Wael's surgical treatment of intestinal gangrene due to congenital internal hernia: A case report and review of literature
Abstract
A high clinical sense of the surgeon is mandatory in unstable deteriorating patients. Usually, a definitive diagnosis through an urgent laparotomy for repair of transmesenteric hernia and resection of gangrenous bowel leads to a successful outcome.
1 INTRODUCTION
An internal hernia is a protrusion of intestines through intra-abdominal mesenteric defect that is formed in a congenital or acquired pathway.1 Although it is reported in the pediatric surgical field, in adults it is a rare cause of intestinal obstruction. Transmesenteric type is the commonest type suspected in trauma or postoperative status and considered as a potentially lethal form of internal hernia, with 45% of overall mortality associated with acute intestinal obstruction.2, 3 The urgent surgical intervention must be in patients with complicated intestinal obstruction. In our clinical practice, we report a 25-year-old man who presented with abdominal pain, fever, hypotension, guarding tenderness, abdominal rigidity and signs of peritonitis. Due to his deteriorated status, the CT scan of the abdomen was not performed. After resuscitation, the patient was planned for exploratory laparotomy and required emergency intestinal resection because of internal mesenteric hernia involving widespread nonviable small and large intestines. It is quite challenging, and it is difficult to decide if re-anastomosis of gastrointestinal loops needs a protective stoma or not. We reviewed the presentation, diagnosis, surgical treatment and prognosis of internal mesenteric hernia.
2 CASE PRESENTATION
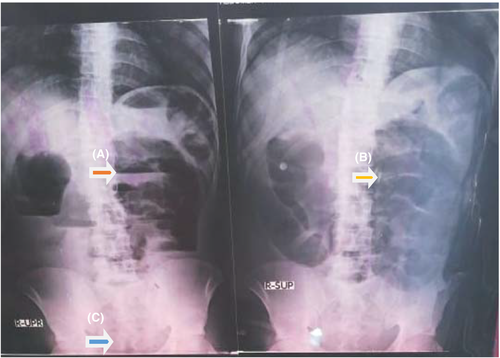
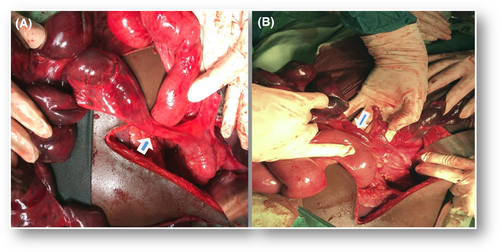
A 25-year-old male patient presented to the emergency department of our hospital with a 3-day history of sudden severe generalized colicky abdominal pain started all over the abdomen, then increased in intensity at the periumbilical area. The pain increased in severity by eating and reduced by fasting and associated with nausea, frequent vomiting and constipation. The systematic review, past medical history, family and psycho-social history including relevant genetic information were unremarkable. The physical assessment showed a conscious distressed patient with pale conjunctiva. On his arrival, the vital signs were as follows: heart rate 105 beats/min, blood pressure 100/60 mm Hg, the oral temperature reached 38°C and respiratory rate 32 breaths/min. Abdominal examination revealed marked abdominal distention, guarding tenderness mainly in the periumbilical quadrant, generalized abdominal board-like rigidity and no stool, masses or blood were felt on digital rectal examination. The laboratory findings on initial presentation were as follows: creatinine (0.7 mg/dL), urea (25 mg/dL), Na+ (136 mmol/L), K+ (4.2 mmol/L), WBC count (21 500 cell/mm3), hemoglobin (14 g/dL), platelets (243 000 per microliter of blood), RBS (151 mg/dL) and INR (1.7). The CT scan of the abdomen was not performed due to the patient being hemodynamically unstable and after resuscitation, plain abdominal X-ray was requested that showed multiple air-fluid levels, dilated intestinal loops and absent rectal gas (Figure 1). Emergent exploratory laparotomy showed black gangrenous dilated jejunal loop and sigmoid colon, absence of mesenteric pulsation and intestinal peristalsis in addition to the atrophied ischemic terminal ileum. These loops were entrapped through a 6 × 4 cm mesenteric defect located in the root of small bowel mesentery with 700 mL of reactionary peritoneal fluids (Figures 2 and 3).


