Functional salivary reservoir in maxillary complete denture – technique redefined
Key Clinical Message
Complete dentures are poorly tolerated in patients with xerostomia. A salivary reservoir can be incorporated into a denture that provides slow, sustained, and continuous release of salivary substitute. This article describes a simple, cost-effective, and innovative technique of fabrication and designing of functional maxillary salivary reservoir complete denture.
Introduction
Oral cancer ranks the first among commonly occurring malignancies in India and majority of them are squamous cell carcinomas. The age-standardized incidence rate of oral cancer is reported as 12.6 per 100,000 population 1. Squamous cell carcinoma is usually radiosensitive and patients who receive radiotherapy to the fields involving the oral cavity experience various oral complications 2. Xerostomia is one such common complication after radiotherapy because salivary glands are highly sensitive to radiation. The changes in the salivary glands following radiotherapy include progressive fibrosis, loss of fine vasculature, and parenchymal degeneration. The degree of xerostomia is directly proportional to the radiation dose administered and the volume of salivary gland exposed to radiation 3, 4. Standard head and neck radiotherapy results in serious, often irreversible damage to the major and minor salivary glands.
Xerostomia is defined by the glossary of prosthodontic 5 terms as dryness of the mouth from lack of normal secretions. Xerostomia is a symptom, not a diagnosis or a disease. It is a subjective feeling of oral dryness. This term encompasses the spectrum of oral complaints voiced by patients with dry mouth 6. It disrupts the normal homeostasis of the oral cavity, leading to changes in the taste, difficulty in speech, difficulty in swallowing, and decreased dietary intake 7. These changes adversely affect the patient's health and overall quality of life 8. Moreover, the absence of saliva as a thin film between the dentures and the oral mucosa decreases retention of the dentures and increases inflammation and ulceration in the oral cavity. Hence, complete dentures are often poorly tolerated in patients with xerostomia 9.
Several treatment options are available to the clinician depending on the etiology of xerostomia. Most cases require symptomatic treatment and include changes in dietary pattern, patient counseling, lifestyle modifications, salivary stimulants, and use of salivary substitute. A salivary reservoir denture is an effective solution in edentulous patients with xerostomia to deliver salivary substitute constantly into the patient's mouth without affecting the normal routine 10. This article describes a simple and innovative technique for fabrication and designing of a functional maxillary salivary reservoir complete denture for a patient with xerostomia secondary to radiation therapy.
Case Report
A 60-year-old patient reported to the Department of Prosthodontics at Pushpagiri College of Dental Sciences for the replacement of missing teeth. The patient also complained of difficulty in swallowing and mastication and experienced difficulty in opening his mouth. The patient gave a history of radiation therapy 2 months back for focal keratinizing squamous cell carcinoma of left retromolar trigonal area. Prior to the radiation therapy, he had undergone total extraction of all teeth. He has a history of hypertrophic cardiomyopathy, had diabetes, and was under insulin therapy. Intraoral examination revealed erythematous spots and white patches on the palatal mucosa indicating incomplete healing of palatal mucosa following radiotherapy. The mouth opening was reduced, but it was within the normal range. Extraoral examination revealed diffuse enlargement in the submental region with local rise in temperature suggestive of submental lymph node enlargement. The patient was diagnosed as a case of radiation-induced xerostomia. The case was also discussed with the patient's consulting medical oncologist. The patient was instructed to perform active mouth opening exercises to improve the reduced mouth opening. A counseling process was also implemented which included dietary counseling, multivitamin supplements, and frequent drinking of water. The complete denture construction was delayed for 4 months to allow for natural healing of tissues and prepare the supporting tissues for prosthesis. The patient was asked to review every month. After 4 months, the mouth opening was improved but the symptoms of xerostomia persisted. The complications associated with radiation therapy and the importance of using a modified form of denture was explained to the patient. It was decided to construct a salivary reservoir complete denture in the maxilla containing salivary substitute to relieve xerostomia and aid the patient in the daily activities. This was well accepted by the patient.
Procedure
- Steps in fabrication of conventional complete denture are similar up to the try-in stage.
- Palatal contours are recorded using tissue conditioning material at the try-in appointment (GC Soft Liner, GC Corporation, Japan) (Fig. 1A).
