The challenge in diagnosing cardiac tumors to avoid unnecessary cardiac surgery
Abstract
Cardiac magnetic resonance in cardiac mass: Cardiac magnetic resonance (CMR) should be considered in the evaluation of patients with cardiac mass. Especially, when the diagnosis is not certain, CMR could provide paramount information that could be helpful for the decision on cardiac surgery.
1 INTRODUCTION
Diagnostic evaluation of cardiac tumors and the decision on cardiac surgery remain a clinical challenge. No international consensus document exists on diagnostic evaluation or treatment strategy in patients with cardiac masses. With an incidence of 0.001%-0.03%, primary cardiac tumors are rare even in a major cardiac surgery center.1, 2 When a cardiac mass is discovered, further clinical assessments, choice of imaging modalities, and treatment strategy are generally decided based upon local expert opinion.
Since its entry into the medical field, echocardiography has been the primary imaging technique in the assessment of cardiac tumors.3 Additional imaging modalities, including cardiac magnetic resonance (CMR), might give crucial information in diagnostic evaluation of cardiac masses.
2 CASE PRESENTATION
A 67-year-old female without previous cardiac history was admitted with palpitations. Prehospital electrocardiogram showed regular supraventricular tachycardia at a ventricular rate of 213 bpm. On suspicion of reentry tachycardia, intravenous Adenosine was given at a dose of 6 mg and after few minutes, further 12 mg was given without achieving conversion to sinus rhythm. Based on the presence of flutter waves during the transient AV block, the diagnosis of atrial flutter was made. Conversion to sinus rhythm was obtained by intravenous administration of 300 mg Amiodarone. Transthoracic echocardiogram (TTE) showed a solid mass of 5 × 3 cm in the right atrium attached to the intra-atrial septum. Transesophageal echocardiogram (TOE) showed no affection of the tricuspid valve. No hemodynamic obstruction of the atrial cavity, inferior, or superior caval veins were present (Figure 1 panel A, and Video S1-S2). Left ventricular function, right ventricular function, and all heart valves were without pathological findings. The tumor was suspected to be a right-sided myxoma, and the patient was referred to cardiothoracic surgery. There was no evidence of embolic phenomena. The SVT was concluded to be the first and single symptom of the tumor, knowing that the episode of SVT might not be necessarily related to the cardiac mass.
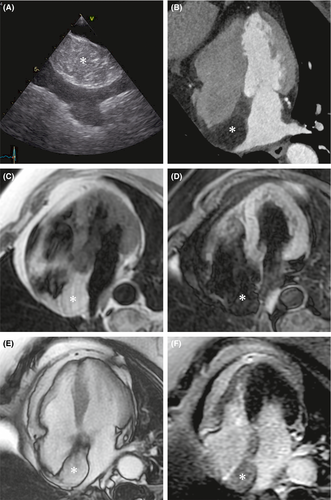
To rule out the presence of coronary stenosis prior to cardiothoracic surgery, cardiac computed tomography (CT) was performed, showing normal coronary arteries. Second review of the echocardiographic images at the heart team conference drew attention to the tumor's broad-based attachment to the intra-atrial septum, reduced mobility and absence of a narrow stalk. CMR was requested. CMR with T1- and T2-weighted images including fat suppression and gadolinium-based contrast revealed that the solid mass consisted of widespread lipomatous atrial septum hypertrophy (LASH) due to fatty infiltration. The tumor had a classic dumbbell shape with sparing of the fossa ovalis (The findings on echocardiography, CT, and CMR are showed on Figure 1, panel A-F, and Video S1-S3). The scheduled surgery was cancelled. Due to intermittent episodes of atrial fibrillation and assumed atrial flutter at the beginning of the hospital admission, the patient started oral anticoagulation therapy and treatment with a beta blocker. Radiofrequency ablation was considered, although refrained from due to the expected unacceptably high risk related to the massively thickened intra-atrial septum.
At the eight months control, the patient was in good condition and did not have any further episodes of palpitations. A new TTE showed unchanged findings without growth of the cardiac mass. Further clinical and TTE control is planned to assess whether LASH grows and whether the patient eventually develops any cardiac symptoms that may alter the decision of no surgery.