2.1 Surgical intervention was done in three steps
A) Meticulous gentle reduction of gangrenous dilated sigmoid colon, jejunal and ileal loops from the defect into their normal anatomical position followed by resection of all nonviable segments of ileum and jejunum up to viable 70 cm from dudeno-jejunal junction. Because of the ischemic terminal ileum, right hemicolectomy was performed (Figures 4 and 5). Primary jejuno-transverse colonic end-to-end anastomosis was done successfully (Figure 6).

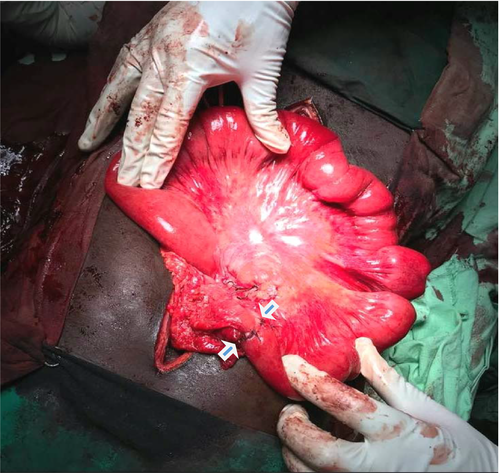
B) Sigmoid colectomy was performed from viable mid-descending colon below the left colic artery down to the recto-sigmoid junction. Hartmann's procedure was done with the complete repair of the mesenteric defect. Postoperatively, the patient spent 4 days in surgical ICU and 6 days in the surgical ward for regular follow-up of his vital signs, wound dressing and colostomy care. Then, the patient was discharged in good condition on the eleventh postoperative day.
C) Three months later, the patient was planned for a reversal of colostomy and supported by good nutrition and electrolytes intake to become fit for surgery. Under general anesthesia, laparotomy began with the surgical separation of the viable colonic end from the anterior abdominal wall. Then, we found accidentally the remained viable jejunal segment increased in length up to 150 cm. After that, in a proper hemostatic way the remaining part of the transverse colon was fully separated from the stomach, the spleen and the pancreas. Meticulous mobilization of colonic end down to the pelvic cavity was accompanied by careful dissection of the left colic artery from its mesentery. The viable rectal stump was identified and a careful dissection from its surrounding fibrous tissues to be mobilized with a good length which met a colonic end in a good opposition and tension free for the performance of end-to-end colorectal anastomosis successfully. Two drains were inserted. Wounds of laparotomy and previous colostomy were closed in layers. The patient spent 2 days in ICU and 6 days in the surgical ward for follow-up and conservative treatment of ileus and wound infection with regular dressing and intravenous antibiotics as results of antimicrobial susceptibility test. Finally, the patient was discharged in an excellent condition on the ninth postoperative day (Figure 7).

