Immunologic characterization of patients with chronic mucocutaneous candidiasis disease
Key Clinical Message
Even if initial immunologic screen is normal, a high index of suspicion for immunodeficiency should guide the evaluation and management of patients with recurrent episodes of mucocutaneous candidiasis. Although rare, a diagnosis of chronic mucocutaneous disease should always be considered in order to improve their outcome.
1 INTRODUCTION
Candida albicans (C. albicans) is a yeast that naturally colonizes the skin, mucosa, gastrointestinal, and reproductive tract.1 In addition to its communalistic relationship with the host, Candida is also known to be a major cause of opportunistic infections. Depending on the defect of the host's immune system, Candida infection can range from benign localized to systemic life-threatening.2 When superficial Candida infections recur chronically, it is termed chronic mucocutaneous candidiasis syndrome (CMCS). CMCS is a heterogenous group of disorders of chronic superficial candidiasis accompanied by endocrine, immunologic, or autoimmune disorders.3 CMCS is well characterized in the literature. Various immunologic and genetic phenotypes have been subscribed to CMCS, including hyper-IgE syndrome (HIES) and autoimmune polyendocrinopathy candidiasis ectodermal dystrophy (APECED). Chronic mucocutaneous candidiasis disease (CMCD) is a relatively new classification described in the literature. Patients with this disorder present with recurrent superficial candidiasis as the major clinical phenotype, lacking any autoimmune, immunologic, or endocrine manifestations.4
The classification of CMCD has prompted further investigation into possible etiology, looking specifically at cytokine deficiencies. One cytokine pathway that has been linked to chronic mucocutaneous candidiasis (CMC) is the IL-12/interferon-gamma (IFN-γ) pathway. Patients with defects in this pathway lack autoimmune or endocrine manifestations, but present with colonization of mycobacterium and salmonella not seen in CMCD. Further studies looking into a specific defect that would result only in recurrent mucocutaneous candidiasis as seen in CMCD have led to a closer evaluation of T helper 17 (Th17) cells and their cytokines, specifically IL-17.5, 6
We report a case series of four patients diagnosed with CMCD. All four patients presented with recurrent superficial candidiasis in the absence of other clinical manifestations and were found to have deficiency in IL-17.
2 CASE PRESENTATION
2.1 Patient 1
A 10 y/o boy presented for recurrent superficial candidiasis, primarily affecting the oral cavity and genitalia area. As per his grandmother, his symptoms started in infancy. The patient was often treated with oral antifungals, which would normally resolve his infection. The patient's grandmother would recall initially having to treat him a few times a year. The need for treatment gradually increased to almost once a month in the last 2 years. Patient was usually treated with a five to seven day course of fluconazole or nystatin swish and swallow for oral candidiasis. While symptoms would resolve with treatment, patient would relapse soon after discontinuation of antifungal therapy. Despite the frequency, prophylaxis with oral antifungals was never considered. The patient suffered no other endocrine or autoimmune disorders, and despite recurrent candidiasis, was otherwise healthy. Physical examination was normal, except for oral thrush (Figure 1). Family history is only known of his mother, who has no history of immunodeficiency.