3 TIMELINE
| Day 1 | Admission to cardiac unit with palpitations. Regular supraventricular tachycardia at 213 bpm. Transient AV block induced by Adenosine showed flutter waves. Conversion to sinus rhythm by intravenous administration of 300 mg Amiodarone. |
| Day 2 | Stable condition. Initiation of treatment with beta blocker. |
| Day 3-5 | Transthoracic echocardiogram (TTE) shows a solid mass 5 × 3 cm in the right atrium. Transesophageal echocardiogram gives suspicion of myxoma. Referred to cardiac computed tomography (CT) to exclude coronary artery disease. Discharge from hospital. |
| Day 17 | Cardiac CT shows normal coronary arteries. Referred to cardiac surgery. |
| Day 24 | Heart team conference: Doubt about the diagnosis myxoma. Referred to cardiac magnetic resonance (CMR) prior to surgery. |
| Day 45 | CMR with T1- and T2-weighted images including fat suppression revealed widespread lipomatous atrial septum hypertrophy due to fatty infiltration. |
| Day 57 | Conference with electrophysiologist: decision on avoiding radiofrequency ablation and continuing medical treatment for SVT. Initiation of anticoagulation. |
|
Day 207 (8 mo after admission date) |
Stable condition. No episodes of palpitations. New TTE: unchanged findings without growth of the cardiac mass. Follow-up clinical and TTE control is planned. |
4 DISCUSSION
4.1 Lipomatous atrial septal hypertrophy
LASH is thickening and hyperplasia of the intra-atrial septum and is defined by non-encapsulated hyperplasia of normal fat in the septum with a diameter >2 cm.4 LASH is associated with older age, female sex, coronary artery disease, and obesity.5-7 It was first described at a postmortem examination in 1964.6 Typically, LASH is an incidental finding on autopsy.8 Currently, the condition is detected more often in living patients because of more frequent use of noninvasive imaging. LASH is usually asymptomatic and requires no treatment. If obstructive symptoms are present, for example, congestive heart failure due to obstruction of the superior vena cava, surgical removal might be preferred. Previous studies have described an association between LASH and SVT due to the localization close to the conduction system connecting sinoatrial and atrioventricular nodes.6
It is important to distinguish LASH from lipomas since the choice of treatment is generally different. Lipomas and LASH are related by the tissue composition and arise from benign neoplastic proliferation of mature adipocytes.9-11 In contrast to LASH, lipomas are usually enclosed in a capsule and grow neoplastic.12 Lipomas can have both epicardial and endocardial localizations.3, 13-15 Endocardial lipomas are broad-based, without a narrow stalk, and tend to grow into the neighboring chamber. If lipomas are epicardially located, they are presented with a narrow stalk and grow into the pericardial space.
An important question in our case arises, how certain is the diagnosis of LASH based on noninvasive imaging only. It is generally accepted that LASH can be safely diagnosed by noninvasive imaging methods if the typical feature with a “dumbbell” configuration with sparing of the central fossa ovalis and a fatty component is identified by CMR.12 The second question is whether the SVT was associated with LASH. The risk factors associated with LASH are also those associated with atrial fibrillation, for example, aging and obesity. More studies are needed to clarify whether there is an independent association between LASH and the occurrence of SVT. However, in an elderly patient with obesity, an atrial arrhythmia might be associated with LASH if no other causative conditions are present, for example, valvular heart disease or heart failure. Thus, in our patient, it is not unlikely that the SVT was associated with LASH.
4.2 Cardiac imaging in evaluation of cardiac tumors
Approximately 75% of primary cardiac tumors are benign, with 50% of them being myxomas.2, 16 The remainder consists of papillary elastomas (20%), lipomas (15%-20%), and hemangiomas (5%). Around 25% of primary cardiac tumors are malignant, the majority of them being sarcomas (95%) and less frequently lymphomas (5%). Metastases to the heart and pericardium (secondary cardiac tumors) are 100-1000 times more frequent than primary tumors.10
Because of its availability, TTE is the imaging technique of choice, but it is heavily operator-dependent. In addition, the restricted field of view and the patient´s body habitus can affect the complete assessment of the cardiac mass. TOE permits a more detailed characterization of a cardiac tumor in terms of size, morphology, attachment site, extension, valvular lesions, and hemodynamic effects.
