Henoch–Schönlein purpura with preceding abdominal pain
Key Clinical Message
Diagnosing HSP can be difficult, especially when abdominal symptoms precede the onset of characteristic palpable purpura (Chen MJ et al. 2005, World Gastroenterol., 11, 2354). Therefore, it is necessary to consider the possibility of HSP in patients with prolonged strong abdominal pain, even in cases without purpura.
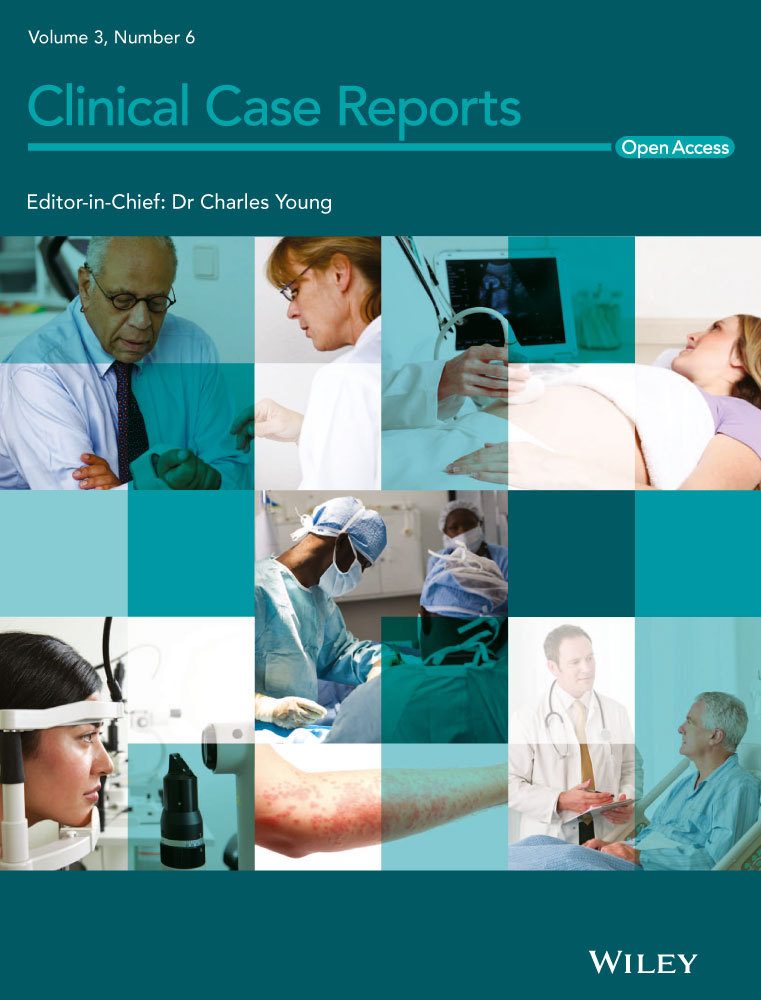
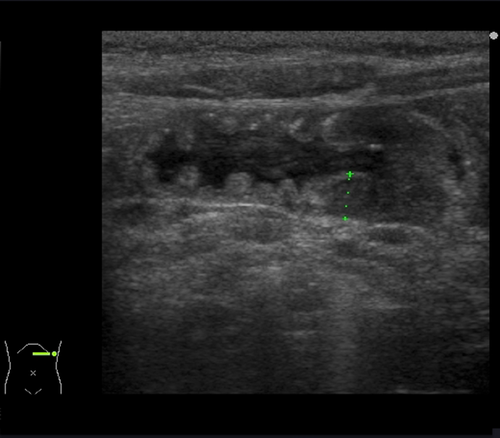
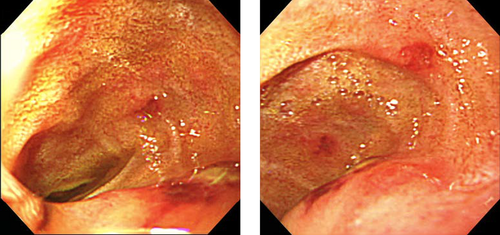
A 4-year-old boy was admitted to our hospital with severe abdominal pain and vomiting lasting for 3 days; no purpura was noted on admission. The patient was diagnosed with infectious enterocolitis and dehydration. After 3 days of hospitalization, blood tests showed hypoalbuminemia, hypokalemia, and an elevated d-dimer level, while the factor XIII level had fallen to 26%. Furthermore, ultrasonography (Fig. 1) and computed tomography (Fig. 2) revealed thickening of the duodenal and jejunal walls, while upper gastrointestinal endoscopy (Fig. 3) showed hemorrhagic-erosive lesions in the descending duodenum 1. The patient was, therefore, diagnosed with Henoch–Schönlein purpura without purpura, and corticosteroid therapy was initiated, which immediately improved his abdominal symptoms.
Conflict of Interest
None declared.