2.2 Patient 2
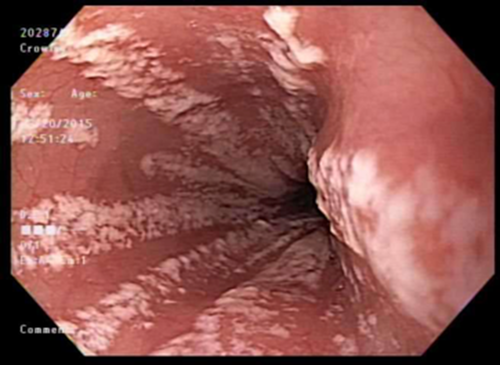
A 16 y/o female presented with a history of two episodes of esophageal candidiasis, confirmed by endoscopy and biopsy. She had no prior history of infections, antibiotics, or steroid use. Her first episode occurred two years prior to evaluation, with symptoms of dysphagia and chest discomfort which lasted for a few weeks prompting further evaluation with endoscopy. Patient was found to have esophageal candidiasis and treated with a fourteen day course of oral fluconazole with complete resolution of her symptoms. Patient remained healthy for two years until similar symptoms recurred. A repeat endoscopy was done which indicated similar findings as prior (Figure 2). Patient was again treated with a fourteen day course of oral fluconazole and referred for an immunology consultation. Initial workup revealed generally normal serum immunoglobulins, complete blood count (CBC), and metabolic panel. Her physical examination was unremarkable. This patient also had no other clinical abnormalities except for recurrent mucocutaneous candidiasis. Patient's family history was significant for her mother who is also suffering from recurrent superficial candidiasis. Prophylaxis was not considered for this patient since her mother wanted a more definitive diagnosis first.
2.3 Patient 3
A 52 y/o female, the mother of the 16 y/o patient, presented to our clinic for evaluation of recurrent vulvovaginal and cutaneous candidiasis. Numerous cultures were positive for yeast. Patient responded well to conventional antifungals, however, relapsed soon after completion of antifungal course. When asked when her symptoms first began, patient reported that it started in her early 20s, at least a few times a year where she would either use topical antifungals or oral fluconazole, normally prescribed by her gynecologist for the recommended duration of the treatment of vulvovaginal candidiasis. Patient would self-treat her cutaneous candidiasis, which she noticed mostly occurred during summer months or when she would perspire. Again, the patient was just treated symptomatically and was not given the option of prophylaxis therapy. Patient eventually sought further counsel with an immunologic evaluation after her daughter began suffering from esophageal candidiasis. Patient had no other history of immunodeficiency, autoimmunity, or endocrine abnormalities. Her family history is only significant for her daughter with recurrent esophageal candidiasis. Physical examination was unremarkable.
2.4 Patient 4
A 51 y/o female, presented with two episodes of esophageal candidiasis, confirmed by endoscopy and biopsy. The episodes were three years apart, with the first appearing when the patient was in her mid-40s. Patient was treated with a fourteen day course of oral fluconazole with complete resolution of her symptoms and was referred for immunologic consultation after her second episode. Prophylactic antifungal therapy was not discussed at that time. Her physical examination was remarkable for onychomycosis of her toenail and recurrent tinea versicolor. A thorough immunologic workup was done with the results pointing toward specific antibody deficiency in the setting of chronic sinusitis along with recurrent esophageal candidiasis. Patient had no significant family history of immunodeficiency.
3 RESULTS
All the patients with recurrent CMC were relatively healthy, except for patient 4 with her history of chronic sinusitis. None of the patients had a history of other opportunistic infections or serious infections such as pneumonias. A baseline CBC and metabolic panel were obtained and were normal in all patients. This was followed by laboratory tests including T/B/NK cell subset, serum immunoglobulins, plant lectins and Candida lymphocyte proliferation assays and delayed-type hypersensitivity skin testing (Table 1). All patients were found to have normal T/B/NK cells enumeration. Serum immunoglobulin levels were normal for all except for patient 4, where IgG was found to be slightly low at 616 mg/dL (654-1459 mg/dL). In addition, patient 4 was unable to produce adequate amounts of protective antibody titers to pneumococcal polysaccharide vaccine (PPSV23). With the clinical presentation of chronic sinusitis, patient four was diagnosed with specific antibody deficiency. Lymphocyte proliferation test to plant lectins was normal for all four patients, but nonreactive to Candida antigen. No other antigen-specific proliferation testing was done. Delayed-type hypersensitivity skin test to Candida was also nonreactive for all patients.