Nevertheless, neither TTE nor TOE provides sufficient tissue characterization or distinction between benign and malignant tumors. While preoperative biopsy is performed in some cases, this intervention is accompanied by a risk of complications such as embolization and hematogenous dissemination with aggravating consequences for the patient, especially if the tumor is located on the left side of the heart.17
Computed tomography can provide important additional information not readily available with echocardiography, in particular, on exact anatomic localization of the tumor, determination of any local invasion or extension into adjacent organs, and presence of coronary calcification (unlike CMR). Limitations of CT include the exposure to ionizing radiation, lower temporal resolution compared with echocardiography or CMR, and lower soft-tissue contrast resolution compared with CMR.10
Advantages of CMR when compared to echocardiography are larger field of view, better tissue characterization based on typical tissue signal intensities, exact anatomic description of the tumor, lack of attenuation and ability to image at any prescribed plane.18 The main limitation of CMR when compared to echocardiography is lower temporal resolution. Therefore, CMR is generally not suitable for the evaluation of valvular vegetations.12 Table 1 shows anatomic features and imaging characteristics of LASH, myxoma, and lipoma. Diagnostic evaluation of these three types of masses can be difficult because of their similarities. However, the anatomic location together with information on whether the mass is well defined, presence of a capsule, and appearance on CMR images might lead closer to the diagnosis.
| Anatomy | Echocardiography | CMR: T1 weightinga | CMR: T2 weightinga | CMR: LGE | |
|---|---|---|---|---|---|
| Myxoma | Arises from the interatrial septum near fossa ovalis. |
The majority (75%-80%) originate in the left atrium. Heterogeneous mobile mass. Attached to the atrium by a narrow stalk. |
Isotense | High | Heterogeneous uptake |
| LASH | Thickening of intra-atrial septum >2 cm. Sparing of fossa ovalis. | Broad-based attachment to the intra-atrial septum, sparing of fossa ovalis, immobile | Highb | Highb | No uptake |
| Lipoma |
Encapsulated. Broad-based. |
Broad-based, immobile, without a pedicle, well circumscribed. Hyperechoic. |
Highb |
Highb | No uptake |
When a cardiac mass has characteristic features of a certain cardiac tumor, CMR might not be necessary to make a diagnosis. When the cardiac mass causes hemodynamic complications, urgent surgery might be performed and additional imaging modalities such as CMR might cause delay in the treatment. When surgery is performed, a precise histological diagnosis will be present afterwards. Thus, additional CMR might be useful in situations where the diagnosis is not clear after echocardiographic examinations.
In conclusion, a team-based approach might be favorable in the diagnostic evaluation of patients with cardiac masses. Application of several imaging modalities might improve the diagnostic evaluation prior to decision on cardiac surgery.
5 PATIENT PERSPECTIVE
We suggest that patients with cardiac masses undergo evaluation in a team-based approach. We suggest that colleagues from other specialties such as cardiothoracic surgery, radiology, and oncology are involved in an early phase in the diagnostic evaluation. CMR could be a supplemental examination before the final decision on surgery to clarify the anatomic and functional changes. Furthermore, we suggest that the international cardiology societies establish a consensus document on assessing patients with cardiac masses.
ACKNOWLEDGMENTS
We want to thank Dr Niels Holmark Andersen, Department of Cardiology, Aalborg University Hospital, for the transesophageal images. Published with written consent of the patient.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTIONS
GJ and TZ: conceived the idea; GJ: directed and planned the study, performed literature search, wrote the manuscript, made revisions, and submitted the manuscript; MZ: examined the patient and obtained the informed consent from her; JG: is thoracic surgeon and participated in the discussion of the patient on the heart team conference; TZ: analyzed the CMR images, provided the presented images, and provided critical feedback to GJ in the description of the imaging modalities; all authors provided critical feedback on the manuscript.