexplained ascites and severe pelvic effusion. Our objective is to emphasize the importance of a holistic approach to analyze the multiple unexplained symptoms and signs.
2 CASE REPORT
A 48-year-old woman presented to the Gastroenterology Department with a 3-month history of worsening abdominal distention. She had weight loss. Six months ago, she developed progressive numbness and weakness in the lower limbs. Electromyography was requested and revealed a moderate to severe lesion of peripheral nerves of extremities, in which sensory disturbance was more serious than dyskinesia, and the lesions of the lower limbs was more pronounced than the upper limbs. Now, she was unable to walk and became a wheelchair user.
On examination, her vital signs were normal. She had no signs of jaundice, liver palms, spider angioma, anemia, edema, and lymphadenopathy. She was cachexic. Her hands showed skin pigmentation and the nails were slightly white. Her abdomen was grossly distended with a positive shifting dullness and fluid thrill. Neurological examination revealed normal cranial nerves and muscle force in upper limbs (5/5), however, there was significantly diminished power in the distal lower limbs (0/5), and a lesser extent in the proximal lower limbs (4/5). Extremities tendon reflex was absent. Sensation was diminished in both lower limbs, but the upper limbs examination was normal.
The blood biochemistry test revealed a high serum IgA (16.20 g/L, ref 0.7–4 g/L), λ-LC (4.78 g/L, ref 0.9–2.1 g/L), prolactin (1192.0 μIU/ml, ref 102–497 μIU/ml). The concentration and percentage of M-protein was 6.05 g/L (ref 0–0) and 9.9% (ref 0–0). The other blood tests showed no obvious abnormalities (Table 1). The ascites analysis revealed an exudative ascites (Table 1), and no tumor cells were detected by pathologic cytology twice. Furthermore, we detected the level of vascular endothelial growth factor (VEGF), which was slightly elevated, 252.01 pg/ml (ref 0–160 pg/ml).
| Parameters | Value (normal range) | Parameters | Value |
|---|---|---|---|
| Blood | Ascites | ||
| RBC | 4.46 × 1012 (3.5–5.0 × 1012/L) | Color | Yellow |
| Hemoglobin | 124 (113–151 g/L) | Character | Turbid |
| Hematocrit | 38.6 (33.5–45.0%) | Serous mucin | Positive |
| WBC | 6.74 × 109 (3.2–9.7 × 109/L) | Total cell count | 778 × 106/L |
| Platelet count | 296 × 109 (100–300 × 109/L) | White cell count | 528 × 106/L |
| CA125 | 61.30 (0–35 U/ml) | Mononuclear leucocyte | 60.0% |
| HE4 | 248.0 (0–104 pmol/L) | Polynuclear leucocyte | 40.0% |
| Creatinine | 100 (45–84 μmol/L) | Sudan III staining | Positive |
| Albumin | 36.0 (34–48 g/L) | TP | 41.0 g/L |
| Globulin | 29.8 (20–32 g/L) | Albumin | 25.3 g/L |
| Cholinesterase | 3332 (4290–10,520 U/L) | SAAG | 10.3 g/L |
| Direct bilirubin | 3.3 (0–6.8 μmol/L) | Glucose | 7.61 mmol/L |
| Indirect bilirubin | 9.2 (0–14.0 μmol/L) | LDH | 60 U/L |
| ALT | 18 (5–35 U/L) | ADA | 3 U/L |
| AST | 16 (8–40 U/L) | CL | 108.2 mmol/L |
| Ig A | 16.20 (0.7–4 g/L) | T-SPOT | Negative |
| Ig M | 1.07 (0.4–2.3 g/L) | TB-DNA | Negative |
| Ig G | 8.20 (7–16 g/L) | CA125 | 611.0 U/mL |
| κ-LC | 1.61 (1.7–3.7 g/L) | HE4 | 427.0 pmol/L |
| λ-LC | 4.78 (0.9–2.1 g/L) | CEA | 0.53 ng/ml |
| κ/λ | 0.34 (1.35–2.65) | ||
| pANCA | Negative | ||
| cANCA | Negative | ||
| MPO | Negative | ||
| PR3 | Negative | ||
| PRL | 1192 (102–496 μIU/ml) | ||
| Anti-HIV 1,2 | Negative | ||
| Glucose | 5.48 (3.89–6.11 mmol/L) | ||
| ANA | Negative | ||
| T-SPOT | Negative |
- Abbreviations: ADA, adenosine deaminase; ALT, alanine aminotransferase; ANA, antinuclear antibody; AST, glutamic oxalacetic transaminase; cANCA, cytoplasmic anti-granulocytic cytoplasmic antibody; LDH, lactic dehydrogenase; MPO, anti-myeloperoxidase antibody; pANCA, perinuclear anti-granulocytic cytoplasmic antibody; PR3, anti-protease 3 antibody; PRL, prolactin; RBC, red blood cell count; SAAG, serum ascites albumin gradient; TP, total protein; WBC, white blood cell count.