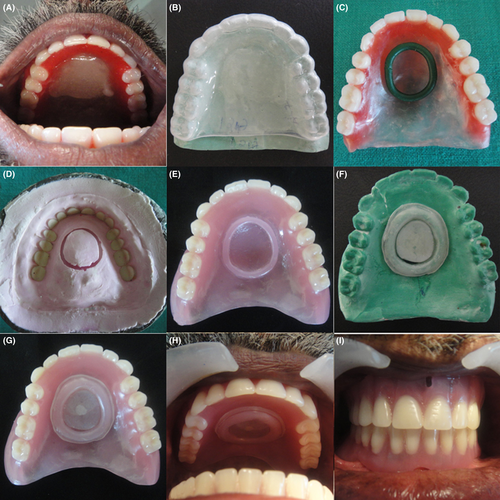 Figure 1Steps in fabrication of maxillary salivary reservoir complete denture. (A) Palatal contours recorded using tissue conditioning material at the try-in appointment. (B) Template of 1-mm thick thermoplastic material fabricated on working cast. (C) Wax-up of reservoir walls and lid rim with sprue wax. (D) Trial denture after dewaxing (view from the cope of flask). (E) Finished and polished complete denture with reservoir walls and lid rim on the palatal aspect of the denture. (F) Reservoir lid fabricated with 2-mm flexible thermoplastic sheet on duplicated cast of the denture. (G) Polished surface of maxillary salivary reservoir complete denture with salivary substitute. (H) Intraoral view of maxillary salivary reservoir complete denture with salivary substitute. (I) Intraoral view of complete dentures in occlusion.
Figure 1Steps in fabrication of maxillary salivary reservoir complete denture. (A) Palatal contours recorded using tissue conditioning material at the try-in appointment. (B) Template of 1-mm thick thermoplastic material fabricated on working cast. (C) Wax-up of reservoir walls and lid rim with sprue wax. (D) Trial denture after dewaxing (view from the cope of flask). (E) Finished and polished complete denture with reservoir walls and lid rim on the palatal aspect of the denture. (F) Reservoir lid fabricated with 2-mm flexible thermoplastic sheet on duplicated cast of the denture. (G) Polished surface of maxillary salivary reservoir complete denture with salivary substitute. (H) Intraoral view of maxillary salivary reservoir complete denture with salivary substitute. (I) Intraoral view of complete dentures in occlusion. - The trial denture with its modified palatal contours is duplicated in alginate (Ruthinium Alginate, Ruthinium Dental Products Pvt. Ltd., India) and a working cast is poured in Type III Dental Stone (Goldstone, Asian Chemicals, India).
- A template of 1-mm thick thermoplastic material (BIOPLAST®, India) is fabricated on this working cast which serves as a guide for salivary reservoir designing (Fig. 1B).
- The tissue conditioning material on the palatal surface of the trial denture is removed. The reservoir walls and lid rim are built with sprue wax (3 mm YETI Dentalprodukte GmBH, Germany) (Fig. 1C). A slight undercut must be created on the inner aspect and a groove is made on the external surface of the lid rim using a Le Cron carver. These two features facilitate attachment for the flexible lid of the reservoir. The reservoir volume must be assessed at this stage by injecting a known quantity of liquid using a calibrated syringe.
- The trial denture is waxed-up, invested, and processed in the conventional manner (Fig. 1D).
- The denture is finished and polished (Fig. 1E) and then duplicated using alginate to obtain a second working cast made of Type III Dental Stone (Goldstone, Asian Chemicals, India).
- The reservoir lid is fabricated with a 2-mm flexible thermoplastic sheet (BIOPLAST®) on the second working cast of the denture (Fig. 1F). The reservoir space must be blocked out with the help of plaster, while the undercut on the inner aspect of the reservoir lid rim must be relieved before fabricating the reservoir lid.
- A 0.8-mm release hole is made on the most dependent portion using a straight fissure bur. This permits the slow and continuous release of the salivary substitute.
- The reservoir lid is snapped to close the reservoir and is filled with salivary substitute (methyl cellulose – wet mouth, ICPA) using a calibrated syringe through the release hole (Fig. 1G). The salivary substitute is released when the tongue creates pressure in the anterior portion of the palate.
- The functional maxillary salivary reservoir complete denture is ready to be inserted (Fig. 1H and I).
Instructions to the patient
- Postinsertion instructions were given to the patient regarding oral and denture care.
- The patient was instructed about the cleaning of the reservoir and the lid using soft bristled toothbrush and toothpaste.
- The patient was instructed about refilling the reservoir with salivary substitute with due care.
- The patient was asked to make a conscious effort to consume at least eight glasses of water, lemon juice, or milk.
- Postinsertion check up was scheduled on the next day and regular recall visits were planned every month.
After a 6-month follow-up, the treatment was found to be satisfactory as the patient has found a great reduction in the symptoms of xerostomia and found it easy to use and clean the denture.
Discussion
Many patients who undergo treatment for oral cancer receive a course of radiation therapy. The prevalence of postradiation xerostomia is reported to be 90% 11. Xerostomia creates an unhealthy oral environment and can also cause or exacerbate a painful oral condition. The dental professional must recognize the seriousness of these complications and continue efforts to alleviate them.
Depending on the etiology of xerostomia, various treatment options are available. However, a combination of methods is often employed to make prosthesis successful. The goal in management of xerostomia is to reduce the suffering from the disease and to help the patient to use the denture and perform normal oral functions comfortably.