| Test (reference intervals) | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Reference interval |
|---|---|---|---|---|---|
| CBC (cell//mm3) | |||||
| White blood cell | 11 400 | 4100 | 5600 | 7100 | 6-12.5 |
| Absolute neutrophil count | 6000 | 1600 | 3500 | 5600 | 1.1-4.9 |
| Absolute lymphocyte count | 3900 | 2000 | 1600 | 1100 | 1.3-6 |
| Flow cytometry (%) | |||||
| CD3 | 71 | 84 | 72 | 81 | 60-76 |
| CD4 | 40 | 56 | 52 | 40 | 31-47 |
| CD8 | 25 | 25 | 18 | 35 | 18-35 |
| CD19 | 18 | 11 | 15 | 6 | 13-27 |
| CD16 | 9 | 3 | 11 | 11 | 4-17 |
| Immunoglobulins (mg/dL) | |||||
| IgG | 713 | 684 | 849.2 | 616 | 654-1459 |
| IgM | 106 | 78 | 342.0 | 96.8 | 61-135 |
| IgA | 48 | 67.3 | 77.3 | 101.9 | 77-260 |
| Delayed-typed hypersensitivity skin test (Candida) | Negative | Negative | Negative | Negative | |
| Lymphocyte proliferation test (Candida) | Nonreactive | Nonreactive | Nonreactive | Nonreactive | |
| Lymphocyte proliferation test | Normal | Normal | Normal | Normal | |
3.1 Cytokine assays
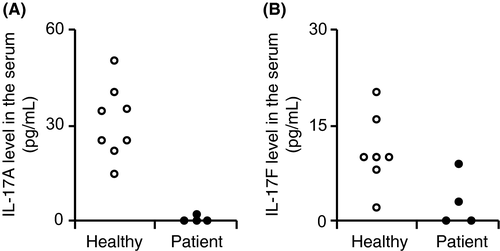
Serum from all four patients was matched with those of healthy controls. Serum cytokine profiles were examined using a bead-based multiplex assay (LEGENDplex™; Biolegend, San Diego, CA, USA) according to the manufacturer's guidelines. IL-17A was consistently deficient for all four patients (Figure 3). When compared to controls, IL-17A was completely absent for patients 1, 2, and 3 and significantly reduced for patient 4. IL-17F was more variable and found to be absent for patients 1 and 2, while levels were normal for patients 3 and 4. IFN-γ and IL-12 cytokines were also analyzed, though their results were more variable with both the patients and controls, with many of the controls having negligible amounts. Genetic testing was done to further clarify this.
3.2 Genetic testing
All four patients underwent genetic testing to evaluate for common genetic defects found in CMCS and CMCD. Evaluation for mutations in autoimmune regulator (AIRE), capsase recruitment domain-containing (CARD9), IL12B, IL12RB1, IL17F, IL17RA, IL17RC, RAR-related orphan receptor C (RORC), signal transducer and activator of transcription 1(STAT1), signal transducer and activator of transcription 3 (STAT3) was all negative. IL-12 was analyzed to help assess the IL12/IFN-γ pathway.
4 DISCUSSION AND CONCLUSION
We describe four patients who presented with isolated CMC. While the phenotypic presentation did vary, the defect in the IL-17 signaling pathway appears to be the common link. CMC was initially recognized as a group of heterogeneous disorders, under the classification of CMCS.7 Hyper-IgE syndrome, APECED, and CARD9 deficiency all present with CMC and therefore were classified under this category.7-13 Each one these disorders have a specific genetic mutation resulting in infectious, endocrine, and/or autoimmune manifestations. The decreased or absent level of IL-17 is the shared immunologic abnormality seen among them.