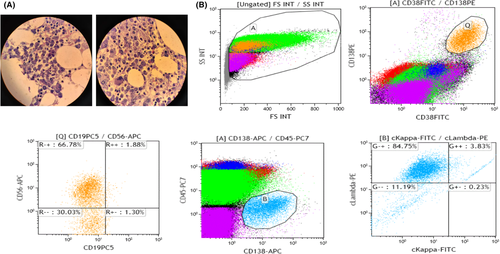
A CT scan of abdomen and pelvic showed hepatosplenomegaly, widened portal vein diameter, ascites, severe pelvic effusion with no intra-abdominal and retro-peritoneal lymphadenopathy (Figure 1). A PET/MR scan of whole body revealed a slightly higher signal intensity on T2WI and increased level of glucose metabolism at the anterior edge of the third thoracic vertebra (SUV max of 4.3) (Figure 1). Gastroscopy and colonoscopy showed no abnormalities. Fundus examination revealed bilateral retinal edema. Moreover, a bone marrow biopsy was obtained showing plasma tumor cells distributed in clusters, with different sizes of cell bodies, rich cytoplasm, purplish red, round and partial nuclei (Figure 2A). Flow cytometric of bone marrow revealed a population of abnormal plasma cells (0.9%), characterized with CD138+CD38+CD56+CD19−CD45−. The monoclonal expression of these abnormal plasma cells was λ-LC (Figure 2B).
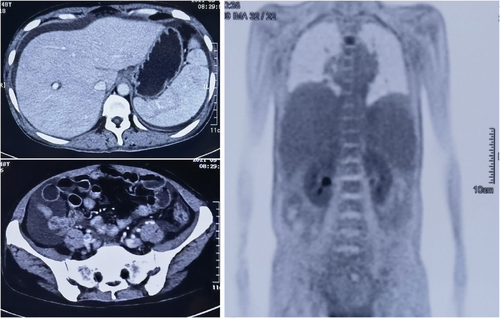
Exudative ascites and pelvic effusion raised the suspicion of common causes like malignancy, tuberculosis, microbial infections and autoimmune or connective tissue disease. On malignancy, the level of tumor marker CA125 and HE4 in both ascites and serum was increased, however, we did not find tumor cells in repeated cytological tests and no accessory space-occupying lesions was found in the CT scan and PET/MR. On tuberculosis, patients showed no symptoms of tuberculosis poisoning such as night sweats and the afternoon hot flashes, the T-SPOT and TB-DNA was negative in both blood and ascites, and the test for ascitic ADA was negative. On connective tissue disease, the serological test was negative.
The patient was given supportive therapy with abdominal drainage tube insertion to relieve her excessive ascites. Combined her presentation and the results of the tests, she was highly suspected as POEMS syndrome. She was given l-thyroxin for the hypothyroidism. The patient was transferred to the department of hematology and was treated with dexamethasone and thalidomide. She made good clinical response, and the ascites/pelvic effusion were effectively controlled.
3 DISCUSSION
We reported a rare case of POEMS syndrome in a patient who presented with unexplained large-volume ascites. Preceding this presentation, she had a diagnosis of peripheral neuropathy. The diagnosis of POEMS syndrome was often misdiagnosed by many clinicians due to its rarity in clinical practice and the complicated clinical manifestations. The disparate signs and symptoms must be linked to make accurate diagnosis.