Complete dentures are poorly tolerated by patients with diminished salivary flow because of the lack of saliva bonding between the interface of the prosthesis and the oral/gingival tissues 12-17. The reservoir denture containing salivary substitute offers clinician an alternative method of treating patients suffering from xerostomia 18, 19 with a slow, sustained, and continuous release of salivary substitute. Artificial salivary substitutes can be classified into carboxymethyl cellulose-based and mucin-based salivary substitutes. Commercially available saliva substitutes containing carboxymethyl cellulose are the most commonly used as they are less costly and readily available. A number of artificial salivary substitute available in the market include Wet Mouth, Saliveze, Salivart, Moi-Stir, and Salix.
Several authors have recommended many approaches to fabricate reservoir dentures with available space in either the maxillary denture or the mandibular denture.
Mendoza and Tomlinson 20 described split-denture technique for artificial saliva reservoir in the mandibular denture, which was split into upper and lower parts. The laboratory stages were time-consuming in this technique. Similar methods were used by Dabas et al. 21 and Hallikerimath and Jain 22.
Burhanpurwala et al. 23 described a method for fabricating mandibular reservoir denture, but still the laboratory steps were complicated.
Sinclair et al. 24 used cobalt samarium magnets to connect the lower and upper part of the mandibular reservoir denture. Although he succeeded in providing a reservoir with a maximum capacity, the procedure required exhaustive laboratory steps. He has outlined a criteria for fabrication of salivary reservoir denture which includes maximum space for the reservoir, minimum adjustments in the finished denture so that a maximally extended reservoir would not be perforated and provide easy cleaning, and refilling the reservoir. Reservoir denture fabricated by our technique fulfilled all these criteria.
The methods advocated for incorporating reservoir space in mandibular complete denture are costly, time-consuming, and require exhaustive laboratory steps.
Toljanic and Zucuskie 25 described the use of salivary reservoir in the maxillary denture in patients with xerostomia. Its advantages over a reservoir in the mandibular denture includes larger reservoir size, provides flow of saliva to the whole mouth unlike mandibular reservoir where flow is restricted to the floor of the mouth, and do not block the outlet holes by fluid and food in the floor of the mouth. However, incorporating reservoir in the maxillary denture leads to increase in weight, which may affect its retention and stability.
Hirvikingas et al. 26 used a Gerber attachment to operate the release mechanism for the salivary substitute in the maxillary reservoir complete denture. Disadvantage of this technique is that the precision attachment increased the cost of the treatment.
Disadvantages of above methods were overcome in our method. The advantages and disadvantages of this technique in comparison with conventional methods of fabrication of salivary reservoir complete denture are outlined below.
Advantages
- Simplified technique.
- Cost-effective.
- Laboratory procedures are less time-consuming.
- No additional clinical steps.
- Physiologic mechanism of salivary release.
- Easy to use, clean, and refill the reservoir.
- Sustained and slow release of salivary substitute.
- Does not interfere with normal oral functions.
- Easy visibility of salivary substitute in the chamber.
- Easy accessibility to the reservoir by the dentist and patient
- Reservoir is less bulky compared to the conventional techniques.
Disadvantages
- Additional laboratory steps.
- The patient should manually refill the reservoir at regular intervals.
- High degree of precision is mandatory to ensure accurate and smoothly fitting the reservoir lid.
The volume of reservoir by this technique was 3 mL for a working duration of 2 h. The highlight of this technique used here is that it allows fabrication of a prosthesis that makes swallowing a control mechanism for the flow of salivary substitute. As the patient swallows, the tongue contacts the anterior portion of the palate and hence the thermoplastic membrane. This creates positive pressure inside the reservoir thus pushing the salivary substitute out of the outlets. Then, the pressure is relieved, air is sucked in creating a negative pressure, and the next cycle starts 27.
The tissue conditioner material is used to locate the position of the reservoir on the palate without interfering with the phonetics of the patient 28. The material is thicker in the anterior portion and vault of ridge thinning down to feather edge on the posterior border to make posterior border of reservoir discernible to tongue. The overall thickness of the palate was not affected with this design.
Although our technique has a definite advantage over other techniques, it cannot be used in cases with high palatal vaults. In case of repair or replacement of the lid, the patient or clinician can preserve the working cast which can be used readily for the lid fabrication.
Conclusion
This article reports a simple and innovative technique for the construction of functional salivary reservoir in maxillary denture. Xerostomic patients wearing prosthesis can benefit immensely from this as it will enhance the oral health and quality of life of such patients. Prosthodontists are first-line health care providers to treat such patients with artificial salivary reservoir prosthesis. To meet patient's functional and esthetic demands, a thorough knowledge and understanding of different saliva reservoir designs, and the merits and demerits of each design are essential. Case selection is important. Before fabrication of a removable prosthesis is started, the oral tissues should be ascertained that the denture bearing tissues will accept and support the prosthesis in comfort 29. Further research should be directed toward developing more physiologic salivary substitutes. However, this simple and innovative technique for fabrication and designing of functional maxillary salivary reservoir complete denture has proved to be successful and is helpful to both the dentist and patients in the management of xerostomia.
Conflict of Interest
None declared.