This patient cohort presented solely with CMC without any other clinical manifestations seen in CMCS. CMCD has been reported sparingly in the literature.4 Given its relatively new identification, much has yet to be discovered. While a defect in IL-17 seems to be a common link in CMCS, it also appears to be contributing to the pathophysiology of CMCD. IL-17 has been shown to be crucial in the recruitment of neutrophils and enhancement of β- defensins of keratinocytes against C. albicans, thus explaining a more isolated form of CMC.14-17 Similarly, IL-22 is another Th17 cytokine that contributes to mucosal immunity.14, 16 IL-22 has been linked to CMCD, with one study showing a decrease in the levels of both IL-17 and IL-22 in patients with CMC, as compared to healthy controls.17 However, our patient population did not express any abnormality in IL-22. Although a distinct and separate T helper cell subset has been shown to abundantly produce IL-22,18 the role of that cell subset remains to be elucidated in our patient cohort.
In an attempt to determine the specific defect in the signaling pathway of IL-17, we analyzed polarizing cytokines that promote survival of IL-17 cells and that are essential for the production of their transcription factors. Cytokines that promote differentiation of Th17 cells include IL-1β, IL-6, and transforming growth factor beta (TGF-β).19 All of the Th17 polarizing cytokines except for TGF-β were analyzed and were found to be normal in our patient cohort. IL-23, which is essential for maintenance of IL-17 and is also important in amplification of the inflammatory response, was also normal.20, 21 To assess the specific defect of IL-17, genetic analysis of IL-17, IL-17 receptors, the master regulator transcription factor of Th17, RORC, STAT1, and STAT3 was obtained.22 Genetic testing did not reveal any abnormality.
Our results demonstrated a defect in the IL-17 signaling pathway, with the exact mechanism yet to be determined. Cytokine analysis of all four patients revealed complete or near complete absence of IL-17 when compared to healthy controls. The abnormality of IL-17 may explain the specific defect in mounting immunity against C. albicans resulting in isolated CMC. This was further elucidated by a normal mitogen lymphocyte response in contrast to a nonreactive response to Candida.
Identifying the disease pathology and providing appropriate treatment is vital. Therapy is primarily with a member of the azole family, first line being fluconazole. Although the azoles provide symptomatic relief of cutaneous candidiasis, they are not the definitive treatment since it does not treat the underlying immunodeficiency. In addition, the increased use of antifungals has the potential to cause resistance, resulting in either higher doses or a need for change in medical therapy.23 Patients should also be made aware that treatment with azoles is not without side effects, hepatotoxicity being a primary concern.24 Targeted therapy is currently underway. In one case, a patient with known STAT1 mutation presenting with CMC was given granulocyte-colony stimulating factor (G-CSF) infusion with complete remission. However, in that case the genetic etiology was known, which is not the case for our patient cohort.25-27
There is a need for increase awareness in the medical community of CMCD in order to facilitate the early diagnosis and management of those patients. For all four patients, there was a significant delay before the diagnosis was made. Therefore, we would recommend that any physician treating recurrent candidiasis do an initial screen of the immune system with CBC, metabolic panel, immunoglobulins, and T/B/NK cell subsets, prior to follow-up with immunologic consultation. Recurrent candidiasis may be the first sign of an immunodeficiency and therefore warrants an evaluation. Our patient cohort was shown to have a defect in the IL-17 signaling pathway leading to the inability to mount an effective response against Candida. Knowing the etiology will allow physicians to better treat these patients. For example, prescribing inhaled corticosteroids or even oral steroids to patients with known IL-17 deficiency may prompt physician to simultaneously add prophylactic antifungals for this at risk group.
Chronic mucocutaneous candidiasis disease is a relatively new entity, where much is still unknown. Further studies are needed to determine the underlying genetic etiology, in order to provide targeted treatment and improved patient care.
ACKNOWLEDGMENTS
The authors would like to thank the patients and their family for their collaboration. They are also grateful to the nursing staff at Albany Medical Center for their assistance, especially Allisa Cronin. The authors declare no competing financial interests.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTION
KK, JC, and MP: contributed to the planning of this work and writing of this manuscript. QY and XS: collected the samples, analyzed the data, and revised the manuscript. All authors reviewed the manuscript.