POEMS syndrome (polyneuropathy, organomegaly, endocrinopathy, M-protein, skin changes) is a multisystem clonal disorder. The diagnosis of POEMS syndrome is based on a composite of clinical and laboratory characters, which requires the presence of both mandatory criteria (polyneuropathy and monoclonal plasma-proliferative disorder, almost always λ restricted), and at least one major criteria (sclerotic bone lesion, Castleman's disease and elevated VEGF) and one minor criteria (organomegaly: splenomegaly, hepatomegaly, or lymphadenopathy; extravascular volume overload: edema, pleural effusion, or ascites; endocrinopathy: adrenal, thyroid, pituitary, gonadal, parathyroid, pancreatic; skin changes: hyperpigmentation, hypertrichosis, glomeruloid hemangiomata, plethora, acrocyanosis, flushing, white nails; papilledema, and thrombocytosis).1 When patients had these clinical presentations of unknown cause including peripheral neuropathy, monoclonal protein, organomegaly, peripheral edema, skin changes, and unexplained ascites, POEMS syndrome should be taken into consideration.
Ascites is not a common first symptom of POEMS syndrome. In China, the sensorimotor polyneuropathy is the first common symptom in 60.44% patients,2 which is higher than that in Japan.3 The second common symptom is extravascular volume overload (15.72%), followed by endocrine abnormalities (9.87%), skin changes (8.05%) and organomegaly (2.13%). For POEMS syndrome, the ascites is typically exudative as the same with our patient. It is important to rule out other causes of exudative ascites, such as inflammatory, infective and malignant causes. In our case, the CT scan showed a widened portal vein diameter (1.5 cm), but the serum ascites albumin gradient was low, indicating non-portal hypertension. We also temporarily ruled out the tuberculosis, infection and tumor. Therefore, it is difficult to diagnose POEMS syndrome by ascites. Apart from ascites and pelvic effusion, our patient had a significantly high level of λ-LC. Monoclonal plasma cells (λ light chain restriction) were mandatory for the POEMS syndrome diagnosis. Serum immunoglobulin assay reveals a monoclonal protein for most patients.4
Raised circulating VEGF showed high sensitivity and specificity in the diagnosis of POEMS syndrome.5 The neo-angiogenesis and vascular permeability function of VEGF were correlated with some of clinical features of POEMS, like edema, pleural effusion, ascites, and papilledema. In fact, our patient did not show a “elevated” or “very elevated” of serum VEGF, which was lower than 1000 pg/ml. Our patient had a polyneuropathy of both lower limbs, a high serum IgA and λ-LC level, elevated serum VEGF, splenomegaly, hepatomegaly, skin changes, ascites and severe pelvic effusion. According to these features, the patient was diagnosed as POEMS syndrome.
The treatment of POEMS syndrome is comprehensive. Currently, the gold standard treatment is high-dose chemotherapy combined with peripheral blood stem cell transplant, which shows a good hematological control and clinical improvement.6 Moreover, melphalan/thalidomide/lenalidomide in combination with dexamethasone also show good clinical response.7-9
POEMS syndrome is a rare paraneoplastic disorder, which can affect multiple systems in the body. In fact, the characters of ascites alone in this case could not guide us to find the real cause. The analysis of disease by combining seemingly unrelated symptoms is important in diagnosing patients with ascites of unknown reason. However, the most important thing is to recognize this rare disease.
The key clinical significance of this report is to recognize, early diagnose this rare disease. A holistic approach to analyze the multiple unexplained symptoms and signs is important to make accurate diagnosis and differential diagnosis.
AUTHOR CONTRIBUTIONS
JM wrote the manuscript and revised drafts. YC wrote the first manuscript. XJQ analyzed and interpreted the patient clinical data. XGL analyzed and interpreted the patient clinical data. ECL and HJF followed up the patient. YDX: revised drafts. XW: revised subsequent drafts.
ACKNOWLEDGMENT
The authors thank the patient and her family members for their generosity and cooperation.
CONFLICT OF INTEREST
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
CONSENT
Informed written consent was obtained from the parents in this case report prior to submission regarding the publication of images and data.
Open Research
DATA AVAILABILITY STATEMENT
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.