3 DISCUSSION
The internal mesenteric hernia is a rare malformation representing about 0.2%-0.9% of all small bowel obstruction cases.4 Other studies showed internal hernia in <1% of autopsy and it caused small bowel obstruction in 5.8% of the patients.5, 6 Transmesenteric hernia is the commonest type found in 8% of patients. The pathogenesis is uncertain. Treves in 1885, emphasized the weakest area in terminal ileum mesentery circumscribed by the ileocolic artery and its last ileal branch.7, 8 Another study found prenatal intestinal ischemia leads to thinning of the mesenteric leaves associated with bowel atresia in 5.5% of cases.7 There is a genetic association between transmesenteric hernia and anomalies including Hirschsprung disease and cystic fibrosis.3 Ghahremani divided internal abdominal hernia into two types: The congenital type is more common in pediatric cases while acquired type more common in adults caused by Roux-en-Y anastomosis creation as performed in hepatic transplantation or bariatric gastric bypass.9, 10 Another classification divided internal hernia into a retroperitoneal and congenital hernia. Moreover, retroperitoneal hernias were subdivided into paraduodenal, Winslow's foramen, paracecal and intersigmoid (30%-53%, 8%, 6% and 5%, respectively). Also, congenital hernias are divided into transmesenteric, broad ligament and transomental (5%-10%, 4%-7% and 1%-4%, respectively).11 Small bowel loops were the most common herniated organ followed by the sigmoid colon.12 Transmesenteric hernia complicated by volvulus and strangulation reported in 30% and 40%, respectively. This result from small defect aperture (2-5 cm) and absence of herniated loops encapsulation which permits the large length of small bowel through this mesenteric defect with high mortality rate reached up to 100% if exploration was delayed.13, 14 There are difficulties in preoperative diagnosis, due to no specific laboratory or radiological findings were available to confirm the diagnosis. This reason prompted researchers to seek for early diagnostic biomarkers of bowel gangrene.15 D-lactate is the normal end-stage of anaerobic breakdown of glucose in the tissues. The normal value of serum D-lactate is nano- to micromolar range. Thus, the elevation is almost pathological detected in postintestinal ischemia/strangulation due to abnormal proliferation of enteral flora from mucosal injury.16, 17 There were some studies evaluated the promising clinical value of D-lactate measurements in patients with acute abdomen and concluded an improvement in the diagnosis of acute intestinal ischemia.18, 19 Also, another study revealed an increased values of serum D-lactate in patients had strangulated bowel obstruction.20 Unfortunately, rarely D-lactate levels raised during the early phase of intestinal ischemia. Later at 43 hours, peaked D-lactate measurements were noticed and can persist for 2 days indicated pending poor outcome. Moreover, in a preoperative emergency setting of the developing countries and postoperative follow-up, the biomarkers were not assessed with regard to clinical diagnosis of strangulation due to the high cost and unavailability of the D-lactate test.21, 22 Contrast CT scan of the abdomen has an essential role in diagnosis and surgical planning in hemodynamic stable patients which showed common indicators including engorgement, crowding, twisting, or stretching of mesenteric vessels. Hence, a high clinical sense of the surgeon is mandatory in unstable deteriorating patients. Usually, a definitive diagnosis through an urgent exploratory laparotomy to reduce the hernia, mesenteric defect repair and resection of gangrenous bowel with anastomosis leads to a successful outcome with a reduction of the mortality rate down to 50%.3, 10, 13, 14, 23
4 CONCLUSION
In the absence of previous surgical history, the internal mesenteric hernia can be included in the differential diagnosis of intestinal obstruction. Perfect clinical assessment of nonspecific abdominal pain especially in a virgin abdomen is essential for early surgical intervention and optimal outcome. Furthermore, any obstruction in loops of the small bowel and colon end with strangulation necessitating resection and if accompanied with the colostomy procedure, the surgical outcomes become better than the ileostomy choice. Finally, the main strength of this case is applicability of our surgical treatment in an emergency setting of the developing countries in unstable deteriorating patients and where availability of CT scans and expensive serum biomarkers is beyond the reach of poor patients.
ACKNOWLEDGMENTS
The authors really would like to thank their colleagues in the surgical department for their kind suggestions and unlimited support.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
AUTHOR CONTRIBUTIONS
WMD: is responsible for original manuscript writing, editing, supervision and critical revision of contents. WMD, JAE and MOO: are responsible for data collection, data analysis and manuscript design. JAE, AMM and MSA: are responsible for manuscript drafting and revision. All authors read and gave the final approval of the manuscript to be published.
ETHICAL APPROVAL
This case report has been approved ethically by our institution.
CONSENT FOR PUBLICATION
The authors state that they have written and signed consent from the patient to publish this case report and any accompanying images. A copy of the written consent is available for review by the editor of this journal.